Abstract
The prevalence of cardiac amyloidosis has progressively increased over the last years, being recognized as a significant cause of heart failure. In fact, the management of advanced heart failure is a cornerstone treatment of amyloid cardiomyopathy due to the frequent delay in its diagnosis. Left ventricular assist devices (LVADs) have been gaining importance in the scenario of end-stage heart failure, representing an alternative to heart transplant. However, only few studies have investigated the role of LVAD in restrictive cardiomyopathies such as cardiac amyloidosis, since there are several problems to consider. In fact, both anatomical factors and the restrictive physiology of this condition make LVAD implant a relevant challenge in this subset of patients. Furthermore, due to the systemic involvement of amyloidosis, several factors have to be considered after LVAD implant, such as an increased risk of bleeding and right ventricular failure. This review attempts to summarize the current evidence of LVAD in cardiac amyloidosis, especially focusing on the challenges that this cardiomyopathy imposes both to the implant and to its management thereafter.


Similar content being viewed by others
Availability of data and materials
Not applicable.
References
Garcia-Pavia P, Rapezzi C, Adler Y et al (2021) Diagnosis and treatment of cardiac amyloidosis: a position statement of the ESC working group on myocardial and pericardial diseases. Eur Heart J 42(16):1554–1568
Adam RD, Coriu D, Jercan A et al (2021) Progress and challenges in the treatment of cardiac amyloidosis: a review of the literature. ESC Heart Fail 8(4):2380–2396
Mohammed SF, Mirzoyev SA, Edwards WD et al (2014) Left ventricular amyloid deposition in patients with heart failure and preserved ejection fraction. JACC Heart Fail 2:113–122
Falk RH (2005) Diagnosis and management of the cardiac amyloidoses. Circulation 112(13):2047–2060
Di Nora C, Livi U (2020) Heart transplantation in cardiac storage diseases: data on Fabry disease and cardiac amyloidosis. Curr Opin Organ Transplant 25(3):211–217
Topilsky Y, Pereira NL, Shah DK, Boilson B, Schirger JA, Kushwaha SS et al (2011) Left ventricular assist device therapy in patients with restrictive and hypertrophic cardiomyopathy. Circ Heart Fail 4(3):266–275
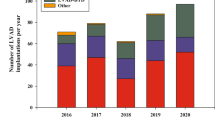
Molina EJ, Shah P, Kiernan MS et al (2021) The society of thoracic surgeons intermacs 2020 annual report. Ann Thorac Surg 111(3):778–792
Gustafsson F, Rogers JG (2017) Left ventricular assist device therapy in advanced heart failure: patient selection and outcomes. Eur J Heart Fail 19(5):595–602
Fukamachi K, Shiose A, Massiello A et al (2013) Preload sensitivity in cardiac assist devices. Ann Thorac Surg 95(1):373–380
Grupper A, Park SJ, Pereira NL et al (2015) Role of ventricular assist therapy for patients with heart failure and restrictive physiology: improving outcomes for a lethal disease. J Heart Lung Transplant 34(8):1042–1049
Pagani FD, Miller LW, Russell SD et al (2009) Extended mechanical circulatory support with a continuous-flowrotary left ventricular assist device. J Am Coll Cardiol 54:312–321
Bellavia D, Iacovoni A, Scardulla C et al (2017) Prediction of right ventricular failure after ventricular assist device implant: systematic review and meta-analysis of observational studies. Eur J Heart Fail 19(7):926–946
Bodez D, Ternacle J, Guellich A et al (2016) Prognostic value of right ventricular systolic function in cardiac amyloidosis. Amyloid 23(3):158–167
Arvidsson S, Henein MY, Wikström G, Suhr OB, Lindqvist P (2018) Right ventricular involvement in transthyretin amyloidosis. Amyloid 25(3):160–166
Patel SR, Saeed O, Naftel D et al (2017) Outcomes of restrictive and hypertrophic cardiomyopathies after LVAD: an INTERMACS analysis. J Card Fail 23(12):859–867
Imamura T, Kinugawa K, Kato N et al (2014) Late-onset right ventricular failure in patients with preoperative small left ventricle after implantation of continuous flow left ventricular assist device. Circ J 78(3):625–633
Vivo RP, Cordero-Reyes AM, Qamar U et al (2013) Increased right-to-left ventricle diameter ratio is a strong predictor of right ventricular failure after left ventricular assist device. J Heart Lung Transplant 32(8):792–799
Topilsky Y, Oh JK, Shah DK et al (2011) Echocardiographic predictors of adverse outcomes after continuous left ventricular assist device implantation. JACC Cardiovasc Imaging 4(3):211–222
Kukucka M, Stepanenko A, Potapov E et al (2011) Right-to-left ventricular end-diastolic diameter ratio and prediction of right ventricular failure with continuous-flow left ventricular assist devices. J Heart Lung Transplant 30(1):64–69
Wan K, Sun J, Han Y et al (2018) Right ventricular involvement evaluated by cardiac magnetic resonance imaging predicts mortality in patients with light chain amyloidosis. Heart Vessels 33(2):170–179
Liu D, Hu K, Herrmann S et al (2017) Value of tissue Doppler-derived Tei index and two-dimensional speckle tracking imaging derived longitudinal strain on predicting outcome of patients with light-chain cardiac amyloidosis. Int J Cardiovasc Imaging 33(6):837–845
Ghio S, Perlini S, Palladini G et al (2007) Importance of the echocardiographic evaluation of right ventricular function in patients with AL amyloidosis. Eur J Heart Fail 9(8):808–813
Bellavia D, Pellikka PA, Al-Zahrani GB et al (2010) Independent predictors of survival in primary systemic (Al) amyloidosis, including cardiac biomarkers and left ventricular strain imaging: an observational cohort study. J Am Soc Echocardiogr 23(6):643–652
Fine NM, White JA, Jimenez-Zepeda V et al (2020) Determinants and prognostic significance of serial right heart function changes in patients with cardiac amyloidosis. Can J Cardiol 36(3):432–440
Wan K, Lin J, Guo X et al (2020) Prognostic value of right ventricular dysfunction in patients with AL amyloidosis: comparison of different techniques by cardiac magnetic resonance. J Magn Reson Imaging 52(5):1441–1448
Maleszewski JJ (2015) Cardiac amyloidosis: pathology, nomenclature, and typing. Cardiovasc Pathol 24(6):343–350
Brenner DA, Jain M, Pimentel DR, Wang B, Connors LH, Skinner M et al (2004) Human amyloidogenic light chains directly impair cardiomyocyte function through an increase in cellular oxidant stress. Circ Res 94(8):1008–1010
Binder C, Duca F, Stelzer PD et al (2019) Mechanisms of heart failure in transthyretin vs. light chain amyloidosis. Eur Heart J Cardiovasc Imaging 20(5):512–524
Cappelli F, Porciani MC, Bergesio F et al (2012) Right ventricular function in AL amyloidosis: characteristics and prognostic implication. Eur Heart J Cardiovasc Imaging 13:416–422
Dungu J, Whelan CJ, Gibbs SD et al (2012) Patterns of late gadolinium enhancement in 94 patients with AL or transthyretin cardiac amyloidosis. J Cardiovasc Magn Reson 14:O87
Phelan D, Collier P, Thavendiranathan P et al (2012) Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart 98:1442–1448
Moñivas Palomero V, Durante-Lopez A, Sanabria MT et al (2019) Role of right ventricular strain measured by two-dimensional echocardiography in the diagnosis of cardiac amyloidosis. J Am Soc Echocardiogr 32(7):845-853.e1
Mehta P, Chapel DB, Goyal N et al (2019) A histopathologic schema to quantify the burden of cardiac amyloidosis: relationship with survival and echocardiographic parameters. Echocardiography 36(2):285–291
Kim D, Choi JO, Kim K, Kim SJ, Kim JS, Jeon ES (2021) Clinical and prognostic implications of capillary density in patients with cardiac light chain amyloidosis. ESC Heart Fail 8(6):5594–5599
Nicol M, Siguret V, Vergaro G et al (2022) Thromboembolism and bleeding in systemic amyloidosis: a review. ESC Heart Fail 9(1):11–20.
Tanaka Y, Hosotani K, Fukushima M (2020) A case of amyloid light-chain amyloidosis presenting with submucosal hematoma and bleeding in the upper gastrointestinal tract. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 18:e158–e159
Sundaram S, Rathod R (2019) Gastric amyloidosis causing nonvariceal upper gastrointestinal bleeding. ACG Case Rep J 6:3–4
Kumar S, Dispenzieri A, Lacy MQ, Litzow MR, Gertz MA (2001) High incidence of gastrointestinal tract bleeding after autologous stem cell transplant for primary systemic amyloidosis. Bone Marrow Transplant 28:381–385
Tabit CE, Chen P, Kim GH, Fedson SE, Sayer G, Coplan MJ, Jeevanandam V, Uriel N, Liao JK (2016) Elevated Angiopoietin-2 level in patients with continuous-flow left ventricular assist devices leads to altered angiogenesis and is associated with higher nonsurgical bleeding. Circulation 134:141–152
Patel SR, Madan S, Saeed O, Algodi M, Luke A, Gibber M, Goldstein DJ, Jorde UP (2016) Association of nasal mucosal vascular alterations, gastrointestinal arteriovenous malformations, and bleeding in patients with continuous-flow left ventricular assist devices. JACC Heart Fail 4:962–970
Swiecicki PL, Edwards BS, Kushwaha SS, Dispenzieri A, Park SJ, Gertz MA (2013) Left ventricular device implantation for advanced cardiac amyloidosis. J Heart Lung Transplant 32(5):563–568
Cappelli F, Tini G, Russo D et al (2020) Arterial thrombo-embolic events in cardiac amyloidosis: a look beyond atrial fibrillation. Amyloid Int J Exp Clin Investig Off J Int Soc Amyloidosis 28:1–7
Imamura T, Burkhoff D, Rodgers D et al (2018) Repeated ramp tests on stable LVAD patients reveal patient-specific hemodynamic fingerprint. ASAIO J 64(6):701–707
Randhawa VK, Gabrovsek A, Soltesz EG et al (2021) A case series of cardiac amyloidosis patients supported by continuous-flow left ventricular assist device. ESC Heart Fail 8(5):4353–4356
Topilsky Y, Pereira NL, Shah DK et al (2011) Left ventricular assist device therapy in patients with restrictive and hypertrophic cardiomyopathy. Circ Heart Fail 4(3):266–275
Author information
Authors and Affiliations
Contributions
CS conceptualized and designed the review. CS, GD, CF, AS, and GEM participated in the writing the manuscript. SV, EG, FD, MF, and MC critically revised the manuscript. All authors provided critical feedback and helped shape the research and manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sciaccaluga, C., De Carli, G., Fusi, C. et al. Left ventricular assist device in cardiac amyloidosis: friend or foe?. Heart Fail Rev 28, 359–365 (2023). https://doi.org/10.1007/s10741-022-10288-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-022-10288-w