Abstract
Purpose
To compare the characteristics and outcomes of male and female patients that underwent corneal transplantation for keratoconus (KC) in Southern Brazil and worldwide.
Methods
Retrospective longitudinal study that evaluated medical records of patients who were submitted to keratoplasty between August 1990 and September 2015 in two tertiary hospitals in the state of Rio Grande do Sul (Brazil) and review of the Medline and Embase database international literature.
Results
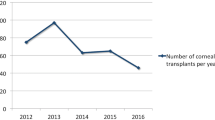
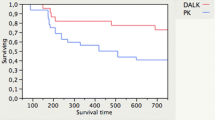
Out of a total of 4026 corneal transplants at that period, 1284 patients (1530 eyes) received preoperative diagnosis of KC (31.8%). A total of 839 men underwent keratoplasty for KC (65.4%) with mean age of 30.3 (±12.2) years. The 445 transplanted women (34.6%) had a mean age of 34.5 (±14.8) years. Both differences were statistically significant (p < 0.01). Regarding laterality, skin color, recipient and donor cornea trephination diameter, and rejection episodes there was no significant difference between the two groups at baseline (p > 0.05). Females were submitted significantly more to deep anterior lamellar keratoplasty (DALK) in comparison with males (26.5 vs. 15.7%, p < 0.01). We were able to include 57.4% of the original keratoplasties for our follow-up data analysis. Male sex and penetrating keratoplasty (PK) were associated significantly with increased risk for graft failure in KC transplantation at the end of follow-up (p < 0.05). The mean follow-up of transplanted patients was similar in both groups.
Conclusion
Keratoconus is the most transplanted corneal disease in Southern Brazil and globally. Studies in Africa, Asia, Europe and North America also showed gender differences in KC patients submitted to keratoplasty. We found that men were transplanted in a 1.9 male/female ratio and at an earlier age than women. At final follow-up, male sex and PK were risk factors associated with increased graft failure. It is essential to broaden the hormonal and genetic investigations to elucidate why keratoconic males have undergone more keratoplasties and have more secondary failure than females.

Similar content being viewed by others
References
Flores VG, Dias HL, Castro RS (2007) Penetrating keratoplasty indications in “Hospital das Clínicas-UNICAMP”. Arq Bras Oftalmol 70:505–508
Kennedy RH, Bourne WM, Dyer JA (1986) A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol 101:267–273
Ashwin PT, McDonnell PJ (2010) Collagen cross-linkage: a comprehensive review and directions for future research. Br J Ophthalmol 94:965–970
Siganos D, Ferrara P, Chatzinikolas K et al (2002) Ferrara intrastromal corneal rings for the correction of keratoconus. J Cataract Refract Surg 28:1947–1951
Abu-Amero KK, Al-Muammar AM, Kondkar AA (2014) Genetics of keratoconus: where do we stand? J Ophthalmol 2014:641708. Epub 2014 Aug 28
Tachibana M, Adachi W, Kinoshita S, Kobayashi Y et al (2002) Androgen-dependent hereditary mouse keratoconus: linkage to an MHC region. Invest Ophthalmol Vis Sci 43:51–57
Kelly TL, Williams KA, Coster DJ (2011) Corneal transplantation for keratoconus: a registry study. Arch Ophthalmol 129:691–697. Epub 2011 Feb 14
Mamalis N, Anderson CW, Kreisler KR, Lundergan MK, Olson RJ (1992) Changing trends in the indications for penetrating keratoplasty. Arch Ophthalmol 110:1409–1411
Yahalom C, Mechoulam H, Solomon A, Raiskup FD, Peer J (2005) Forty years of changing indications in penetrating keratoplasty in Israel. Cornea 24:256–258
Legeais JM, Parc C, d’Hermies F, Pouliquen Y, Renard G (2001) Nineteen years of penetrating keratoplasty in the Hotel-Dieu Hospital in Paris. Cornea 20:603–606
Yorston D, Wood M, Foster A (1996) Penetrating keratoplasty in Africa: graft survival and visual outcome. Br J Ophthalmol 80:890–894
Mkanganwi N, Nondo SI, Guramatunhu S (2000) Indications for corneal grafting in Zimbabwe. Cent Afr J Med 46:300–302
Ameerh MAA, Al Refai RM, Bdour MDA (2012) Keratoconus patients at Jordan University Hospital: a descriptive study. Clin Ophthal 6:1895–1899
Fasolo A, Frigo AC, Böhm E et al (2006) The CORTES study: corneal transplant indications and graft survival in an Italian cohort of patients. Cornea 25:507–515
Godefrooij DA, Gans R, Imhof SM, Wisse RP (2016) Trends in penetrating and anterior lamellar corneal grafting techniques for keratoconus: a national registry study. Acta Ophthalmol. doi:10.1111/aos.13041
Zhang YM, Wu SQ, Yao YF, Zhejiang J (2013) Long-term comparison of full-bed deep anterior lamellar keratoplasty and penetrating keratoplasty in treating keratoconus. Univ Sci B 14:438–450
Al-Mohaimeed MM (2013) Penetrating keratoplasty for keratoconus: visual and graft survival outcomes. Int J Health Sci (Qassim) 7:67–74
Basu S, Reddy JC, Vaddavalli PK, Vemuganti GK, Sangwan VS (2012) Long-term outcomes of penetrating keratoplasty for keratoconus with resolved corneal hydrops. Cornea 31:615–620
Niziol LM, Musch DC, Gillespie BW, Marcotte LM, Sugar A (2013) Long-term outcomes in patients who received a corneal graft for keratoconus between 1980 and 1986. Am J Ophthalmol 155(213–219):e3
Claesson M, Armitage WJ (2009) Ten-year follow-up of graft survival and visual outcome after penetrating keratoplasty in Sweden. Cornea 28:1124–1129
Pramanik S, Musch DC, Sutphin JE, Farjo AA (2006) Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology 113:1633–1688
Brazilian Institute of Geography and Statistics (IBGE). http://cidades.ibge.gov.br/xtras/uf.php?coduf=43. Acessed 22 Feb 2016
Sarezky D, Orlin SE, Pan W, Vander Beek BL (2017) Trends in corneal transplantation in keratoconus. Cornea 36:131–137
Maharana PK, Sharma N, Vajpayee RB (2013) Acute corneal hydrops in keratoconus. Indian J Ophthalmol 61:461–464
Borderie VM, Guilbert E, Touzeau O, Laroche L (2011) Graft rejection and graft failure after anterior lamellar versus penetrating keratoplasty. Am J Ophthalmol 151:1024–1029
Borderie VM, Sandali O, Bullet J, Gaujoux T, Touzeau O, Laroche L (2012) Long-term results of deep anterior lamellar versus penetrating keratoplasty. Ophthalmology 119:249–255
Naderan M, Shoar S, Kamaleddin MA, Rajabi MT, Naderan M, Khodadadi M (2015) Keratoconus clinical findings according to different classifications. Cornea 34:1005–1011
Acknowledgements
Thank you to Mirna Bernardes and Dayane Munhoz for their assistance with this study data collection.
Funding
This study received funding from the Brazilian National Research and Development Council (CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author OAM has received grants from the Brazilian National Research and Development Council. He has no commercial interest on this research. Author RCF and SBM did not receive any grant and have not conflict of interest. None of the authors receive any company honorarium.
Ethical approval
This study was approved by the Federal University Hospital ethical committee/review board (under protocol number 15-0559) and adhered to the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Review Board granted a waiver of consent for chart review.
Human and animals rights
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Magalhaes, O.A., Marafon, S.B. & Ferreira, R.C. Gender differences in keratoconus keratoplasty: a 25-year study in Southern Brazil and global perspective. Int Ophthalmol 38, 1627–1633 (2018). https://doi.org/10.1007/s10792-017-0634-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-017-0634-z