Abstract
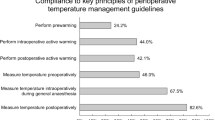
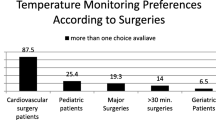
The prevention and treatment of hypothermia is an important part of routine anesthesia care. Avoidance of perioperative hypothermia was introduced as a quality metric in 2010. We sought to assess the integrity of the perioperative hypothermia metric in routine care at a single large center. Perioperative temperatures from all anesthetics of at least 60 min duration between January 2012 and 2017 were eligible for inclusion in analysis. Temperatures were displayed graphically, assessed for normality, and analyzed using paired comparisons. Automatically-recorded temperatures were obtained from several monitoring sites. Provider-entered temperatures were non-normally distributed, exhibiting peaks at temperatures at multiples of 0.5 °C. Automatically-acquired temperatures, on the other hand, were more normally distributed, demonstrating smoother curves without peaks at multiples of 0.5 °C. Automatically-acquired median temperature was highest, 36.8 °C (SD = 0.8 °C), followed by the three manually acquired temperatures (nurse-documented postoperative temperature, 36.5 °C [SD = 0.6 °C]; intraoperative manual temperature, 36.5 °C [SD = 0.6 °C]; provider-documented postoperative temperature, 36.1 °C [SD = 0.6 °C]). Provider-entered temperatures exhibit values that are unlikely to represent a normal probability distribution around a central physiologic value. Manually-entered perioperative temperatures appear to cluster around salient anchoring values, either deliberately, or as an unintended result driven by cognitive bias. Automatically-acquired temperatures may be superior for quality metric purposes.

Similar content being viewed by others
References
Hart SR, et al. Unintended perioperative hypothermia. Ochsner J. 2011;11(3):259–70.
Madrid E, et al. Active body surface warming systems for preventing complications caused by inadvertent perioperative hypothermia in adults. Cochrane Database Syst Rev. 2016;4:Cd009016.
Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209–15.
Poveda VB, Nascimento AS. The effect of intraoperative hypothermia upon blood transfusion needs and length of stay among gastrointestinal system cancer surgery. Eur J Cancer Care (Engl), 2017. 26(6).
Yi J, et al. Maintaining intraoperative normothermia reduces blood loss in patients undergoing major operations: a pilot randomized controlled clinical trial. BMC Anesthesiol. 2018;18(1):126.
Wong PF, et al. Randomized clinical trial of perioperative systemic warming in major elective abdominal surgery. Br J Surg. 2007;94(4):421–6.
Alderson P, et al. Thermal insulation for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev, 2014(6): Cd009908.
Sun Z, et al. Intraoperative core temperature patterns, transfusion requirement, and hospital duration in patients warmed with forced air. J Am Soc Anesthesiol. 2015;122(2):276–85.
PQRS Measure #193: Perioperative Temperature Management. 2015. https://www.pqrspro.com/cmsmeasures/2015/perioperative_temperature_management/. Accessed 25 Mar 2017.
PQRS Measure #424: Perioperative Temperature Management. 2016. https://www.pqrspro.com/cmsmeasures/2016/perioperative_temperature_management-2/. Accessed 25 Mar 2017.
Medicare CF, Services M. Physician quality reporting system. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.html. Accessed 21 June 2012.
Wax DB, et al. Manual editing of automatically recorded data in an anesthesia information management system. J Am Soc Anesthesiol. 2008;109(5):811–5.
Thavarajah S, White WB, Mansoor GA. Terminal digit bias in a specialty hypertension faculty practice. J Hum Hypertens. 2003;17(12):819–22.
von Elm E, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
Deal LG, et al. Are anesthesia start and end times randomly distributed? The influence of electronic records. J Clin Anesth. 2014;26(4):264–70.
Phelps M, et al. Comparison of minute distribution frequency for anesthesia start and end times from an anesthesia information management system and paper records. J Clin Monit Comput. 2016: 31: 1–6.
Slutsky AS, Ranieri VM. Mechanical ventilation: lessons from the ARDSNet trial. Respir Res. 2000;1(2):73–7.
Chatterjee P, Joynt KE. Do cardiology quality measures actually improve patient outcomes? J Am Heart Assoc. 2014;3(1):e000404.
Burack JH, et al. Public reporting of surgical mortality: a survey of New York State cardiothoracic surgeons. Ann Thor Surg. 1999;68(4):1195–200.
Hua M, et al. Impact of public reporting of 30-day mortality on timing of death after coronary artery bypass graft surgery. Anesthesiology. 2017;127(6):953–60.
Van Schalkwyk J, et al. Does manual anaesthetic record capture remove clinically important data? Br J Anaesthesia. 2011;107(4):546–52.
Block FE. Normal fluctuation of physiologic cardiovascular variables during anesthesia and the phenomenon of “smoothing”. J Clin Monit. 1991;7(2):141–5.
Hermanns H, et al. Assessment of skin temperature during regional anaesthesia-What the anaesthesiologist should know. Acta Anaesthesiol Scand. 2018;62(9):1280–9.
Acknowledgements
Patrick Jablonski, Ph.D., provided statistical recommendations to assist in the preparation and refinement of the statistical analysis.
Funding
Dr. Freundlich receives Grant support from an NIH-NCATS KL2 (KL2 TR002245).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Freundlich has received grant support and consulting fees from Medtronic for work unrelated to the content of this manuscript.
Rights and permissions
About this article
Cite this article
Freundlich, R.E., Nelson, S.E., Qiu, Y. et al. A retrospective evaluation of the risk of bias in perioperative temperature metrics. J Clin Monit Comput 33, 911–916 (2019). https://doi.org/10.1007/s10877-018-0233-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0233-1