Abstract
Background
Worse functional status correlates with increased mortality on the liver transplant (LT) waitlist. Whether functional status affects LT outcomes equally across cirrhosis etiologies is unclear.
Aims
We evaluate the impact of functional status on waitlist and post-LT mortality stratified by etiology and age.
Methods
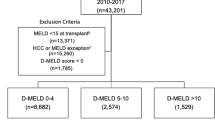
Functional status among US adults from 2005 to 2017 United Network for Organ Sharing LT registry data was retrospectively evaluated using Karnofsky Performance Status Score (KPS-1 = functional status 80–100%, KPS-2 = 60–70%, KPS-3 = 40–50%, KPS-4 = 10–30%). Waitlist and post-LT survival were stratified by KPS and cirrhosis etiology, including alcoholic liver disease (ALD), nonalcoholic steatohepatitis (NASH), hepatitis C (HCV), and HCV/ALD, and evaluated using Kaplan–Meier and multivariate Cox proportional hazard models.
Results
Among 94,201 waitlist registrants (69.4% men, 39.5% HCV, 26.7% ALD, 23.2% NASH), ALD patients had worse functional status compared to HCV (KPS-4: 17.2% vs. 8.3%, p < 0.001). Worse functional status at time of waitlist registration was associated with higher 90-day waitlist mortality with the greatest effect in ALD (KPS-4 vs. KPS-1: ALD HR 2.16, 95% CI 1.83–2.55; HCV HR 2.17, 95% CI 1.87–2.51). Similar trends occurred in 5-year post-LT survival with ALD patients the most harmed. Compared to patients < 50 years, patients ≥ 65 years had increased waitlist mortality at 90-days if they had HCV or HCV/ALD, and 5-year post-LT mortality regardless of cirrhosis etiology with ALD patients most severely affected.
Conclusions
In a retrospective cohort study of patients, US ALD patients had disparately worse functional status at time of LT waitlist registration. Worse functional status correlated with higher risk of waitlist and post-LT mortality, affecting ALD and HCV patients the most.



Similar content being viewed by others
Change history
03 January 2020
The original version of the article unfortunately contained an error in Figure��3. X-axis of Figures��3(a-d) should be ���Time in months���. Corrected version of Figure��3 is given.
Abbreviations
- ALD:
-
Alcoholic liver disease
- ECOG:
-
Eastern Cooperative Oncology Group
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- KPS:
-
Karnofsky Performance Status
- LT:
-
Liver transplantation
- MELD:
-
Model for end-stage liver disease
- OPTN:
-
Organ Procurement and Transplant Network
- UNOS:
-
United Network for Organ Sharing
References
Lai JC, Dodge JL, Sen S, Covinsky K, Feng S. Functional decline in patients with cirrhosis awaiting liver transplantation: results from the functional assessment in liver transplantation (FrAILT) study. Hepatology. 2016;63:574–580.
McCabe P, Wong RJ. More severe deficits in functional status associated with higher mortality among adults awaiting liver transplantation. Clin Transplant. 2018;32:e13346.
Orman ES, Ghabril M, Chalasani N. Poor performance status is associated with increased mortality in patients with cirrhosis. Clin Gastroenterol Hepatol. 2016;14(8):1189.e1–1195.e1.
Samoylova ML, Covinsky KE, Haftek M, Kuo S, Roberts JP, Lai JC. Disability in patients with end-stage liver disease: results from the functional assessment in liver transplantation study. Liver Transpl. 2017;23:292–298.
Tapper EB, Finkelstein D, Mittleman MA, Piatkowski G, Lai M. Standard assessments of frailty are validated predictors of mortality in hospitalized patients with cirrhosis. Hepatology. 2015;62:584–590.
Wang CW, Lebsack A, Chau S, Lai JC. The range and reproducibility of the liver frailty index. Liver Transpl. 2019;25:841–847.
Karnofsky DA, Burchenal J. The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM, ed. evaluation of chemotherapeutic agents. New York: Columbia University Press; 1949.
Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655.
Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148:547–555.
Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the US. Hepatology. 2014;59:2188–2195.
Thuluvath PJ, Thuluvath AJ, Savva Y. Karnofsky performance status before and after liver transplantation predicts graft and patient survival. J Hepatol. 2018;69:818–825.
Malinis MF, Chen S, Allore HG, Quagliarello VJ, et al. Outcomes among older adult liver transplantation recipients in the model of end stage liver disease (MELD) era. Ann Transplant. 2014;19:478–487.
McCabe P, Gish RG, Cheung R, Wong RJ. More severe deficits in performance status at time of liver transplant is associated with significantly higher risk of death following liver transplantation. J Clin Gastroenterol. 2019;53:e392–e399.
Thuluvath PJ, Hanish S, Savva Y. Waiting list mortality and transplant rates for NASH cirrhosis when compared with cryptogenic, alcoholic, or AIH cirrhosis. Transplantation. 2019;103:113–121.
Goldberg D, French B, Abt P, Feng S, Cameron AM. Increasing disparity in waitlist mortality rates with increased model for end-stage liver disease scores for candidates with hepatocellular carcinoma versus candidates without hepatocellular carcinoma. Liver Transpl. 2012;18:434–443.
Trivedi HD, Tapper EB. Interventions to improve physical function and prevent adverse events in cirrhosis. Gastroenterology Report. 2018;6:13–20.
Lucey MR. Liver transplantation in patients with alcoholic liver disease. Liver Transpl. 2011;17:751–759.
Adachi J, Asano M, Ueno Y, et al. Alcoholic muscle disease and biomembrane perturbations (review). J Nutr Biochem. 2003;14:616–625.
Sacanella E, Fernández-Solà J, Cofan M, et al. Chronic alcoholic myopathy: diagnostic clues and relationship with other ethanol-related diseases. QJM. 1995;88:811–817.
Marroni CA, Fleck AM, Fernandes SA, et al. Liver transplantation and alcoholic liver disease: history, controversies, and considerations. World J Gastroenterol. 2018;24:2785–2805.
Grat M, Lewandowski Z, Grąt K, et al. Negative outcomes after liver transplantation in patients with alcoholic liver disease beyond the fifth post-transplant year. Clin Transplant. 2014;28:1112–1120.
Galant LH, Forgiarini Junior LA, Dias AS, Marroni CA. Functional status, respiratory muscle strength, and quality of life in patients with cirrhosis. Brazilian Journal of Physical Therapy. 2012;16:30–34.
Bryce CL, Angus DC, Arnold RM, et al. Sociodemographic differences in early access to liver transplantation services. Am J Transplant. 2009;9:2092–2101.
Shah ND, Cots MV, Zhang C, Zahiragic N. Worldwide lack of early referral of patients with alcoholic liver disease: results of the global alcoholic liver disease survey (GLADIS). J Hepatology. 2017;66:S107–S108.
Ursic-Bedoya J, Faure S, Donnadieu-Rigole H, Pageaux GP. Liver transplantation for alcoholic liver disease: lessons learned and unresolved issues. World J Gastroenterol. 2015;21:10994–11002.
dos Santos DC, Limongi V, Oliveira da Silva AM, et al. Evaluation of functional status, pulmonary capacity, body composition, and quality of life of end-stage liver disease patients who are candidates for liver surgery. Transplant Proc. 2014;46:1771–1774.
Duarte-Rojo A, et al. Exercise and physical activity for patients with end-stage liver disease: Improving functional status and sarcopenia while on the transplant waiting list. Liver Transpl. 2018;24:122–139.
Mizuno Y, et al. Changes in muscle strength and six-minute walk distance before and after living donor liver transplantation. Transplant Proc. 2016;48:3348–3355.
Ow MM, et al. Impaired functional capacity in potential liver transplant candidates predicts short-term mortality before transplantation. Liver Transpl. 2014;20:1081–1088.
Prentis JM, et al. Submaximal cardiopulmonary exercise testing predicts 90-day survival after liver transplantation. Liver Transpl. 2012;18:152–159.
Tandon P, Ney M, Irwin I, Ma M, et al. Severe muscle depletion in patients on the liver transplant wait list: its prevalence and independent prognostic value. Liver Transpl. 2012;18:1209–1216.
Wang CW, Feng S, Covinsky KE, et al. A comparison of muscle function, mass, and quality in liver transplant candidates: results from the functional assessment in liver transplantation study. Transplantation. 2016;100:1692–1698.
Bolondi G, Mocchegiani F, Montalti R, Nicolini D, Vivarelli M, De Pietri L. Predictive factors of short term outcome after liver transplantation: a review. World J Gastroenterol. 2016;22:5936–5949.
Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol. 1984;2:187–193.
Mor V, Laliberte L, Morris JN, Wiemann M. The Karnofsky performance status scale. An examination of its reliability and validity in a research setting. Cancer. 1984;53:2002–2007.
Dunn MA, Josbeno DA, Schmotzer AR, et al. The gap between clinically assessed physical performance and objective physical activity in liver transplant candidates. Liver Transpl. 2016;22:1324–1332.
Wang CW, Lai JC. Reporting functional status in UNOS: the weakness of the Karnofsky performance status scale. Clin Transpl 2017. 31.
Lai JC, Covinsky KE, McCulloch CE, Feng S. The liver frailty index improves mortality prediction of the subjective clinician assessment in patients with cirrhosis. Am J Gastroenterol. 2018;113:235–242.
Lai JC, Covinsky KE, Hayssen H, et al. Author response to: clinical assessments of health status as a potential marker to identify patients who are too sick to undergo transplantation. Liver Int. 2016;36:611.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McCabe, P., Galoosian, A. & Wong, R.J. Patients with Alcoholic Liver Disease Have Worse Functional Status at Time of Liver Transplant Registration and Greater Waitlist and Post-transplant Mortality Which Is Compounded by Older Age. Dig Dis Sci 65, 1501–1511 (2020). https://doi.org/10.1007/s10620-019-05891-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05891-1