Abstract
Background
Fluid therapy plays a critical role in the management of acute pancreatitis. Normal saline (NS) is commonly used in these patients. However, Lactate Ringer’s (LR) has also been shown to be useful for this condition.
Aim
To assess the effect of LR compared to NS in patients with acute pancreatitis.
Methods
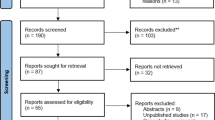
We searched in three electronic databases from inception to December 2020 for randomized controlled trials (RCTs). Outcomes were mortality, intensive care unit (ICU) admission, hospital stay, and Systemic Inflammatory Response Syndrome (SIRS) at 24, 48, and 72 h. The risk of bias was assessed using the Risk of Bias 2.0 tool. All meta-analyses were performed using a random-effects model.
Results
Four RCTs comprising 248 patients were included. The mean age ranged from 42.3 to 63.8 years and 49% of patients were men. Patients treated with LR had similar risk of mortality (risk ratio [RR], 0.53; 95% confidence interval [CI], 0.09–3.00) and SIRS at 24 h (RR, 0.69; 95% CI, 0.32–1.51), 48 h (RR, 0.80; 95% CI, 0.46–1.41), and 72 h (RR, 0.68; 95% CI, 0.37–1.25) compared to NS. LR had significantly lower hospital stay (mean difference, − 1.10; 95% CI, − 1.92 to − 0.28) and lower risk of ICU admission (RR, 0.42; 95% CI, 0.20–0.89) compared to NS. The risk of bias was low in nearly all RCTs.
Conclusion
No differences were found in the mortality and SIRS at 24, 48, and 72 h in patients treated with LR and NS. In contrast, patients who received LR had a lower risk of ICU admission and lower hospital stay than NS.




Similar content being viewed by others
References
Sarles H. Revised classification of pancreatitis–Marseille 1984. Dig Dis Sci 1985;30:573–574. https://doi.org/10.1007/BF01320265.
Toskes PP. Hyperlipidemic pancreatitis. Gastroenterol Clin North Am 1990;19:783–791.
Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Arch Intern Med 2008;168:649–656.
Chatila AT, Bilal M, Guturu P. Evaluation and management of acute pancreatitis. World J Clin Cases 2019;7:1006–1020.
Forsmark CE, Vege SS, Wilcox CM. Acute Pancreatitis. N Engl J Med 2016;375:1972–1981.
Sternby H, Bolado F, Canaval-Zuleta HJ, Marra-López C, Hernando-Alonso AI, Del-Val-Antoñana A, García-Rayado G, Rivera-Irigoin R, Grau-García FJ, Oms L, Millastre-Bocos J, Pascual-Moreno I, Martínez-Ares D, Rodríguez-Oballe JA, López-Serrano A, Ruiz-Rebollo ML, Viejo-Almanzor A, González-de-la-Higuera B, Orive-Calzada A, Gómez-Anta I, Pamies-Guilabert J, Fernández-Gutiérrez-Del-Álam F, Iranzo-González-Cruz I, Pérez-Muñante ME, Esteba MD, Pardillos-Tomé A, Zapater P, de-Madaria E. Determinants of Severity in Acute Pancreatitis: A Nation-wide Multicenter Prospective Cohort Study. Ann Surg 2019;270:348–355.
Knoefel WT, Kollias N, Warshaw AL, Waldner H, Nishioka NS, Rattner DW. Pancreatic microcirculatory changes in experimental pancreatitis of graded severity in the rat. Surgery 1994;116:904–913.
Pandol SJ, Saluja AK, Imrie CW, Banks PA. Acute pancreatitis: bench to the bedside. Gastroenterology 2007;132:1127–1151.
Strate T, Mann O, Kleinhans H, Rusani S, Schneider C, Yekebas E, Freitag M, Standl T, Bloechle C, Izbicki JR. Microcirculatory function and tissue damage is improved after therapeutic injection of bovine hemoglobin in severe acute rodent pancreatitis. Pancreas 2005;30:254–259.
Leppäniemi A, Tolonen M, Tarasconi A, Segovia-Lohse H, Gamberini E, Kirkpatrick AW, Ball CG, Parry N, Sartelli M, Wolbrink D, van Goor H, Baiocchi G, Ansaloni L, Biffl W, Coccolini F, Di Saverio S, Kluger Y, Moore E, Catena F. 2019 WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg 2019;14:27.
de-Madaria E, Herrera-Marante I, González-Camacho V, Bonjoch L, Quesada-Vázquez N, Almenta-Saavedra I, Miralles-Maciá C, Acevedo-Piedra NG, Roger-Ibáñez M, Sánchez-Marin C, Osuna-Ligero R, Gracia Á, Llorens P, Zapater P, Singh VK, Moreu-Martín R, Closa D. Fluid resuscitation with lactated Ringer’s solution vs normal saline in acute pancreatitis: A triple-blind, randomized, controlled trial. United European Gastroenterol J 2018;6:63–72.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898.
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401–406.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135.
Efthimiou O. Practical guide to the meta-analysis of rare events. Evid Based Ment Health 2018;21:72–76.
Choosakul S, Harinwan K, Chirapongsathorn S, Opuchar K, Sanpajit T, Piyanirun W, Puttapitakpong C. Comparison of normal saline versus Lactated Ringer’s solution for fluid resuscitation in patients with mild acute pancreatitis, A randomized controlled trial. Pancreatology 2018;18:507–512.
Lee A, Ko C, Buitrago C, Hiramoto B, Hilson L, Buxbaum J. Lactated Ringers vs Normal Saline Resuscitation for Mild Acute Pancreatitis: A Randomized Trial. Gastroenterology 2021;160:955-957.e954.
Wu BU, Hwang JQ, Gardner TH, Repas K, Delee R, Yu S, Smith B, Banks PA, Conwell DL. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol 2011;9:710-717.e711.
de-Madaria E, Garg PK. Fluid therapy in acute pancreatitis - aggressive or adequate? Time for reappraisal. Pancreatology 2014;14:433–435.
Garg PK, Mahapatra SJ. Optimum Fluid Therapy in Acute Pancreatitis Needs an Alchemist. Gastroenterology 2021;160:655–659.
Siddall E, Khatri M, Radhakrishnan J. Capillary leak syndrome: etiologies, pathophysiology, and management. Kidney Int 2017;92:37–46.
Semler MW, Self WH, Wanderer JP, Ehrenfeld JM, Wang L, Byrne DW, Stollings JL, Kumar AB, Hughes CG, Hernandez A, Guillamondegui OD, May AK, Weavind L, Casey JD, Siew ED, Shaw AD, Bernard GR, Rice TW. Balanced Crystalloids versus Saline in Critically Ill Adults. N Engl J Med 2018;378:829–839.
Bhoomagoud M, Jung T, Atladottir J, Kolodecik TR, Shugrue C, Chaudhuri A, Thrower EC, Gorelick FS. Reducing extracellular pH sensitizes the acinar cell to secretagogue-induced pancreatitis responses in rats. Gastroenterology 2009;137:1083–1092.
Noble MD, Romac J, Vigna SR, Liddle RA. A pH-sensitive, neurogenic pathway mediates disease severity in a model of post-ERCP pancreatitis. Gut 2008;57:1566–1571.
Iqbal U, Anwar H, Scribani M. Ringer’s lactate versus normal saline in acute pancreatitis: A systematic review and meta-analysis. J Dig Dis 2018;19:335–341.
Hoque R, Farooq A, Ghani A, Gorelick F, Mehal WZ. Lactate reduces liver and pancreatic injury in Toll-like receptor- and inflammasome-mediated inflammation via GPR81-mediated suppression of innate immunity. Gastroenterology 2014;146:1763–1774.
Khatua B, Yaron JR, El-Kurdi B, Kostenko S, Papachristou GI, Singh VP. Ringer’s Lactate Prevents Early Organ Failure by Providing Extracellular Calcium. J Clin Med 2020;9:263.
Aziz M, Ahmed Z, Weissman S, Ghazaleh S, Beran A, Kamal F, Lee-Smith W, Assaly R, Nawras A, Pandol SJ, McDonough S, Adler DG. Lactated Ringer's vs normal saline for acute pancreatitis: An updated systematic review and meta-analysis. Pancreatology 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guzmán-Calderón, E., Diaz-Arocutipa, C. & Monge, E. Lactate Ringer’s Versus Normal Saline in the Management of Acute Pancreatitis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Dig Dis Sci 67, 4131–4139 (2022). https://doi.org/10.1007/s10620-021-07269-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07269-8