Abstract
Chronic pain and chronic PTSD are often comorbid sequelae in patients who have experienced life-threatening experiences such as combat, assaults, or motor vehicle accidents, presenting lifelong challenges for patients and for medical management in all settings. This article briefly reviews four models for exploring the interrelationships of chronic pain and chronic PTSD. The article presents a longitudinal case study, documented over 10 years, of a patient with chronic back pain, and delayed-onset chronic PTSD related to sexual trauma experienced as a young adult. Data from the case study are examined for evidence in support of the chronic pain/chronic PTSD models. There is evidence to support all four models, with considerable evidence supporting the Mutual Maintenance Model (Sharp & Harvey, in Clinical Psychology Review 21(6): 857–77, 2001). Data show significant recovery over time from both conditions with improvements in function, work, and relationships, in response to Psychodynamic Therapy (PDT), Cognitive Behavioral Therapy (CBT), and hypnotic interventions, physical therapy, and pilates-based exercise. Notably, both chronic conditions were addressed simultaneously, with providers working collaboratively and sharing information through the patient. Emphasis is on non-pharmaceutical rehabilitative trauma-informed and patient-centered approaches to care.


Similar content being viewed by others
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, D.C.: Author.
American Psychological Association Guideline Development Panel for the Treatment of PTSD in Adults. (2017). Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Retrieved July 28, 20 from https://www.apa.org/ptsd-guideline/ptsd.pdf.
Anderson, T. E., Ellegard, H., Schiottz-Christensen, B., & Manniche, C. (2018). Somatic experiencing for patients with low back pain and comorbid posttraumatic stress disorder—protocol of a randomized controlled trial. BMC Complementary and Alternative Medicine, 18, 308–315.
Asmundson, G. J., & Katz, J. (2009). Understanding the co-occurrence of anxiety disorders and chronic pain: State-of-the-art. Depression and Anxiety, 26(10), 888–901.
Asmundson, G. J. G., Norton, G., Allerdings, M., Norton, P., & Larson, D. (1998). Post- traumatic stress disorder and work-related injury. Journal of Anxiety Disorders, 12, 57–69.
Beck, J. G., Coffey, S. F., Foy, D. W., Keane, T. M., & Blanchard, E. B. (2009). Group cognitive behavior therapy for chronic posttraumatic stress disorder: An initial randomized controlled trial. Behavior Therapy, 40, 82–92.
Bisson, J., & Andrew, M. (2005). Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Database Systematic Reviews, 2, CD003388.
Cantor, C. (2005). Evolution and posttraumatic stress: Disorders of vigilance and defence. Hove: Routledge.
Carmody, J., & Baer, R. A. (2009). How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology, 65(6), 627–638.
Chong, C. S., Tsunaka, M., Tsang, H. W., Chan, E. P., & Cheung, W. M. (2011). Effects of yoga on stress management in health adults: A systematic review. Alternative Therapies in Health and Medicine, 17(1), 32–38.
Clond, M. (2016). Emotional freedom techniques for anxiety: A systematic review with meta- analysis. Journal of Nervous and Mental Disease, 204(5), 388–395.
Daitch, C. (2007). Affect regulation toolbox: Practical and effective hypnotic interventions for the over-reactive client. New York: Norton.
Dauphin, V. B. (2020). A critique of the American psychological association clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Psychoanalytic Psychology, 37(2), 117–127.
Defrin, R., Ginzburg, K., Solomon, Z., Polad, E., Bloch, M., Govezensky, M., et al. (2008). Quantitative testing of pain perception in subjects with PTSD-implications for the mechanism of the coexistence between PTSD and chronic pain. Pain, 138, 450–459.
Dunleavy, K., & Kubo Slowik, A. (2012). Emergence of delayed posttraumatic stress disorder symptoms related to sexual trauma: Patient-centered and trauma-cognizant management by physical therapists. Physical Therapy, 92(2), 339–351.
Dunleavy, K., Kubo Slowik, A., Daitch, C., Elconin, L., Horowitz, R., Kestenberg, W., et al. (2014). When a white coat fear is really a white coat fear: Implications of sexual abuse by a physician for interactions with healthcare professionals. European Journal of Person Centered Healthcare, 2(3), 303–313.
Dunne, R. L., Kenardy, J., & Sterling, M. (2012). A randomized controlled trial of cognitive-behavioral therapy for the treatment of PTSD in the context of chronic whiplash. Clinical Journal of Pain, 28, 755–765.
Fishbain, D. A., Pulikal, A., Lewis, J. E., & Gao, J. (2017). Chronic pain types differ in thei reported prevalence of post-traumatic stress disorder (PTSD) and there is consistent evidence that chronic pain is associated with PTSD: An evidence-based structured systematic review. Pain Medicine, 18, 711–735.
Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35.
Foa, E., Riggs, D., Dancu, C., & Rothbaum, B. (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress., 6, 459–473.
Ford, J. D., Courtois, C. A., Steele, K., van der Hart, O., & Nijenhuis, E. R. S. (2005). Treatment of complex posttraumatic self-dysregulation. Journal of Traumatic Stress, 18(5), 437–447.
Gibson, C. (2012). Review of posttraumatic stress disorder and chronic pain: The path to integrated care. Journal of Rehabilitation Research and Development, 49(5), 753–776.
Goyal, M., Singh, S., Sibinga, E. M., Gould, N. F., Rowland-Seymour, A., Sharma, R., … Haythornthwaite, J. A. (2014). Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Internal Medicine, 174(3), 357-368
Greene, T., Neria, Y., & Gross, R. (2016). Prevalence, detection and correlates of PTSD in the primary care setting: A systematic review. Journal of Clinical Psychology in Medical Settings, 23, 160–180.
Hammond, D. C. (2010). Hypnosis in the treatment of anxiety- and stress-related disorders. Expert Review of Neurotherapeutics, 10(2), 263–273.
Herman, J. L. (1992). Trauma and recovery. New York: Basic Books.
Holbrook, T. L., Hoyt, D. B., Stein, M. B., & Sieber, W. J. (2002). Gender differences in long-term posttraumatic stress disorder outcomes after major trauma: Women are at higher risk of adverse outcomes than men. Journal of Trauma, 53(5), 882–888.
Keane, T. M., & Barlow, D. H. (2002). Posttraumatic stress disorder. Anxiety and its disorders (pp. 418–453). New York: Guilford Press.
Kearns, M. C., Kessler, K. J., Zatzick, D., & Rothbaum, B. (2012). Early interventions for PTSD: A review. Depression and Anxiety, 29, 833–842.
Kilpatrick, D., Edmunds, C., & Seymour, A. (1992). Rape in America: A report to the nation. Arlington, VA: National Victim Center.
Lebovits, A. (2007). Cognitive-behavioral approaches to chronic pain. Primary Psychiatry, 14(9), 48–50, 51–54.
Lynn, S. J., Malakataris, A., Condon, L., Maxwell, R., & Cleere, C. (2012). Post-traumatic stress disorder: Cognitive hypnotherapy, mindfulness, and acceptance-based treatment approaches. American Journal of Clinical Hypnosis, 54(4), 311–330.
McFarlane, A. C., Atchison, M., Rafalowicz, E., & Papay, P. (1994). Physical symptoms in posttraumatic stress disorder. Journal of Psychosomatic Research, 42, 607–617.
McGeary, D., Moore, M., Vriend, C. A., Peterson, A. L., & Gatchel, R. J. (2011). The evaluation and treatment of comorbid pain and PTSD in a military setting: An overview. Journal of Clinical Psychology in Medical Settings, 18(2), 155–168.
Merskey, H., & Bogduk, N. (1994). Classification of chronic pain: Descriptions of chronic pain syndromes and definitions of pain terms (2nd ed.). Seattle: IASP Press.
Moeller-Bertram, T., Keltner, J., & Strigo, I. A. (2011). Pain and post traumatic stress disorder—Review of clinical and experimental evidence. (2012). Neuropharmacology, 62, 586–597.
Norcross, J. C., & Wampold, B. E. (2019). Relationships and responsiveness in the psychological treatment of trauma: The tragedy of the APA clinical practice guideline. Psychotherapy, 56(3), 391–399.
Noyman-Veksler, G., Shalev, H., Brill, S., Rudich, Z., & Shahar, G. (2018). Chronic pain under missile attacks: Role of pain catastrophizing, media, and stress-related exposure. Psychological Trauma: Theory, Research, Practice and Policy, 16(4), 463–469.
Ogden, P., Minton, K., & Pain, C. (2006). Trauma and the body: A sensorimotor approach to psychotherapy. New York: Norton.
Otis, J. D., Keane, T. M., & Kerns, R. D. (2003). An examination of the relationship between chronic pain and post-traumatic stress disorder. Journal of Rehabilitation Research and Development, 40(5), 397–406.
Otis, J. D., Keane, T. M., Kerns, R. D., Monson, C., & Scioli, E. (2009). The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Medicine, 10(7), 1300–1311.
Paintain, E., & Cassidy, S. (2018). First-line therapy for post-traumatic stress disorder: A systematic review of cognitive behavioural therapy and psychodynamic approaches. Counselling and Psychotherapy Research, 18(3), 237–250.
Rothschild, B. (2011). Trauma essentials: The go-to guide. New York: Norton.
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., & Gray, S. H. (2008). Contributions of psychodynamic approaches to treatment of PTSD and trauma: A review of the empirical treatment and psychopathology literature. Psychiatry, 71(1), 13–34.
Sharp, T. J., & Harvey, A. G. (2001). Chronic pain and posttraumatic stress disorder: Mutual maintenance? Clinical Psychology Review, 21(6), 857–877.
Sijbrandij, M., Engelhard, I. M., de Vries, G.-J., Luitse, J. S. K., Carlier, I. V. E., Gersons, B. P. R., et al. (2013). The role of injury and trauma-related variables in the onset and course of symptoms of posttraumatic stress disorder. Journal of Clinical Psychology in Medical Settings, 20, 449–455.
Silveira, H., Moraes, H., Oliveira, N., Coutinho, E. S. F., Laks, J., & Deslandes, A. (2013). Physical exercise and clinically depressed patients: A systematic review and meta-analysis. Neuropsychobiology, 67(2), 61–68.
Simon, C. B., & Hicks, G. E. (2018). Paradigm shift in geriatric low back pain management: Integrating influences, experiences, and consequences. Physical Therapy, Suppl Special Issue on Nonpharmacological Management, 98(5), 434–446.
Tsur, N., Defrin, R., Lahav, Y., & Solomon, Z. (2018). The traumatized body: Long-term PTSD and its implications for the orientation towards bodily signals. Psychiatry Research, 261, 281–289.
Tunks, E. R., Crook, J., & Weir, R. (2008). Epidemiology of chronic pain with psychological comorbidity: Prevalence, risk, course, and prognosis. Canadian Journal of Psychiatry, 53(4), 224–234.
Valentine, K. E., Milling, L. S., Clark, L. J., & Moriarty, C. L. (2019). The efficacy of hypnosis as a treatment for anxiety: A meta-analysis. International Journal of Clinical and Experimental Hypnosis, 67(3), 336–363.
van der Kolk, B. (2014a). The body keeps the score. New York: Penguin.
van der Kolk, B. (2014b). Yoga as an adjunctive treatment for PTSD. Journal of Clinical Psychiatry, 75(6), 559–565.
van Emmerik, A., Kamphuis, J. H., & Emmelkamp, P. M. G. (2008). Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioral therapy or structured writing therapy: A randomized control trial. Psychotherapy and Psychosomatics, 77, 93–100.
Veltmeyer, M. D., McFarlane, A., Bryant, R. A., Mayo, T., Gordon, E., & Clark, C. R. (2006). Integrative assessment of brain function in PTSD: Brain stability and working memory. Journal of Integrative Neuroscience, 5(1), 123–138.
Vlaeyen, J. W., & Linton, S. J. (2000). Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain, 85(3), 317–332.
Wang, C.-W., Chan, C. H. Y., Ho, R. T. H., Chan, J. S. M., Ng, S.-M., & Chan, C. L. W. (2014). Managing stress and anxiety through qigong exercise in health adults: A systematic review and meta-analysis of randomized controlled trials. BMC Complementary and Alternative Medicine, 14, 1–9.
Whitson, H. E., Johnson, K. S., Sloane, R., Cigolle, C. T., Pieper, C. F., Landerman, L., et al. (2016). Identifying patterns of multimorbidity in older Americans: Application of latent class analysis. Journal of the American Geriatric Society, 32, 898–906.
Wilson, L. C., & Jones, R. T. (2010). Therapists as trauma survivors: A case study detailing cognitive processing therapy for rape victims with a psychology graduate student. Clinical Case Studies, 9(6), 442–456.
www.ptsd.va.gov/understand/common/common_adults.asp. Accessed 3 Sept 2020.
Acknowledgements
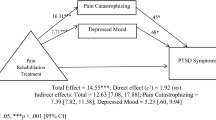
The authors gratefully acknowledge the cooperation and assistance of Carolyn Daitch, Ph.D., Lisa Elconin, M.D., Kristen Robertson, D.P.T, Amy Kubo Slowik, P.T., and Natalie Kay Wicks, M.S.W. The authors also thank Dr. Cheryl Munday and four anonymous reviewers whose comments on earlier drafts were very helpful. The data presented in Fig. 1 expand on data published in Physical Therapy in 2012. Additional longitudinal data are presented here, and the data are used for a different analysis. The corresponding author for this paper is also the patient; she gives her full, informed consent to have identifying information presented in this paper.
Funding
The authors received no funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Carol Cronin Weisfeld and Kim Dunleavy declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weisfeld, C.C., Dunleavy, K. Strategies for Managing Chronic Pain, Chronic PTSD, and Comorbidities: Reflections on a Case Study Documented over Ten Years. J Clin Psychol Med Settings 28, 78–89 (2021). https://doi.org/10.1007/s10880-020-09741-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-020-09741-5