Abstract
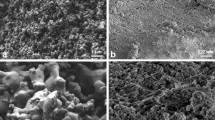
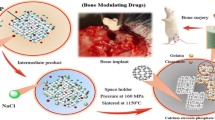
Natural or synthetic biomaterials are increasingly being used to support bone tissue repair or substitution. The combination of natural calcium phosphates with biocompatible alloys is an important route towards the development of new biomaterials with bioperformance and mechanical responses to mimic those of human bones. This article evaluated the structural, physical, mechanical and biological properties of a new mechanical improved nanocomposite elaborated by association of fish biphasic calcium phosphate (BCP) and niobium pentoxide (Nb2O5). The nanocomposite (Nb-BCP) and the pure BCP, used as a positive control, were obtained by powder metallurgy. The density, porosity and microhardness were measured. The structural analysis was determined by X-ray diffraction (XRD) and the biological properties were studied in histological sections of critical size calvaria defects in rats, 7, 15, 30, 45 and 60 days after implantation of disks of both materials. Morphological description was made after scanning electron microscopy (SEM) and optical microscopy analysis. After sintering, the Nb-BCP nanocomposite presented four crystalline phases: 34.36% calcium niobate (CaNb2O6), 21.68% phosphorus niobium oxide (PNb9O25), 42.55% β-tricalcium phosphate (Ca3(PO4)2) and 1.31% of niobium pentoxide (Nb2O5) and exhibited increases of 17% in density, 66% in Vickers microhardness and 180% in compressive strength compared to pure BCP. In vivo study, showed biocompatibility, bioactivity and osteoconductivity similar to pure BCP. SEM showed the formation of globular accretions over the implanted nanocomposites, representing one of the stages of bone mineralization. In conclusion, the BCP and Nb2O5 formed a nanocomposite exhibiting characteristics that are desirable for a biomaterial, such as bioperformance, higher β-TCP percentage and improved physical and mechanical properties compared to pure BCP. These characteristics demonstrate the promise of this material for supporting bone regeneration.











Similar content being viewed by others
References
Service RS. Tissue engineers build new bone. Science. 2000;289:1498–500.
Khan WS, Rayan F, Dhinsa BS, Marsh D. An osteoconductive, osteoinductive, and osteogenic tissue-engineered product for trauma and orthopaedic surgery: how far are we? Stem Cells Int. 2012;2012:236231.
Henkel J, Woodruff MA, Epari DR, Steck R, Glatt V, Dickinson IC et al. Bone regeneration based on tissue engineering conceptions—a 21st century perspective. Bone Res. 2013;1:216–48.
Pacifici L, De Angelis F, Orefici A, Cielo A. Metals used in maxillofacial surgery. Oral Implantol. 2016;9(Suppl 1/2016 to N4/2016):107–11.
Hattar S, Asselin A, Greenspan D, Oboeuf M, Berdal A, Sautier JM. Potential of biomimetic surfaces to promote in vitro osteoblast-like cell differentiation. Biomaterials. 2005;26:839–48.
Long M, Rack HJ. Titanium alloys in total joint replacement—a materials science perspective. Biomaterials. 1998;19:1621–39.
Ramírez G, Rodil SE, Arzate H, Muhl S, Olaya LL. Niobium based coatings for dental implants. Appl Surf Sci. 2011;257:2555–9.
Okazak Y, Nishimura E, Nakada H, Kobayashi K. Surface analysis of Ti-15Zr-4Nb-4Ta alloy after implantation in rat tibia. Biomaterials. 2001;22:599–607.
Yamamoto A, Honma R, Sumita M, Hanawa T. Cytotoxicity evaluation of ceramic particles of different sizes and shapes. J Biomed Mater Res A. 2004;68:244–56.
Rigo ECS, Oliveira LC, Santos LA, Bosch AO, Carrodeguas RG. Implantes metálicos recobertos com hidroxiapatita. Rev Bras Eng Biomed. 1999;15:21–29.
Legeros RZ. Properties of osteoconductive biomaterials: calcium phosphates. Clin Orthop Relat Res. 2002;395:81–98.
Dorozhkin SV. Nanodimensional and nanocrystalline apatites and other calcium orthophosphates in biomedical engineering, biology and medicine. Materials. 2009;2:1975–2045.
Ono I, Tateshita T, Nakajima T. Evaluation of a high-density polyethylene fixing system for hydroxyapatite ceramic implants. Biomaterials. 2000;21:143–51.
Fleckenstein KB, Cuenin MF, Peacock ME, Billman MA, Swiec GD, Buxton TB et al. Effect of a hydroxyapatite tricalcium phosphate alloplast on osseous repair in the rat calvarium. J Periodontol. 2006;77:39–45.
Kumar P, Vinitha B, Fathima G. Bone grafts in dentistry. J Pharm Bioallied Sci. 2013;5(Suppl 1):S125–7.
Dorozhkin SV. Calcium orthophosphate-based biocomposites and hybrid biomaterials. J Mat Sci. 2009;44:2343–87.
Liu B, Lun D. Current application of β-tricalcium phosphate composites in orthopaedics. Orthop Surg. 2012;4:139–44.
Arifin A, Sulong AB, Muhamad N, Syarif J, Ramli MI. Material processing of hydroxyapatite and titanium alloy (HA/Ti) composite as implant materials using powder metallurgy: a review. Mater and Design. 2014;55:165–75.
Aminzare M, Eskandari A, Baroonian MH, Berenov A, Razavi Hesabi Z, Taheri M et al. Hydroxyapatite nanocomposites: synthesis, sintering and mechanical properties. Ceram Int. 2013;39:2197–206.
Drdlik D, Slama M, Hadraba H, Cihlar J. Hydroxyapatite/zirconia-microfibre composites with controlled microporosity and fracture properties prepared by electrophoretic deposition. Ceram Int. 2015;41:11202–12.
Velten D, Eisenbarth E, Schanne N, Breme J. Biocompatible Nb2O5 thin films prepared by means of the sol-gel process. J Mater Sci Mater Med. 2004;15:457–61.
Li Y, Munir KS, Lin J, Wen C. Titanium-niobium pentoxide composites for biomedical applications. Bioact Mater. 2016;1:127–31.
Miyazaki T, Kim HM, Kokubo T, Ohtsuki C, Nakamura T. Apatite-forming ability of niobium oxide gels in a simulated body fluid. J Ceram Soc Jpn. 2001;109:929–33.
Bonadio TGM, Fiorentin ER, Candido AG, Miyahara RY, Freitas VF, Kiyochi HJ, Jr, Hernandes L, Rosso JM, Burato JA, Santos IA, Baesso ML, Weinand WR. Enhanced mechanical properties and osseointegration features of CaNb2O6-PNb9O25-Ca3(PO4)2triphasic nanostructured bioceramics derived by optimised sinterization of Nb2O5 and natural hydroxyapatite-β-tricalcium phosphate. Ceram Int. 2020;46(8):12837–45.
Demirkol N, Oktar FN, Kayali ES. Influence of niobium oxide on the mechanical properties of hydroxyapatite. Key Eng Mat. 2013;529–530:29–33.
Nascimento WJ, Bonadio TGM, Freitas VF, Weinand WR, Baesso ML, Lima WM. Nanostructured Nb2O5-natural hydroxyapatite formed by the mechanical alloying method: a bulk composite. Mater Chem Phys. 2011;130:84–9.
Bonadio TGM, Sato F, Medina AN, Weinand WR, Baesso ML, Lima WM. Bioactivity and structural properties of nanostructured bulk composites containing Nb2O5 and natural hydroxyapatite. J Appl Phys. 2013;113:1–8.
Cesar R, Leivas TP, Pereira CAM, Boffa RS, Guarniero R, Reiff RBM et al. Axial compressive strength of human vertebrae trabecular bones classified as normal, osteopenic and osteoporotic by quantitative ultrasonometry of calcaneus. Res Biomed Eng. 2017;33:91–6.
Havaldar R, Pilli SC, Putti BB. Insights into the effects of tensile and compressive loadings on human femur bone. Adv Biomed Res. 2020;3:1–5.
Karpiński R, Jaworski Ł, Czubacka P. The structural and mechanical properties of the bone. J Technol Exploit Mech Eng. 2017;3:43–50.
Coelho TM, Nogueira ES, Steimacher A, Medina AN, Weinand WR, Lima WM et al. Characterization of natural nanostructured hydroxyapatite obtained from the bones of Brazilian river fish. J Appl Phys. 2006;100:094312.
C773-88. Standard test method for compressive (crushing) strength of fired whiteware materials. West Conshohocken, United States: ASTM International; 2016. pp. 1–4.
C373-88. Standard Test Method for Water Absorption, Bulk Density, Apparent Porosity, and Apparent Specific Gravity of Fired Whiteware Products. West Conshohocken, United Stated: ASTM International; 2006. pp. 1–2.
Standard test method 42: Method for determination of density of compacted or sintered powder metallurgy (PM) products materials. Metal Powder Industries Federation (MPIF). Princeton, NJ, 2019.
Oliver WC, Pharr GM. An improved technique for determining hardness and elastic modulus using load and displacement sensing indentation experiments. J Mater Res. 1992;7:1564–83.
Young RA. The Rietveld method. New York: Oxford University Press; 1995.
Schmitz JP, Hollinger JO. The critical size defect as an experimental model for craniomandibulofacial nonunions. Clin Orthop Relat Res. 1986;205:299–308.
Powder Diffraction Files (PDF) of Joint Committee on Powder Diffraction Standards (JCPDS) database. Access through the website https://bdec.dotlib.com.br/ in Inorganic Crystal Structure Database (ICSD) through the agreement with the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) from Brazil.
Strong E, Moulthrop T. Calvarial bone graft harvest: a new technique. Otolaryng Head Neck Surg. 2000;123:547–52.
Cameron JA, Milner DJ, Lee JS, Cheng J, Fang NX, Jasiuk IM. Employing the biology of successful fracture repair to heal critical size bone defects. Curr Top Microbiol Immunol. 2013;367:113–32.
Yetmez M. Sintering behavior and mechanical properties of biphasic calcium phosphate ceramics. Adv Mater Sc Eng. 2014;2014:1–5.
Demirkol N, Oktar FN, Kayali ES. Mechanical and microstructural properties of sheep hydroxyapatite (SHA)–niobium oxide composites. Acta Phys Pol A. 2012;121:274–6.
Oktar FN. Hydroxyapatite–TiO2 composites. Mater Lett. 2006;60:2207–10.
Roman-Lopez J, Correcher V, Garcia-Guinea J, Rivera T, Lozano IB. Thermal and electron stimulated luminescence of natural bones, commercial hydroxyapatite and collagen. Spectrochim Acta A. 2014;120:610–5.
Suryanarayana C. Mechanical alloying and milling. Prog Mater Sci. 2001;46:39–42.
Liu Q, Huang S, Matinlinna JP, Chen Z, Pan H. Insight into biological apatite: physiochemical properties and preparation approaches. BioMed Res Int. 2013;2013:1–13.
Liu DM, Troczynski T, Tseng WJ. Water-based sol-gel synthesis of hydroxyapatite: process development. Biomaterials. 2001;22:1721–30.
Qaisar SA, Bilton M, Wallace R, Brydson R, Brown AP, Ward M et al. Sol–gel synthesis and TEM-EDX characterization of hydroxiapatite nanoscale powders modified by Mg, Sr or Ti. J Phys: Conf Series. 2010;241:1–4.
Gutierres M, Lopes MA, Hussain NS, Cabral AT, Almeida L, Santos JD. Substitutos ósseos—conceitos gerais e estado actual. Arq Med. 2006;19:153–62.
Velard F, Braux J, Amedee J, Laquerriere P. Inflammatory cell response to calcium phosphate biomaterial particles: an overview. Acta Biomater. 2013;9:4956–63.
Bhumiratana S, Grayson WL, Castaneda A, Rockwood DN, Gil ES, Kaplan DL et al. Nucleation and growth of mineralized bone matrix on silk-hydroxyapatite composite scaffolds. Biomaterials. 2011;32:2812–20.
Galois L, Mainard D. Bone ingrowth into two porous ceramics with different pore sizes: an experimental study. Acta Orthop Belg. 2004;70:598–603.
Hench LL. Characterization of bioceramics. In: Hench LL, Wilson J, editors. An introduction to bioceramics. River Edge, EUA: World Scientific Publishing; 1993.
Dupoirieux L, Pourquier D, Picot MC, Neves M. Comparative study of three different membranes for guided bone regeneration of rat cranial defects. Int J Oral Maxillofac Surg. 2001;30:58–62.
Braz F, Rahal SC, Rocha NS, Taga E, Biasi F. Emprego de matriz óssea orgânica bovina e hidroxiapatita no reparo de defeito induzido em crânio de ratos. Acta Cir Bras. 2003;18:19–24.
Moreschi E, Hernandes L, Dantas JA, da Silva MA, Casaroto AR, Bersani-Amado CA. Effect of dolomite on the repair of bone defects in rats: histological study. Histol Histopathol. 2010;25:1547–56.
Ko JCH. Investigating the process of cement line maturation on substrate surfaces with submicron under cuts. Toronto, Canada: University of Toronto; 2010.
Davies JE, Hosseini MM. Histodynamics of endosseus wound healing. In: Davies JE, editor. Bone engineering. Toronto: Em Squared Inc. pp. 1–14.
von Ebner V. Ueber den feineren Bau der Knochensubstanz. Sber Akad Wiss Wien III. 1875;72:49–138.
Davies JE. In vitro modeling of the bone/implant interface. Anat Rec. 1996;245:426–45.
Zhou H, Chernecky R, Davies JE. Deposition of cement at reversal lines in rat femoral bone. J Bone Miner Res. 1994;9:367–74.
Orr RD, de Brujin JD, Davies JE. Scanning electron microscopy of the bone interface with titanium, titanium alloy and hydroxyapatite. Cells Mat. 1992;2:241–51.
Anselme K. Osteoblast adhesion on biomaterials. Biomaterials. 2000;21:652–67.
Acknowledgements
We are thankful to Brazilian Agencies CAPES, CNPq, FINEP, and Fundação Araucária for the financial support of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures involving the use of animals were approved (under number 079/2010) by the Ethics Committee on the Use of Animals (CEUA) of Universidade Estadual de Maringá, in accordance with the terms of article 8 of Federal Law 11794/2008.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kiyochi Junior, H.d.J., Candido, A.G., Bonadio, T.G.M. et al. In vivo evaluation of interactions between biphasic calcium phosphate (BCP)-niobium pentoxide (Nb2O5) nanocomposite and tissues using a rat critical-size calvarial defect model. J Mater Sci: Mater Med 31, 71 (2020). https://doi.org/10.1007/s10856-020-06414-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-020-06414-5