Abstract
Purpose
To investigate the cumulative live birth (cLB) rate of one complete freeze-all-IVF cycle in a general infertile population and to investigate patient and treatment variables that predict blastocyst development and live birth (LB).
Method
In a retrospective observational study, the data of all IVF cycles performed between 1 February 2015 and 31 January 2016 at a single IVF centre was investigated. In the study, patient-couples were followed up for 18 months following oocyte retrieval. After exclusions, the patient and treatment variables of 1582 patient-couples who underwent treatment were included in the analyses.
Results
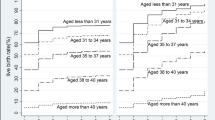
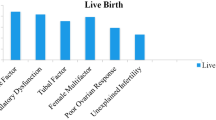
The median time interval between the oocyte retrieval attempt and the frozen embryo transfer (FET) in which LB was achieved was 38.0 (35.0–67.0) days. The variables of freeze-all-IVF cycles with single blastocyst FET selected by multiple logistic regression to predict LB significantly were female age, infertility duration, FET number (i.e. 1st, 2nd, or ≥ 3rd FET), and blastocyst quality. In a regression adjusting for female age, the number of blastocysts transferred, and oocyte number group (1–3, 4–9, 10–15, and > 15), none of the oocyte number groups were selected to predict LB of 1st FET, significantly. While the per transfer LB rates decreased linearly from the 1st (56.5%) to the 3rd (36.4%) FET, the cLB rate increased from 47.3% after the 1st FET to 55.0% after a 3rd possible FET.
Conclusion
The cLB rate of one complete freeze-all-IVF cycle of a general infertile population, with 18-month follow-up, was 55.0%. In freeze-all-IVF, ovarian reserve variables were not selected by regression models to predict LB, significantly.
Similar content being viewed by others
References
Rogers PA, Milne BJ, Trounson AO. A model to show human uterine receptivity and embryo viability following ovarian stimulation for in vitro fertilization. J In Vitro Fert Embryo Transf. 1986;3:93–8.
Practice Committee of American Society for Reproductive Medicine. Gonadotropin preparations: past, present, and future perspectives. Fertil Steril. 2008;90:S13–20.
Devroey P, Polyzos NP, Blockeel C. An OHSS-free clinic by segmentation of IVF treatment. Hum Reprod. 2011;26:2593–7.
Evans J, Hannan NJ, Edgell TA, Vollenhoven BJ, Lutjen PJ, Osianlis T, et al. Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Hum Reprod Update. 2014;20:808–21.
Baker VL, Brown MB, Luke B, Smith GW, Ireland JJ. Gonadotropin dose is negatively correlated with live birth rate: analysis of more than 650,000 assisted reproductive technology cycles. Fertil Steril. 2015;104:1145–52.
Haahr T, Roque M, Esteves SC, Humaidan P. GnRH agonist trigger and LH activity luteal phase support versus hCG trigger and conventional luteal phase support in fresh embryo transfer IVF/ICSI cycles—a systematic PRISMA review and meta-analysis. Front Endocrinol (Lausanne). 2017;8:116.
Stone BA, March CM, Ringler GE, Baek KJ, Marrs RP. Casting for determinants of blastocyst yield and of rates of implantation and of pregnancy after blastocyst transfers. Fertil Steril. 2014;102:1055–64.
Baker VL, Brown MB, Luke B, Conrad KP. Association of number of retrieved oocytes with live birth rate and birth weight: an analysis of 231,815 cycles of in vitro fertilization. Fertil Steril. 2015;103:931–8.
Ji J, Liu Y, Tong XH, Luo L, Ma J, Chen Z. The optimum number of oocytes in IVF treatment: an analysis of 2455 cycles in China. Hum Reprod. 2013;28:2728–34.
Steward RG, Lan L, Shah AA, Yeh JS, Price TM, Goldfarb JM, et al. Oocyte number as a predictor for ovarian hyperstimulation syndrome and live birth: an analysis of 256,381 in vitro fertilization cycles. Fertil Steril. 2014;101:967–73.
Chen YH, Xu XH, Wang Q, Zhang SD, Jiang LL, Zhang CL, et al. Optimum oocyte retrieved and transfer strategy in young women with normal ovarian reserve undergoing a long treatment protocol: a retrospective cohort study. J Assist Reprod Genet. 2015;32:1459–67.
Drakopoulos P, Blockeel C, Stoop D, Camus M, de Vos M, Tournaye H, et al. Conventional ovarian stimulation and single embryo transfer for IVF/ICSI. How many oocytes do we need to maximize cumulative live birth rates after utilization of all fresh and frozen embryos? Hum Reprod. 2016;31:370–6.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C. Clinical rationale for cryopreservation of entire embryo cohorts in lieu of fresh transfer. Fertil Steril. 2014;102:3–9.
Blockeel C, Drakopoulos P, Santos-Ribeiro S, Polyzos NP, Tournaye H. A fresh look at the freeze-all protocol: a SWOT analysis. Hum Reprod. 2016;31:491–7.
Ozgur K, Humaidan P, Coetzee K. Segmented ART—the new era in ART? Reprod Biol. 2016;16:91–103.
Ata B, Seli E. A universal freeze all strategy: why it is not warranted. Curr Opin Obstet Gynecol. 2017;29(3):136–45.
Dieamant FC, Petersen CG, Mauri AL, Comar V, Mattila M, Vagnini LD, et al. Fresh embryos versus freeze-all embryos—transfer strategies: nuances of a meta-analysis. JBRA Assist Reprod. 2017;21:260–72.
Coates A, Kung A, Mounts E, Hesla J, Bankowski B, Barbieri E, et al. Optimal euploid embryo transfer strategy, fresh vs frozen, following PGS with NGS. A randomized controlled trial. Fertil Steril. 2017;107:723–30.
Roque M, Valle M, Kostolias A, Sampaio M, Geber S. Freeze-all cycle in reproductive medicine: current perspectives. JBRA Assist Reprod. 2017;21:49–53.
Maheshwari A, Raja EA, Bhattacharya S. Obstetric and perinatal outcomes after either fresh or thawed frozen embryo transfer: an analysis of 112,432 singleton pregnancies recorded in the Human Fertilisation and Embryology Authority anonymized dataset. Fertil Steril. 2016;106:1703–8.
Teh WT, McBain J, Rogers P. What is the contribution of embryo-endometrial asynchrony to implantation failure? J Assist Reprod Genet. 2016;33:1419–30.
Zhao J, Xu B, Zhang Q, Li YP. Which one has a better obstetric and perinatal outcome in singleton pregnancy, IVF/ICSI or FET?: a systematic review and meta-analysis. Reprod Biol Endocrinol. 2016;14:51.
Zhu Q, Chen Q, Wang L, Lu X, Lyu Q, Wang Y, et al. Live birth rates in the first complete IVF cycle among 20 687 women using a freeze-all strategy. Hum Reprod. 2018;33(5):924–9.
Ozgur K, Bulut H, Berkkanoglu M, Humaidan P, Coetzee K. Increased body mass index associated with increased preterm delivery in frozen embryo transfers. J Obstet Gynaecol. 2018. accepted for publication.
Ozgur K, Bulut H, Berkkanoglu M, Humaidan P, Coetzee K. Artificial frozen embryo transfer cycle success depends on blastocyst developmental rate and progesterone timing. Reprod BioMed Online. 2018;36:269–76.
Gardner DK, Schoolcraft WB. In vitro culture of human blastocysts. In: Jansen R, Mortimer D, editors. Toward reproductive certainty: fertility and genetics beyond 1999. London: Parthenon Publishing; 1999. p. 378–88.
Ozgur K, Berkkanoglu M, Bulut H, Humaidan P, Coetzee K. Agonist depot versus OCP programming of frozen embryo transfer: a retrospective analysis of freeze-all cycles. J Assist Reprod Genet. 2016;33:207–14.
ALPHA Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26:1270–83.
Ahlström A, Westin C, Reismer E, Wikland M, Hardarson T. Trophectoderm morphology: an important parameter for predicting live birth after single blastocyst transfer. Hum Reprod. 2011;26:3289–96.
McLernon DJ, Steyerberg EW, Te Velde ER, Lee AJ, Bhattacharya S. Predicting the chances of a live birth after one or more complete cycles of in vitro fertilisation: population based study of linked cycle data from 113 873 women. BMJ. 2016;355:i5735.
De Vos A, Van Landuyt L, Santos-Ribeiro S, Camus M, Van de Velde H, Tournaye H, et al. Cumulative live birth rates after fresh and vitrified cleavage-stage versus blastocyst-stage embryo transfer in the first treatment cycle. Hum Reprod. 2016;31:2442–9.
Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. 2016;6:CD002118.
ESHRE Special Interest Group of Embryology and Alpha Scientists in Reproductive Medicine. The Vienna consensus: report of an expert meeting on the development of ART laboratory performance indicators. Reprod BioMed Online. 2017;35:494–510.
Swain JE, Carrell D, Cobo A, Meseguer M, Rubio C, Smith GD. Optimizing the culture environment and embryo manipulation to help maintain embryo developmental potential. Fertil Steril. 2016;105:571–87.
Thomas MR, Sparks AE, Ryan GL, Van Voorhis BJ. Clinical predictors of human blastocyst formation and pregnancy after extended embryo culture and transfer. Fertil Steril. 2010;94:543–8.
Dessolle L, Fréour T, Barrière P, Daraï E, Ravel C, Jean M, et al. A cycle-based model to predict blastocyst transfer cancellation. Hum Reprod. 2010;25:598–604.
ACOG Committee on Gynecologic Practice; Practice Committee of the ASRM. Female age-related fertility decline. Committee Opinion No. 589. Obstet Gynecol. 2014;123:719–21.
Roberts SA, Hann M, Brison DR. Factors affecting embryo viability and uterine receptivity: insights from an analysis of the UK registry data. Reprod BioMed Online. 2016;32:197–206.
Vaegter KK, Lakic TG, Olovsson M, Berglund L, Brodin T, Holte J. Which factors are most predictive for live birth after in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) treatments? Analysis of 100 prospectively recorded variables in 8,400 IVF/ICSI single-embryo transfers. Fertil Steril. 2017;107:641–8.
Gianaroli L, Magli MC, Cavallini G, Crippa A, Capoti A, Resta S, et al. Predicting aneuploidy in human oocytes: key factors which affect the meiotic process. Hum Reprod. 2010;25:2374–86.
Ata B, Kaplan B, Danzer H, Glassner M, Opsahl M, Tan SL, et al. Array CGH analysis shows that aneuploidy is not related to the number of embryos generated. Reprod BioMed Online. 2012;24:614–20.
Labarta E, Bosch E, Mercader A, Alamá P, Mateu E, Pellicer A. A higher ovarian response after stimulation for IVF is related to a higher number of euploid embryos. Biomed Res Int. 2017;2017:5637923.
Wong KM, van Wely M, Mol F, Repping S, Mastenbroek S. Fresh versus frozen embryo transfers in assisted reproduction. Cochrane Database Syst Rev. 2017;3:CD011184.
Katz-Jaffe MG, Surrey ES, Minjarez DA, Gustofson RL, Stevens JM, Schoolcraft WB. Association of abnormal ovarian reserve parameters with a higher incidence of aneuploid blastocysts. Obstet Gynecol. 2013;121:71–7.
Shahine LK, Marshall L, Lamb JD, Hickok LR. Higher rates of aneuploidy in blastocysts and higher risk of no embryo transfer in recurrent pregnancy loss patients with diminished ovarian reserve undergoing in vitro fertilization. Fertil Steril. 2016;106:1124–8.
Sekhon L, Shaia K, Santistevan A, Cohn KH, Lee JA, Beim PY, et al. The cumulative dose of gonadotropins used for controlled ovarian stimulation does not influence the odds of embryonic aneuploidy in patients with normal ovarian response. J Assist Reprod Genet. 2017;34:749–58.
Lainas TG, Sfontouris IA, Venetis CA, Lainas GT, Zorzovilis IZ, Tarlatzis BC, et al. Live birth rates after modified natural cycle compared with high-dose FSH stimulation using GnRH antagonists in poor responders. Hum Reprod. 2015;30:2321–30.
Reed BG, Babayev SN, Bukulmez O. Shifting paradigms in diminished ovarian reserve and advanced reproductive age in assisted reproduction: customization instead of conformity. Semin Reprod Med. 2015;33:169–78.
Munne S, Held KR, Magli CM, Ata B, Wells D, Fragouli E, et al. Intra-age, intercenter, and intercycle differences in chromosome abnormalities in oocytes. Fertil Steril. 2012;97:935–42.
Ubaldi FM, Capalbo A, Vaiarelli A, Cimadomo D, Colamaria S, Alviggi C, et al. Follicular versus luteal phase ovarian stimulation during the same menstrual cycle (DuoStim) in a reduced ovarian reserve population results in a similar euploid blastocyst formation rate: new insight in ovarian reserve exploitation. Fertil Steril. 2016;105:1488–95.
Vaiarelli A, Cimadomo D, Ubaldi N, Rienzi L, Ubaldi FM. What is new in the management of poor ovarian response in IVF? Curr Opin Obstet Gynecol. 2018;30:155–62.
Chambers GM, Paul RC, Harris K, Fitzgerald O, Boothroyd CV, Rombauts L, et al. Assisted reproductive technology in Australia and New Zealand: cumulative live birth rates as measures of success. Med J Aust. 2017;207:114–8.
McLernon DJ, Maheshwari A, Lee AJ, Bhattacharya S. Cumulative live birth rates after one or more complete cycles of IVF: a population-based study of linked cycle data from 178,898 women. Hum Reprod. 2016b;31:572–81.
Niinimäki M, Veleva Z, Martikainen H. Embryo quality is the main factor affecting cumulative live birth rate after elective single embryo transfer in fresh stimulation cycles. Eur J Obstet Gynecol Reprod Biol. 2015;194:131–5.
Acknowledgements
The authors wish to thank Dr. Peter Humaidan (MD, DMSc) for his signficant contribution to the conceptualisation and design of the study, to the scientific and semantic content of the manuscript, and the critical revision of the reviewed manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key/summary message: The cLB rate of one complete freeze-all-IVF cycle in a general infertile population was 55.0%, with oocyte numbers retrieved not independently predictive of LB.
Rights and permissions
About this article
Cite this article
Ozgur, K., Bulut, H., Berkkanoglu, M. et al. Prediction of live birth and cumulative live birth rates in freeze-all-IVF treatment of a general population. J Assist Reprod Genet 36, 685–696 (2019). https://doi.org/10.1007/s10815-019-01422-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01422-z