Abstract
Purpose
The current study is aimed to present the long-term results of the patients who underwent conjunctivolimbal autograft (CLAU) as the primary operation in unilateral limbal stem cell deficiency and the ocular surface safety of the donor eyes. The patients were followed up for five years or longer.
Methods
The records of all patients who underwent CLAU as the primary operation were retrospectively analyzed. Additional ocular surface operations, ocular surface stability, best-corrected visual acuity (BCVA), and ocular surface status of the donor eyes were investigated.
Results
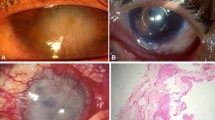
The mean age of the patients at the time of transplantation was 35.07 ± 12.9 (12–60). Twenty-nine eyes of 29 patients were followed up for an average of 97.82 ± 34.45 (60–186) months. Additional ocular surface operation was required in 27.58% (8/29) of the eyes in order to achieve a stable ocular surface. Ocular surface stability was achieved in 82.75% (24/29) of the eyes at the end of the follow-up period. BCVA increased from 1.78 ± 0.82 to 0.91 ± 0.92 logMAR at the last visit (p < 0.001). Corneal ectasia and vascularization developed in one donor eye in the fifth postoperative year.
Conclusions
CLAU tissues provide ocular surface stability with a successful vision result in the long term. CLAU theoretically carries risks including limbal stem cell deficiency in the donor eye. In the long-term follow-up of donor eyes after CLAU, ectasia and limbal stem cell deficiency were observed in one eye.




Similar content being viewed by others
References
Shanbhag SS, Nikpoor N, Rao Donthineni P, Singh V, Chodosh J, Basu S (2020) Autologous limbal stem cell transplantation: a systematic review of clinical outcomes with different surgical techniques. Br J Ophthalmol 104(2):247–253
Holland EJ (2015) Management of limbal stem cell deficiency: a historical perspective, past, present, and future. Cornea 34:S9–S15
Atallah MR, Palioura S, Perez VL, Amescua G (2016) Limbal stem cell transplantation: current perspectives. Clin Ophthalmol 1(10):593–602
Baradaran-Rafii A, Eslani M, Jamali H, Karimian F, Tailor UA, Djalilian AR (2012) Postoperative complications of conjunctival limbal autograft surgery. Cornea 31(8):893–899
Kenyon KR, Tseng SCG (1989) Limbal autograft transplantation for ocular surface disorders. Ophthalmology 96:709–723
Cheung AY, Sarnicola E, Holland EJ (2017) Long-term ocular surface stability in conjunctival limbal autograft donor eyes. Cornea 36(9):1031–1035
Khan-Farooqi H, Chodosh J (2016) Autologous limbal stem cell transplantation: the progression of diagnosis and treatment. Semin Ophthalmol 31(1–2):91–98
Dua HS, Azuara-Blanco A (2000) Autologous limbal transplantation in patients with unilateral corneal stem cell deficiency. Br J Ophthalmol 84:273–278
Le Q, Chauhan T, Yung M, Tseng CH, Deng SX (2020) Outcomes of limbal stem cell transplant: a meta-analysis. JAMA Ophthalmol 138(6):660–670
Burcu A, Yalniz-Akkaya Z, Ozdemir MF, Erdem E, Onat MM, Ornek F (2014) Surgical rehabilitation following ocular chemical injury. Cutan Ocul Toxicol 33(1):42–48
Li W, Hayashida Y, Chen YT, Tseng SC (2007) Niche regulation of corneal epithelial stem cells at the limbus. Cell Res 17(1):26–36
Dua HS, Miri A, Elalfy MS, Lencova A, Said DG (2017) Amnion-assisted conjunctival epithelial redirection in limbal stem cell grafting. Br J Ophthalmol 101(7):913–919
Yin J, Jurkunas U (2018) Limbal stem cell transplantation and complications. Semin Ophthalmol 33(1):134–141
Wylegala E, Dobrowolski D, Tarnawska D, Janiszewska D, Gabryel B, Malecki A et al (2008) Limbal stem cells transplantation in the reconstruction of the ocular surface: 6 years experience. Eur J Ophthalmol 18(6):886–890
Rao SK, Rajagopal R, Sitalakshmi G, Padmanabhan P (1999) Limbal autografting: comparison of results in the acute and chronic phases of ocular surface burns. Cornea 18(2):164–171
Morgan S, Murray A (1996) Limbal auto-transplantation in the acute and chronic phases of severe chemical injuries. Eye (Lond) 10:349–354
Han ES, Wee WR, Lee JH, Kim MK (2007) The long-term safety of donor eye for 180 degrees limbal transplantation. Graefes Arch Clin Exp Ophthalmol 245:745–748
Jenkins C, Tuft S, Liu C, Buckley R (1993) Limbal transplantation in the management of chronic contact-lens-associated epitheliopathy. Eye (Lond) 7:629–633
Basti S, Mathur U (1999) Unusual intermediate-term outcome in three cases of limbal autograft transplantation. Ophthalmology 106:958–963
Shimazaki J, Shinozaki N, Tsubota K (1998) Transplantation of amniotic membrane and limbal autograft for patients with recurrent pterygium associated with symblepharon. Br J Ophthalmol 82:235–240
Tan DT, Ficker LA, Buckley RJ (1996) Limbal transplantation. Ophthalmology 103:29–36
Miri A, Said DG, Dua HS (2011) Donor site complications in autolimbal and living related allolimbal transplantation. Ophthalmology 118:1265–1271
Moldovan SM, Borderie V, Baudrimont M, Laroche L (1999) Treatment of unilateral limbal stem cell deficiency syndrome by limbal autograft. J Fr Ophtalmol 22:302–309
Baradaran-Rafii A, Akbari M, Shirzadeh E, Shams M (2015) Single block conjunctival limbal autograft for unilateral limbal stem cell deficiency. J Ophthalmic Vis Res 10(1):90–92
Chen JJ, Tseng SC (1990) Corneal epithelial wound healing in partial limbal deficiency. Invest Ophthalmol Vis Sci 31:1301–1314
Chen JJ, Tseng SC (1991) Abnormal corneal epithelial wound healing in partial-thickness removal of limbal epithelium. Invest Ophthalmol Vis Sci 32:2219–2233
Sangwan VS, Basu S, MacNeil S, Balasubramanian D (2012) Simple limbal epithelial transplantation (SLET): a novel surgical technique for the treatment of unilateral limbal stem cell deficiency. Br J Ophthalmol 96:931–934
Pellegrini G, Traverso CE, Franzi AT, Cancedda R, De Luca M (1997) Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet 349(9057):990–993
Bonnet C, González S, Roberts JS, Robertson SYT, Ruiz M, Zheng J, Deng SX (2021) Human limbal epithelial stem cell regulation, bioengineering and function. Prog Retin Eye Res 85:100956
Soleimani M, Cheraqpour K, Koganti R, Baharnoori SM, Djalilian AR (2023) Concise review: bioengineering of limbal stem cell niche. Bioengineering (Basel) 10(1):111
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by AB, ZYA, EŞ, and SUÖ. Literature review was performed by FÖ and BNT. The first draft of the manuscript was written by BNT, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose. The authors whose names are listed above certify that they have no conflict of interest in this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nurozler Tabakci, B., Burcu, A., Yalnız Akkaya, Z. et al. Long-term ocular surface stability in conjunctivolimbal autograft and ocular surface safety in the donor eyes. Int Ophthalmol 44, 75 (2024). https://doi.org/10.1007/s10792-024-03035-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03035-7