Abstract
Superior vena cava collapsibility index (SVC-CI) and stroke volume variation (SVV) have been shown to predict fluid responsiveness. SVC-CI has been validated only with conventional transoesophageal echocardiography (TEE) in the SVC long axis, on the basis of SVC diameter variations, but not in the SVC short axis or by SVC area variations. SVV was not previously tested in vascular surgery patients. Forty consecutive adult patients undergoing open major vascular surgical procedures received 266 intraoperative volume loading tests (VLTs), with 500 ml of gelatine over 10 min. The hSVC-CI was measured using a miniaturized transoesophageal echocardiography probe (hTEE). The SVV and cardiac index (CI) were measured using Vigileo-FloTrac technology. VLTs were considered ‘positive’ (≥ 11% increase in CI) or ‘negative’ (< 11% increase in CI). We compared SVV and hSVC-CI measurements in the SVC short axis to predict fluid responsiveness. Areas under the receiver operating characteristic curves for hSVC-CI and SVV were not significantly different (P = 0.56), and both showed good predictivity at values of 0.92 (P < 0.001) and 0.89 (P < 0.001), respectively. The cutoff values for hSVC-CI and SVV were 37% (sensitivity 90%, specificity of 83%) and 15% (sensitivity 78%, specificity of 100%), respectively. Our study validated the value of the SVC-CI measured as area variations in the SVC short axis to predict fluid responsiveness in anesthetized patients. An hTEE probe was used to monitor and measure the hSVC-CI but conventional TEE may also offer this new dynamic parameter. In our cohort of significant preoperative hypovolemic patients undergoing major open vascular surgery, hSVC-CI and SVV cutoff values of 37% and 15%, respectively, predicted fluid responsiveness with good accuracy.
Similar content being viewed by others
1 Introduction
Tailoring the volume of fluid administration remains the cornerstone of fluid resuscitation and haemodynamic status optimization in surgery and intensive care. Older static haemodynamic parameters, such as central venous pressure (CVP) and pulmonary capillary wedge pressure are considered inferior to newer dynamic (functional) parameters that can be used to assess fluid status and predict fluid responsiveness in sedated, paralyzed, and ventilated patients [1,2,3,4]. Recent guidelines and expert consensus in haemodynamic management of critically ill or high-risk patients also favour the use of dynamic over static parameters whenever possible [5,6,7,8]. The ‘era’ of dynamic parameters started more than 30 years ago when the systolic pressure variation (SPV) and its delta down (∆d) component were validated [9, 10]; however, other dynamic parameters, namely, stroke volume variation (SVV) and pulse pressure variation (PPV) have gained the greatest popularity [11, 12]. Transthoracic (TTE) and transoesophageal (TEE) echocardiography can also be used to assess volume responsiveness during mechanical ventilation via dynamic parameter measurements derived from variations in either aortic flow or inferior vena cava (IVC) flow on TTE or superior vena cava (SVC) diameters via TEE. Only four studies have focused on the SVC collapsibility index (SVC-CI) measured via TEE. These studies found that SVC-CI was an excellent predictor of volume responsiveness in sedated, sinus rhythm, paralyzed and volume-controlled mechanically ventilated patients [13, 14] but only a pretty good predictor whenever one or more of the above conditions are not met [15, 16]. Although SVC-CI is an interesting parameter of fluid responsiveness, the lack of continuity and physicians with experience in performing serial conventional TEE exams makes this approach inaccessible in many hospitals worldwide [16,17,18]. These deficiencies can be obviated through the use of a new miniaturized (5.5-mm in diameter) transoesophageal, monoplane echocardiographic detachable probe (hTEE), which, once connected to a dedicated ultrasound system, can monitor cardiac function and haemodynamic status continuously for up to 72 h (ClariTEE™, ImaCor Inc., Garden City, NY, USA). The hTEE probe provides continuous direct visualization of three views of the heart including: the trans-gastric short-axis, the mid-oesophageal four-chamber view, and the mid-oesophageal ascending aortic short-axis (ME-AA-SAX), the last allowing visualization of the SVC in its short-axis. Currently, this new technology is used mainly in critically ill and post cardiac surgery patients as a qualitative alternative to other methods. It has shown promising results that include a very short training period (only 6 h) [19] and a direct therapeutic impact in 50–66% of studied patients [20, 21]. The ME-AA-SAX view is suitable for calculating the SVC-CI based on either the SVC diameter or area variations under mechanical ventilation. Until now, the SVC-CI was studied and validated as a predictor of fluid responsiveness based only on the SVC long-axis view observed during conventional TEE, which focused on the mid-oesophageal bicaval (ME-BIC) view [13,14,15,16]. SVC-CI measurements were obtained in the M-mode on the basis of SVC diameter variations but never on the basis of SVC area variations [13,14,15,16]. Importantly, the ME-BIC and ME-AA-SAX views do not interrogate the SVC at the same anatomical level, and therefore, the SVC measurements obtained in the two views are not superimposable. To date, neither the SVC-CI measurement in the SVC short-axis view nor the measurement of SVC-CI using hTEE (hSVC-CI) have been tested against any other dynamic parameter to predict fluid responsiveness. Yet, despite a lack of evidence, some authors have recommended an SVC-CI cutoff value of > 35% [19] or > 30% [22] measured in the SVC short-axis view on hTEE as a safe threshold for fluid administration to restore haemodynamic stability. Therefore, we investigated hSVC-CI versus SVV measurements to predict fluid responsiveness in patients undergoing open major vascular surgical procedures.
2 Methods
This prospective clinical cohort study was conducted in the Anaesthesia and Intensive Care Departments of a tertiary care teaching hospital. We obtained local institutional ethics committee approval (Chairperson: Professor Daniela Filipescu, No. 17290 on 20 August 2013) and written patient consent.
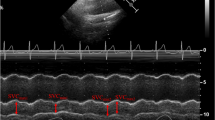
Forty-five consecutive patients undergoing scheduled open major vascular surgeries, including open abdominal aortic aneurysm or Leriche syndrome repair procedures, from September 2013 to November 2016 were recruited for the study. We excluded patients who met any of the following criteria: age younger than 18 years, with suspected pregnancy, non-sinus cardiac rhythm, weight > 120 kg or < 60 kg, left ventricular ejection fraction ≤ 30%, right ventricular dysfunction (right ventricular ejection fraction ≤ 30% on preoperative TTE), significant pulmonary hypertension [23] (mean arterial pulmonary pressure ≥ 35 mmHg on preoperative TTE), preoperative vasodilator, vasoconstrictor, or inotrope treatments, renal failure requiring haemo- or peritoneal dialysis, haemoglobin < 8 g dl−1, significant aortic regurgitation [24] and a history of oesophageal or gastrointestinal disease precluding TEE. After premedication with intramuscular morphine at a dose of 0.1 mg kg−1, all patients were transferred to the operating room and standard non-invasive monitoring was initiated. Two peripheral venous lines and a radial artery catheter were inserted. General anaesthesia was induced with fentanyl 7 mcg kg−1, midazolam 0.1 mg kg−1 or Propofol 1.5 mg kg−1, and atracurium 0.6 mg kg−1 and maintained with sevoflurane (for minimum alveolar concentration 0.8–1.2 and a bispectral index 40–60), fentanyl, and atracurium as needed for ventilator-adaptation maintenance. After endotracheal intubation, controlled mechanical ventilation was instituted in all patients according to the following parameters: FIO2 0.6, tidal volume 8 ml kg−1, frequency of 12 cycles min.−1, peak inspiratory pressure < 25 cm H2O, I:E ratio 1:2, and a positive end-expiratory pressure of 5 cm H2O to maintain the end tidal CO2 at 30–35 mmHg. These mechanical ventilation parameters were unchanged throughout the surgery. The arterial line was connected to a FloTrac sensor (Edwards Lifesciences, Irvine, CA, USA) and a Vigileo monitor (Edwards Lifesciences, Irvine, CA, USA; software version 4.02). Eventually a three-way central venous catheter was inserted into an internal jugular vein, and a urinary catheter and an hTEE probe (ClariTEE™, ImaCor Inc., Garden City, NY, USA) coupled to a ZURA-EVO 1™ console (ImaCor Inc., Garden City, NY, USA) were inserted. The FloTrac and venous transducers were zeroed to the level of the left atrium and the Vigileo monitor was set to measure the cardiac index (CI) and SVV at 10-s intervals on the basis of a proprietary algorithm described in detail elsewhere [25]. The hTEE probe was fixed in the ME-AA-SAX view. Once the patient was monitored and stable, maintenance fluid, either 5% dextrose or Ringer’s lactate solution (at the discretion of the treating physician) at 1 ml kg h−1 was administered throughout the intraoperative period. Hypothermia was minimized using forced-air warming blankets. Intraoperatively, standardized volume loading tests (VLT) with 500 ml of a gelatine solution (Gelofusine 4 g/100 ml, B. Braun, Germany) were administered over 10 min any time one or any combination of the following circumstances were present: systolic arterial pressure (SAP) decreased ≥ 40 mmHg from baseline, SAP < 90 mmHg, mean arterial pressure (MAP) decreased ˃20% from baseline, MAP < 60 mmHg, tachycardia > 100 beats min−1, hyperlactatemia > 2 mmol l−1, urine output < 0.5 ml kg−1 h−1 for 60 min, or estimated blood loss ≥ 500 ml. Boluses of ephedrine or norepinephrine were given whenever the treating physician deemed necessary but all the VLTs preceded by those boluses were excluded from the study [26]. The following haemodynamic parameters were studied before and after each VLT: heart rate (HR), SAP, MAP, CI, CVP, SVV, and hSVC-CI. Aside from the above-described VLTs, any other fluids, red blood cells (transfused to maintain the haemoglobin > 8 g dl−1), or blood products administered between the VLTs were not counted in the VLTs. One senior anaesthesiologist blinded to the SVV and hSVC-CI measurements managed the intraoperative status of the patients (standardized VLT administrations included). Another anaesthesiologist collected the invasive haemodynamic data (HR, SAP, MAP, CI, CVP, and SVV) during 12-s periods before and after the VLTs were administered. A third blinded anaesthesiologist was dedicated to maintaining the best SVC view and recording two consecutive cine-loops of the ME-AA-SAX views (each for 6 s) when the first anaesthesiologist announced that either a VLT condition was present or the end of each VLT. All invasive haemodynamic data were also recorded in our patient data management system (HIM-GmbH, Bad Homburg, Germany) for review and analysis. The best SVC view was defined as the first SVC short axis view visualised during the gradual withdrawal of the monoplane probe from the four chambers view. The hSVC-CI was calculated offline using the formula:
The maximum and minimum areas were measured offline by tracing the SVC borders. The average hSVC-CI from two consecutive cine-loops was used for statistical purposes. CI increases induced by volume expansion were used to classify each VLT as ‘positive’ (+) (≥ 11% increase in CI) or ‘negative’ (−) (< 11% increase in CI) for further analysis.
2.1 Statistics
Categorical data are expressed as numbers (proportions). Haemodynamic continuous variables hSVC-CI, SVV, and CVP were studied and tested for normality using the Shapiro–Wilk test. For normally distributed data Student t test for paired samples was used. For non-normally distributed data, we used the Wilcoxon signed rank test. Results are expressed as means \(\pm\) standard deviations (SD), medians (inter-quartile range (IQR) 25–75%), or means (95% confidence interval, (CI)), as appropriate. To assess the ability of the variables to discriminate between a +VLT and −VLT, the value of each haemodynamic variable measured before the VLT that led to a +VLT was compared to the VLT measured before a −VLT using the Mann–Whitney U-test. Receiver operating characteristic curves (ROC) were constructed to test the ability of the variables to predict fluid responsiveness. Areas under the ROC curves (AUC) were compared using DeLong’s test [27]. A difference between two AUCs was considered statistically significant when the P-value of DeLong’s test was < 0.05. Sensitivity and specificity were also calculated. The optimal cutoff for each variable was estimated by maximizing the Youden index (sensitivity + specificity − 1). We assumed that hSVC-CI would be clinically relevant if the 95% CI of its AUC was more than 0.75, corresponding to an AUC of a good clinical tool, as reported by Ray [28]. Accordingly, we determined that 39 patients had to be included. The statistical analysis was performed using MedCalc (MedCalc, Inc., Mariakerke, Belgium). For all comparisons, P < 0.05 was considered significant.
3 Results
We enrolled 45 consecutive patients; however, 5 were excluded because of inadequate SVC image quality on hTEE. We studied 40 patients with the mean weight of 80 ± 11 kg (range: 62–99 kg) undergoing open major vascular surgery: 22 with abdominal aortic aneurysms and 18 with Leriche syndrome, all requiring repair. Each VLT of 500 ml given over 10 min represented a loading dose between a maximum of 8 ml kg−1 and a minimum of 5 ml kg−1.
Aya and co-workers [29] demonstrated that a fluid loading dose of 4 ml kg−1 is enough to increases CI ≥ 10%, and reliably detects responders and nonresponders.
Thirty-one patients were men and nine were women, with an overall mean age of 63 ± 9 years (men: 65 ± 9, women: 63 ± 11). A total of 289 VLTs were administered but twenty-three VLTs preceded by vasopressor administration, were excluded. For the 266 remaining VLTs, the median number of VLTs per patient was 7 (range 3–8). The mean estimated blood loss was 1225 ml ± 305 ml. No patient received inotropic therapy during the study. All patients survived and no complication linked to hTEE usage has been highlighted. Table 1 summarizes the results of the haemodynamic measurements at baseline and after the VLTs. Of 266 VLTs studied, 243 (91%) were positive (≥ 11% increase in CI) and only 23 (9%) were negative (< 11% increase in CI) (Fig. 1). Among the 266 VLTs studied and the 243 +VLTs, we found a significant decrease from baseline to post VLT administration in both hSVC-CI and SVV. This was accompanied by a significant increase in CVP and CI (Table 1). Among the 23 negative VLTs the hSVC-CI, SVV, CVP and CI values did not change (Table 1). A comparison of variables measured at baseline between +VLTs and −VLTs showed significantly higher hSVC-CI (0.44 [0.39 to 0.51] vs. 0.35 [0.32 to 0.36] % P < 0.0001) and SVV (18.0 [16.0 to 21.0] vs. 13.0 [12.0 to 14.0] %; P < 0.0001) values and significantly lower CI (2.0 [1.8 to 2.2] vs. 2.5 [2.1 to 2.9] l min −1 m−2; P < 0.0001) values in +VLTs than in –VLTs (Table 1. Also, CVP values (10.0 [7.0 to 13.0] vs. 11.0 [6.0 to 14.0] mm Hg; P = 0.63) did not show any statistically significant difference between the +VLTs and –VLT groups (Table 1). Discrimination between +VLTs and −VLTs according to haemodynamic parameters was then evaluated by constructing ROC curves (Fig. 2). In the ROC curve analysis, both hSVC-CI and SVV showed good predictivity, with AUCs values of 0.92 (95% CI 0.88 to 0.95; P < 0.001) and 0.89 (95% CI 0.85 to 0.93; P < 0.001), respectively. No significant difference was found between the two AUCs (P = 0.56). The AUC for CVP (0.53, 95% CI 0.46 to 0.59; P = 0.69) was significantly lower than that for hSVC-CI and SVV, thus demonstrating poor predictivity for this parameter. The AUC for CVP was not significantly different from 0.5. Based on the Youden test, a baseline hSVC-CI cutoff value > 37% predicted fluid responsiveness with a sensitivity of 90% (95% CI: 86 to 94) and specificity of 83% (95% CI: 61 to 95). Baseline SVV cutoff values > 15% predicted fluid responsiveness with a sensitivity of 78% (95% CI: 72 to 82) and specificity of 100% (95% CI: 85 to 100).
Receiver operating characteristic curves describing the ability of hSVC-CI, SVV, and CVP to predict a fluid challenge-induced increase in cardiac index of at least 11%. hSVC-CI superior vena cava collapsibility measured with a miniaturized transoesophageal echocardiography probe, SVV stroke volume variation, CVP central venous pressure
4 Discussion
To the best of our knowledge, this is the first study investigating the value of SVC-CI measured in the short-axis view and the feasibility of hSVC-CI measurements using a miniaturized monoplane transoesophageal probe (hTEE) to predict fluid responsiveness. We found that hTEE provided adequate images of SVC in the short-axis view, allowing good quality cine-loop recordings and subsequent offline analyses in 89% of our initially enrolled patients. We also proved that hTEE technology is suitable for accurate measurements of the SVC-CI in anaesthetized patients. In our study, an hSVC-CI threshold of 37% predicted fluid responsiveness with a sensitivity of 90% and specificity of 83%. An SVV threshold of 15% predicted fluid responsiveness with lower sensitivity (78%) than hSVC-CI, but with excellent specificity (100%). To date, all other studies published on SVC-CI and fluid responsiveness have used SVC diameter variations measured in the SVC long-axis view (ME-BIC) to calculate SVC-CI via conventional TEE [13,14,15,16].
Variations in SVC size under mechanical ventilation were first observed by Vieillard-Baron and co-workers [30]. The same authors studied 66 mechanically ventilated patients in septic shock. The AUC for SVC-CI was 0.99. A threshold SVC-CI of 36% discriminated between responders (CI increase ≥ 11% induced by volume expansion) and non-responders (CI increase < 11%) with a sensitivity of 90% and specificity of 100% [13].
Charbonneau and co-workers [15] examined 44 ventilated patients in septic shock and demonstrated an AUC of 0.74. They found that a SVC-CI cutoff value > 29% predicted fluid responsiveness with 54% sensitivity and 94% specificity.
In another study of 540 ventilated patients with all-cause circulatory failure, an increase in aortic velocity time integral (Ao-VTI) ≥ 10% during a passive leg raising manoeuvre was used as a discriminator for fluid responsiveness. Vignon and Vieillard-Baron [16] determined the diagnostic accuracy of SVC-CI for predicting fluid responsiveness compared with the maximal Doppler velocity in the left ventricular outflow tract (ΔVmaxAo), inferior vena cava distensibility index (IVC-DI), and PPV. They found that the AUCs were similar for ΔVmaxAo (0.75) and SVC-CI (0.75) and both were significantly greater than those for PPV (0.67) and IVC-DI (0.63). The best cutoff values were ≥ 21% for SVC-CI (61% sensitivity, 84% specificity) and ≥ 10% for ΔVmaxAo (79% sensitivity, 64% specificity).
The discrepancies observed between the above two studies [15, 16] and other validation studies [13, 14] in terms of poorer AUCs and SVC-CI sensitivities can be explained by the heterogeneity of the studied populations. Hrishi [14] compared SVC-CI, Δd, and Ao-VTI variations to predict fluid responsiveness in 15 anaesthetized stable neurosurgical patients. They found that SVC-CI values > 38% (long-axis) were excellent predictors of fluid responsiveness (100% sensitivity, 95% specificity), followed by Ao-VTI variations > 20% (100% sensitivity, 90% specificity), and Δd > 5 mm Hg (100% sensitivity, 90% specificity).
Our results concerning the hSVC-CI threshold value (37%), sensitivity (90%), and specificity (83%) are closer to those of studies conducted in strictly anaesthetized, sedated, and paralyzed patients [13, 14] (as our patients were) than those of studies conducted in a heterogeneous population [15, 16]. Similar to that in Vieillard-Baron’s report [13], a CI increase ≥ 11% was used to discriminate between +VLTs and –VLTs; however, we calculated hSVC-CI on the basis of SVC variations studied in the short-axis view and not on the basis of variations studied in the long-axis view (Fig. 3). Moreover, we calculated hSVC-CI based on SVC area variations, not diameter variations. We considered that measuring SVC-CI in the short-axis view (ME-AA-SAX) based on its area variations (using either hTEE or conventional TEE) could confer advantages and disadvantages, both anatomical and physiological.
The TEE probes do not interrogate the superior vena cava at the same level in ME-AA-SAX view and in ME-BIC view. The A-B distance is 1–2 cm. On the right side of the figure: TEE or hTEE schematic image of ME-AA-SAX view (top) and TEE schematic image of ME-BIC view (bottom). TEE transoesophageal echocardiography, hTEE miniaturized transoesophageal echocardiography, ME-AA-SAX mid-oesophageal ascending aortic short-axis, ME-BIC mid-oesophageal bicaval, A tip position of the TEE probe in ME-BIC view, B tip position of the TEE probe in ME-AA-SAX view, SVC superior vena cava, RPA right pulmonary artery, MPA main pulmonary artery, Asc.Ao ascending aorta, RA right atrium, LA left atrium, IVC inferior vena cava
Obtaining reliable measurements of SVC-CI in the long-axis view (ME-BIC) via conventional TEE requires accurate measurements of diameters using an exact alignment of the M mode beam to 90°. The potential inaccuracies of the ME-BIC approach related to possible paramedian cuts of the vessel make the ME-AA-SAX approach more advantageous when measuring the SVC-CI diameters. However, in reality, the SVC does not have a perfectly cylindrical shape and is often irregularly shaped on cross-sectional images. The SVC demonstrates an ellipsoid shape as seen on TEE or hTEE in ME-AA-SAX views [31]. In daily practice it is often difficult to select the real ‘maximum’ or ‘minimum’ diameter according to the irregularly shaped SVC even in the short-axis view (ME-AA-SAX). Therefore, we presumed that SVC-CI measurements based on SVC area variations in the short-axis view may reflect more accurate amplitudes of SVC changes under mechanical ventilation. This could be another advantage to the method.
From the physiological point of view, during mechanical ventilation, intermittent positive airway pressure periodically and temporarily increases the pleural pressure and thereby causes cyclic changes mainly to preload and, to a lesser extent, afterload. A recent study demonstrated that about 67% of airway pressure changes during mechanical inspiration are transmitted to the pleura, and only 33% to the pericardium and SVC, resulting in a decrease in transmural pressure in the SVC and an unchanged transmural pressure in the right atrium [32]. From the anatomical point of view, the SVC has a proximal (extrapericardial) section and a distal (intrapericardial) one. The mean SVC length is about 7.1 ± 1.5 cm (range 4.4–9 cm.). Half of the SVC lies within the pericardium and half lies outside [33,34,35,36,37]. The SVC image in long-axis view (ME-BIC) is the distal segment. This part always belongs to the intrapericardial section of the SVC. Depending on the patient’s anatomy, if the patient has a very short SVC (about 4–4.5 cm.), the ME-AA-SAX view may show images of the extrapericardial part of the SVC. In any case, the SVC images offered by ME-AA-SAX (short-axis view) are not seen at the same anatomical level as the ME-BIC (long-axis view) but are slightly (1–2 cm.) higher (Fig. 3). Accordingly, the SVC diameters and the SVC-CI values measured in ME-BIC and in ME-AA-SAX views, may not be interchangeable.
The main limitations of our study are: the lack of a standardised fluid bolus given on a ml kg−1 basis, the high amount of fluids given and the relatively small number of patients. Regarding the VLTs of 500 ml administered to all our patients regardless of their weight, we have to underline that all our patients received more than 4 ml kg−1 which represents the minimum loading dose able to increase CI ≥ 10%, and discriminate between responders and nonresponders [29]. Giving more fluid than is needed to increase the CI in a significant manner (≥ 10–11%) may result either in an insignificant increase or even in a decrease in CI only if the patient was already either on the final ascendant or on the flat part of Starling curve at the beginning of the VLT. Our cohort of patients consisted in significant preoperative hypovolemic patients and the above described effect is unlikely to significantly impact the results of our study.
The high mean volume given as opposed to a mean blood loss of 1.2 L may be due both to the patient’s conditions (scheduled, fasting, hypovolemic) and the overzealous desire to promptly respond to the occurrence of any protocol circumstances that requires a VLT.
In our study, we also measured SVV, which has been validated in various patient populations (except those undergoing open major vascular surgery) in the operating room and the ICU, with various threshold values between 10 and 15% [38, 39]. Regarding SVV values measured using FloTrac technology, since its introduction, the performance of this uncalibrated technique has improved, particularly under hypo- and normodynamic conditions [40]. The device has been proven to accurately track changes in cardiac output when preload changes [41]. On the other hand, current evidence still shows conflicting results on the FloTrac technology: the system still lacks optimal accuracy and trending ability in cardiac and vascular surgery, and the discrepancy in cardiac output measurement depends on the peripheral vascular tone [42, 43]. The FloTrac 4-th generation software used in our study is both more accurate and more precise even when phenylephrine in low-moderate doses are administered [44]. However, no study was performed with ephedrine or norepinephrine and thus we excluded from the study all the VLTs preceded by the administration of those two drugs.
The only study (11 patients) of mixed gastrointestinal and vascular patients using Flo-Trac showed that an SVV threshold of 12% was a good predictor of fluid responsiveness (sensitivity: 0.86; specificity: 0.91) [45]. Nevertheless, 10% and 13% SVV threshold values, based on FloTrac technology, were used in randomized control trials on the effects of goal-directed therapy in high-risk vascular patients [46, 47]. Both of these studies reported that SVV-guided fluid optimization during open major vascular surgery was associated with better haemodynamic stability and fewer complications; however, there was no decrease in mortality. In our study, an SVV threshold value > 15% predicted fluid responsiveness with excellent specificity (100%) but only 78% sensitivity.
5 Conclusions
Our study validated the value of the SVC-CI measured as area variations in the SVC short axis view, to predict fluid responsiveness in anesthetized patients. We measured this new dynamic parameter with a miniaturized transoesophageal monoplane continuous echocardiography probe but the SVC-CI measured in ME-AA-SAX view may also be extended to the use of conventional TEE. The current study showed that for this cohort of significant preoperative hypovolemic patients underwent major open vascular surgery an hSVC-CI cutoff value of 37% and a SVV cutoff of 15% predicted fluid responsiveness with good accuracy.
References
Diebel L, Wilson RF, Heins J, et al. End-diastolic volume versus pulmonary artery wedge pressure in evaluating cardiac preload in trauma patients. J Trauma. 1994;37:950–5.
Preisman S, Kogan S, Berkenstadt H, et al. Predicting fluid responsiveness in patients undergoing cardiac surgery: functional haemodynamic parameters including the Respiratory Systolic Variation Test and static preload indicator. Br J Anaesth. 2005;95:746–55.
Osman D, Ridel C, Ray P, et al. Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med. 2007;35:64–8.
Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41:1774–81.
Cecconi M, De Backer D, Antonelli M, et al. Consensus on circulatory shock and hemodynamic monitoring Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1795–815.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–77.
Vincent JL, Rhodes A, Perel A, et al. Clinical review: update on hemodynamic monitoring—a consensus of 16. Crit Care. 2011;15:229.
Vincent JL, Pelosi P, Pearse R, et al. Perioperative cardiovascular monitoring of high-risk patients: a consensus of 12. Crit Care. 2015;19:224.
Perel A, Pizov R, Cotev S. Systolic blood pressure variation is a sensitive indicator of hypovolemia in ventilated dogs subjected to graded hemorrhage. Anesthesiology. 1987;67:498–502.
Beaussier M, Coriat P, Perel A, et al. Determinants of systolic pressure variation in patients ventilated after vascular surgery. J Cardiothorac Vasc Anesth. 1995;9:547–51.
Cannesson M, Pestel G, Ricks C, et al. Hemodynamic monitoring and management in patients undergoing high risk surgery: a survey among North American and European anesthesiologists. Crit Care. 2011;15:R197.
Cecconi M, Hofer C, Teboul JL, et al. Fluid challenges in intensive care: the FENICE study: a global inception cohort study. Intensive Care Med. 2015;41:1529–37.
Vieillard-Baron A, Chergui K, Rabiller A, et al. Superior vena cava collapsibility as a gauge of volume status in ventilated septic patients. Intensive Care Med. 2004;30:1734–9.
Hrishi AP, Sethuraman M, Menon G. Quest for the Holy Grail: assessment of echo-derived dynamic parameters as predictors of fluid responsiveness in patients with acute aneurysmal subarachnoid hemorrhage. Ann Card Anaesth. 2018;21:243–8.
Charbonneau M, Riu B, Faron M, et al. Predicting preload responsiveness using simultaneous recordings of inferior and superior vena cavae diameters. Crit Care. 2014;18:473.
Vignon P, Repessé X, Bégot E, et al. Comparison of echocardiographic indices used to predict fluid responsiveness in ventilated patients. Am J Respir Crit Care Med. 2017;195:1022–32.
Charron C, Caille V, Jardin F, et al. Echocardiographic measurement of fluid responsiveness. Curr Opin Crit Care. 2006;12:249–54.
Levitov A, Marik PE. Echocardiographic assessment of preload responsiveness in critically ill patients. Cardiol Res Pract. 2012;2012:819696. https://doi.org/10.1155/2012/819696.
Cioccari L, Baur HR, Berger D, et al. Hemodynamic assessment of critically ill patients using a miniaturized transesophageal echocardiography probe. Crit Care. 2013;17:R121.
Vieillard-Baron A, Slama M, Mayo P, et al. A pilot study on safety and clinical utility of a single-use 72-hour indwelling transesophageal echocardiography probe. Intensive Care Med. 2013;39:629–35.
Maltais S, Costello WT, Billings FT 4th, et al. Episodic monoplane transesophageal echocardiography impacts postoperative management of the cardiac surgery patient. J Cardiothorac Vasc Anesth. 2013;27:665–9.
Fletcher N, Geisen M, Meeran H, et al. Initial clinical experience with a miniaturized transesophageal echocardiography probe in a cardiac intensive care unit. J Cardiothorac Vasc Anesth. 2015;29:582–7.
von Ballmoos MW, Takala J, Roeck M, et al. Pulse-pressure variation and hemodynamic response in patients with elevated pulmonary artery pressure: a clinical study. Crit Care. 2010;14:R111.
Maeda T, Yoshitani K, Inatomi Y, et al. Inaccuracy of the FloTrac/Vigileo™ system in patients with low cardiac index. J Cardiothorac Vasc Anesth. 2014;28:1521–6.
Manecke GR. Edwards FloTrac sensor and Vigileo monitor: easy, accurate, reliable cardiac output assessment using the arterial pulse wave. Expert Rev Med Devices. 2005;2:523–7.
Thiele RH, Bartels K, Gan TJ. Cardiac output monitoring: a contemporary assessment and review. Crit Care Med. 2015;43:177–85.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Ray P, Le Manach Y, Riou B, et al. Statistical evaluation of a biomarker. Anesthesiology. 2010;112:1023–40.
Aya HD, Rhodes A, Chis Ster I, et al. Hemodynamic effect of different doses of fluids for a fluid challenge: a quasi-randomized controlled study. Crit Care Med. 2017;45:161–8.
Vieillard-Baron A, Augarde R, Prin S, et al. Influence of superior vena caval zone condition on cyclic changes in right ventricular outflow during respiratory support. Anesthesiology. 2001;95:1083–8.
Lin FY, Devereux RB, Roman MJ, et al. The right sided great vessels by cardiac multidetector computed tomography: normative reference values among healthy adults free of cardiopulmonary disease, hypertension, and obesity. Acad Radiol. 2009;16:981–7.
Lansdorp B, Hofhuizen C, van Lavieren M, et al. Mechanical ventilation induced intrathoracic pressure distribution and heart-lung interactions. Crit Care Med. 2014;42:1983–90.
Albrecht K, Nave H, Breitmeier D, et al. Applied anatomy of the superior vena cava-the carina as a landmark to guide central venous catheter placement. Br J Anaesth. 2004;92:75–7.
Khouzam RN, Minderman D, D’Cruz IA. Echocardiography of the superior vena cava. Clin Cardiol. 2005;28:362–6.
Kwon TD, Kim KH, Ryu HG, et al. Intra- and extra-pericardial lengths of the superior vena cava in vivo: implication for the positioning of central venous catheters. Anaesth Intensive Care. 2005;33:384–7.
Sonavane SK, Milner DM, Singh SP, et al. Comprehensive imaging review of the superior vena cava. Radiographics. 2015;35:1873–92.
Gindea AJ, Slater J, Kronzon I. Doppler echocardiography flow velocity measurements in the superior vena cava during the Valsalva maneuver in normal subjects. Am J Cardiol. 1990;65:1387–91.
Hofer CK, Senn A, Weibel L, et al. Assessment of stroke volume variation for prediction of fluid responsiveness using the modified FloTrac™ and PiCCOplus™ system. Crit Care. 2008;12:R82.
Vos JJ, Poterman M, Salm PP, et al. Noninvasive pulse pressure variation and stroke volume variation to predict fluid responsiveness at multiple thresholds: a prospective observational study. Can J Anaesth. 2015;62:1153–60.
Slagt C, Malagon I, Groeneveld ABJ. Systematic review of uncalibrated arterial pressure waveform analysis to determine cardiac output and stroke volume variation. Br J Anaesth. 2014;112:626–37.
Meng L, Tran NP, Alexander BS, et al. The impact of phenylephrine, ephedrine, and increased preload on third-generation Vigileo FloTrac and esophageal doppler cardiac output measurements. Anesth Analg. 2011;113:751–7.
Kusaka Y, Ohchi F, Minami T. Evaluation of the fourth-generation flotrac/vigileo system in comparison with the intermittent bolus thermodilution method in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2019;33(4):953–60.
Maeda T, Hattori K, Sumiyoshi M, et al. Accuracy and trending ability of the fourth-generation FloTrac/Vigileo System™ in patients undergoing abdominal aortic aneurysm surgery. J Anesth. 2018;32(3):387–93.
Ji F, Li J, Fleming N, et al. Reliability of a new 4th generation FloTrac algorithm to track cardiac output changes in patients receiving phenylephrine. J Clin Monit Comput. 2015;29:467–73.
Derichard A, Robin E, Tavernier B, et al. Automated pulse pressure and stroke volume variations from radial artery: evaluation during major abdominal surgery. Br J Anaesth. 2009;103:678–84.
Benes J, Chytra I, Altmann P, et al. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study. Crit Care. 2010;14:R118.
Funk DJ, HayGlass KT, Koulack J, et al. A randomized controlled trial on the effects of goal-directed therapy on the inflammatory response open abdominal aortic aneurysm repair. Crit Care. 2015;19:247.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bubenek-Turconi, ŞI., Hendy, A., Băilă, S. et al. The value of a superior vena cava collapsibility index measured with a miniaturized transoesophageal monoplane continuous echocardiography probe to predict fluid responsiveness compared to stroke volume variations in open major vascular surgery: a prospective cohort study. J Clin Monit Comput 34, 491–499 (2020). https://doi.org/10.1007/s10877-019-00346-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00346-4