Abstract
Purpose
To compare the preoperative and postoperative measurements of optical low-coherence reflectometry (OLCR) biometry and assessment of its refractive predictability.
Methods
A total of 114 eyes of 102 patients who underwent cataract treatment were prospectively examined. The axial length (AL), central corneal thickness (CCT), anterior chamber depth (ACD), lens thickness (LT), K (keratometry) 1, K2, K average (KAVE) and K astigmatic (KAST) values were recorded using Lenstar LS 900 (Haag-Streit, Koeniz, Switzerland) OLCR device. The IOL (intraocular lens) power was measured based on the SRK/T formula. The cases were divided into three subgroups according to AL (Group 1: AL < 22 mm, Group 2: 22 mm ≤ AL < 24 mm, Group 3: 24 mm ≤ AL). The mean absolute error (MAE) calculated for each eye.
Results
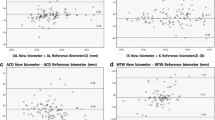
The right eyes of 45 patients (44.1%), left eyes of 45 patients (44.1%), and both eyes of 12 patients (11.7%) were examined. The average AL in the preoperative period was 23.19 ± 1.01; it was 23.20 ± 0.99 in the postoperative period (p > 0.05). A significant deepening was detected in the postoperative ACD (preop 2.76 ± 0.38 mm, postop 3.81 ± 0.46 mm, p < 0.001). CCT was measured as 521.4 ± 36.3 µm in the preoperative period and as 530.8 ± 42.8 (p > 0.05) µm in the postoperative period. The average mean absolute error (MAE) was measured as 0.48 ± 0.41 D, whereas refractive error was − 0.081 ± 0.67 D. The MAE distribution of cases was found to be ≤ 1.5 D 109 (95.6%) eyes, and ≤ 2.0 D in 114 (100%) eyes. MAE values according to AL of the cases were calculated as 0.71 ± 0.83 D in group 1, 0.49 ± 0.43 D in group 2 and 0.41 ± 0.36 D in group 3 (p > 0.05).
Conclusion
When the measurement and refractive results of the OLCR biometry were evaluated, it was observed that there was a very satisfactory result and a predictable device compatible with the current literature. The SRK/T formula, one of the new generation formulas, has shown high MAE and RE results in eyes with AL ≤ 22 mm, although not statistically significant. Other new generation formulas should be tried in these eyes.
Similar content being viewed by others
References
Tabin G, Chen M, Espandar L (2008) Cataract surgery for the developing world. Curr Opin Ophthalmol 19:55–59
Ophthalmology Abouzeid H (2011) New trends in cataract surgery. Rev Med Suisse 7:128–132
Norrby S (2008) Sources of error in intraocular lens power calculation. J Cataract Refract Surg 34:368–376
Olsen T (2007) Calculation of intraocular lens power: a review. Acta Ophthalmol Scand 85:472–485
Salouti R, Nowroozzadeh MH, Zamani M, Ghoreyshi M (2011) Comparison of the ultrasonographic method with 2 partial coherence interferometry methods for intraocular lens power calculation. Optometry 82:140–147
Packer M, Fine IH, Hoffman RS, Coffman PG, Brown LK (2002) Immersion A-scan compared with partial coherence interferometry; outcomes analysis. J Cataract Refract Surg 28:239–242
Holzer MP, Mamusa M, Auffarth GU (2009) Accuracy of a new partial coherence interferometry analyser for biometric measurements. Br J Ophthalmol 93:807–810
Rohrer K, Frueh BE, Walti R, Clemetson IA, Tappeiner C, Goldblum D (2009) Comparison and evaluation of ocular biometry using a new noncontact optical low-coherence reflectometer. Ophthalmology 116:2087–2092
Rabsilber TM, Jepsen C, Auffarth GU, Holzer MP (2010) Intraocular lens power calculation: clinical comparison of 2 optical biometry devices. J Cataract Refract Surg 36:230–234
Bjelos Roncevic M, Busic M, Cima I, Kuzmanovic Elabjer B, Bosnar D, Miletic D (2011) Intraobserver and interobserver repeatability of ocular components measurement in cataract eyes using a new optical low coherence reflectometer. Graefes Arch Clin Exp Ophthalmol 249:83–87
Shammas HJ, Hoffer KJ (2012) Repeatability and reproducibility of biometry and keratometry measurements using a noncontact optical low-coherence reflectometer and keratometer. Am J Ophthalmol 153:55–61
Liampa Z, Kynigopoulos M, Pallas G, Gerding H (2010) Comparison of two partial coherence interferometry devices for ocular biometry. Klin Monbl Augenheilkd 227:285–288
Mylonas G, Sacu S, Buehl W, Ritter M, Georgopoulos M, Schmidt-Erfurth U (2011) Performance of three biometry devices in patients with different grades of age-related cataract. Acta Ophthalmol 89:237–241
Buckhurst PJ, Wolffsohn JS, Shah S, Naroo SA, Davies LN, Berrow EJ (2009) A new optical low coherence reflectometry device for ocular biometry in cataract patients. Br J Ophthalmol 93:949–953
Chen YA, Hirnschall N, Findl O (2011) Evaluation of 2 new optical biometry devices and comparison with the current gold standard biometer. J Cataract Refract Surg 37:513–517
Kolodziejczyk W, Galecki T, Lazicka-Galecka M, Szaflik J (2011) Comparison of the biometric measurements obtained using noncontact optical biometers LenStar LS 900 and IOL Master V. 5. Klin Oczna 113:47–51
Kakoulidis K, Cernak A, Cernak M (2011) Morphologic changes of anterior segment of the eye after cataract surgery. Cesk Slov Oftalmol 67:111–114
Olsen T (2011) Use of fellow eye data in the calculation of intraocular lens power for the second eye. Ophthalmology 118:1710–1715
Hildebrandt AL, Auffarth GU, Holzer MP (2011) Precision of a new device for biometric measurements in pseudophakic eyes. Ophthalmologe 108:739–744
Hoffer KJ, Shammas HJ, Savini G (2010) Comparison of 2 laser instruments for measuring axial length. J Cataract Refract Surg 36:644–648
Kim SM, Choi J, Choi S (2009) Refractive predictability of partial coherence interferometry and factors that can affect it. Korean J Ophthalmol 23:6–12
Eleftheriadis H (2003) IOLMaster biometry: refractive results of 100 consecutive cases. Br J Ophthalmol 87:960–963
Wang JK, Hu CY, Chang SW (2008) Intraocular lens power calculation using the IOLMaster and various formulas in eyes with long axial length. J Cataract Refract Surg 34:262–267
Hasemeyer S, Hugger P, Jonas JB (2003) Preoperative biometry of cataractous eyes using partial coherence laser interferometry. Graefes Arch Clin Exp Ophthalmol 241:251–252
Song BYYK, Yoon KC (2005) Accuracy of partial coherence interferometry in intraocular lens power calculation. J Korean Ophthalmol Soc 46:775–780
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Akalın, İ., Tüfek, M., Türkyılmaz, M. et al. Comparison of preoperative and postoperative measurements of optical low-coherence reflectometry biometry and assessment of its refractive predictability. Int Ophthalmol 39, 1337–1343 (2019). https://doi.org/10.1007/s10792-018-0952-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-018-0952-9