Abstract
Purpose
To investigate whether visual acuity improvement achieved after surgical treatment for macular hole (MH) can be predicted by preoperative multifocal ERG (mfERG) central/peripheral amplitude ratio.
Methods
Thirty patients with unilateral MH were included. Evaluations with comprehensive ophthalmological examination including best-corrected visual acuity (BCVA) were performed at baseline and 1, 3, 8, 24 and 48 weeks after surgery, while mfERG (Diagnosys LLC; 61 hexagons—30°) and spectral-domain optic coherence tomography (sOCT—Heidelberg Engineering) were performed at baseline and 2 months after surgery. mfERG results are shown by means of the ratio between the amplitudes’ average from rings 1 and 2 (central) and rings 4 and 5 (peripheral): the P1 ratio. mfERG data from 20 normally sighted age-matched subjects was used for comparison. A macular hole index (MH index) was defined as the quotient between hole height and base measured on OCT.
Results
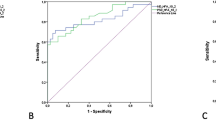
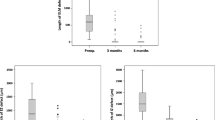
Twenty-six patients finished the 48-week follow-up. Mean ± SE (logMAR) preoperative BCVA was 0.93 ± 0.22 and improved in 0.25 ± 0.07 at 48 weeks. mfERG P1 ratio was reduced at baseline and increased significantly after surgery. A significant correlation was observed between preoperative P1 ratio and BCVA gain at week 8 (r = −0.42; P = 0.033). There was no significant correlation between preoperative MH index and postoperative BCVA (P > 0.05).
Conclusion
Retinal function assessed using the ratio between central and peripheral mfERG responses might be used as predictor of visual acuity outcome after macular surgery for MH.




Similar content being viewed by others
References
Steel DH, Lotery AJ (2013) Idiopathic vitreomacular traction and macular hole: a comprehensive review of pathophysiology, diagnosis, and treatment. Eye (Lond) 27(suppl 1):S1–21
Steel DH, Parkes C, Papastavrou VT, Avery PJ, El-Ghrably IA, Habib MS, Sandinha MT, Smith J, Stannard KP, Vaideanu-Collins D, Hillier RJ (2016) Predicting macular hole closure with ocriplasmin based on spectral domain optical coherence tomography. Eye (Lond) 30:740–745
Grinton ME, Sandinha MT, Steel DH (2015) Photoreceptor outer segment on internal limiting membrane after macular hole surgery: implications for pathogenesis. Case Rep Ophthalmol 6:339–344
Matsumura T, Takamura Y, Tomomatsu T, Arimura S, Gozawa M, Kobori A, Inatani M (2016) Comparison of the inverted internal limiting membrane flap technique and the internal limiting membrane peeling for macular hole with retinal detachment. PLoS ONE 11:e0165068
Jackson TL, Donachie PHJ, Sparrow JM, Johnston RL (2013) United Kingdom national ophthalmology database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology 120:629–634
Tognetto D, Grandin R, Sanguinetti G, Minutola D, Di Nicola M, Di Mascio R, Ravalico G, Hole Surgery Study G (2006) Internal limiting membrane removal during macular hole surgery: results of a multicenter retrospective study. Ophthalmology 113:1401–1410
Nagel E, Franke E, Hary A, Hebenstreit S, Muller E, Richter S (2012) Pars plana vitrectomy for idiopathic macular hole-visual improvement or merely surgical stress? Klin Monbl Augenheilkd 229:48–51
Meng Q, Zhang S, Ling Y, Cui D, Jin Y (2011) Long-term anatomic and visual outcomes of initially closed macular holes. Am J Ophthalmol 151(896–900):e892
Sun Z, Gan D, Jiang C, Wang M, Sprecher A, Jiang AC, Xu G (2012) Effect of preoperative retinal sensitivity and fixation on long-term prognosis for idiopathic macular holes. Graefes Arch Clin Exp Ophthalmol 250(11):1587–1596
Grigoropoulos VG, Theodossiadis GP, Theodossiadis PG (2011) Association of the preoperative photoreceptor layer defect as assessed by optical coherence tomography with the functional outcome after macular hole closure: a long follow-up study. Ophthalmologica 225:47–54
Inoue M, Watanabe Y, Arakawa A, Sato S, Kobayashi S, Kadonosono K (2009) Spectral-domain optical coherence tomography images of inner/outer segment junctions and macular hole surgery outcomes. Graefes Arch Clin Exp Ophthalmol 247:325–330
Landa G, Gentile RC, Garcia PM, Muldoon TO, Rosen RB (2012) External limiting membrane and visual outcome in macular hole repair: spectral domain OCT analysis. Eye (Lond) 26:61–69
Chung SE, Lim DH, Kang SW, Yoon YH, Chae JB, Roh IH (2010) Central photoreceptor viability and prediction of visual outcome in patients with idiopathic macular holes. Korean J Ophthalmol 24(4):213–218
Salter AB, Folgar FA, Weissbrot J, Wald KJ (2012) Macular hole surgery prognostic success rates based on macular hole size. Ophthalmic Surg Lasers Imaging 43:184–189
Almeida DR, Wong J, Belliveau M, Rayat J, Gale J (2012) Anatomical and visual outcomes of macular hole surgery with short-duration 3-day face-down positioning. Retina 32:506–510
Miyake Y, Horiguchi M, Tomita N, Kondo M, Tanikawa A, Takahashi H, Suzuki S, Terasaki H (1996) Occult macular dystrophy. Am J Ophthalmol 122:644–653
Piao CH, Kondo M, Tanikawa A, Terasaki H, Miyake Y (2000) Multifocal electroretinogram in occult macular dystrophy. Invest Ophthalmol Vis Sci 41:513–517
Hood DC, Odel JG, Chen CS, Winn BJ (2003) The multifocal electroretinogram. J Neuroophthalmol 23:225–235
Kim JH, Kim YM, Chung EJ, Lee SY, Koh HJ (2012) Structural and functional predictors of visual outcome of epiretinal membrane surgery. Am J Ophthalmol 153(103–110):e101
Moschos M, Apostolopoulos M, Ladas J, Theodossiadis P, Malias J, Moschou M, Papaspirou A, Theodossiadis G (2001) Multifocal ERG changes before and after macular hole surgery. Doc Ophthalmol 102:31–40
Richter-Mueksch S, Vecsei-Marlovits PV, Sacu SG, Kiss CG, Weingessel B, Schmidt-Erfurth U (2007) Functional macular mapping in patients with vitreomacular pathologic features before and after surgery. Am J Ophthalmol 144:23–31
Chalam KV, Murthy RK, Gupta SK, Brar VS, Grover S (2010) Foveal structure defined by spectral domain optical coherence tomography correlates with visual function after macular hole surgery. Eur J Ophthalmol 20:572–577
Lois N, Burr J, Norrie J, Vale L, Cook J, McDonald A, Boachie C, Ternent L, McPherson G, Full-thickness Macular H, Internal Limiting Membrane Peeling Study G (2011) Internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole: a pragmatic randomized controlled trial. Invest Ophthalmol Vis Sci 52:1586–1592
Ternent L, Vale L, Boachie C, Burr JM, Lois N, Full-thickness Macular H, Internal Limiting Membrane Peeling Study G (2012) Cost-effectiveness of internal limiting membrane peeling versus no peeling for patients with an idiopathic full-thickness macular hole: results from a randomised controlled trial. Br J Ophthalmol 96:438–443
Funding
The study was funded by FAPESP (2011/01449-6).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants
The study protocol adhered to the tenets of the Declaration of Helsinki and was approved by the local Institutional Review Board (3566/2010).
Statement on the welfare of animals
No experiments with animals were made in this study.
Informed consent
All participants gave written informed consent before entering the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moreto, R., De Lucca Perches, A.C.B., Almeida, F. et al. Central mfERG amplitude ratio as a predictor for visual outcome of macular hole surgery. Doc Ophthalmol 140, 23–30 (2020). https://doi.org/10.1007/s10633-019-09716-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-019-09716-4