Abstract
Objectives
To evaluate rate, recurrence, and predictors of gastrointestinal bleeding (GIB) and impact of endoscopy in left ventricular assist device (LVAD) patients.
Methods
This is a cohort study of all patients who received the current-generation continuous-flow HeartMate II LVAD from 2005 to 2013 at our institution. Patients were followed up, and GIB events recorded until death, time of heart transplantation, or end of observation.
Results
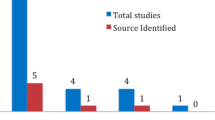
LVAD was implanted in 112 patients (median age 67 years, 88 % male). A total of 44 patients (39 %) had 74 GIB events occurring at a rate of 42.9 per 100 p-y. Endoscopy was performed in 77 % of patients, and GIB source was identified in 57 % with upper GIB found in almost two-third of cases. Right ventricular dysfunction and post-LVAD ejection fraction >30 % were associated with higher GIB rates. Higher pulsatility index was associated with lower GIB rates. Re-bleeding occurred in 19 (43 %) patients at a rate of 62.5 per 100 p-y and was not affected by endoscopic therapy at the index endoscopy.
Conclusions
GIB in LVAD patients is common, occurring primarily in the upper GI tract. Upper endoscopy is the preferred strategy though lower endoscopy is also recommended for a full workup. Endoscopy can identify GIB lesions in about 50 % of patients, but re-bleeding is common. Right ventricular dysfunction and post-LVAD ejection fraction >30 % are associated with higher GIB rates. Higher pulsatility index is associated with lower GIB rates. Reduction in pump speed is a potential strategy for managing and preventing GIB.


Similar content being viewed by others
References
Shrode CW, Draper KV, Huang RJ, et al. Significantly higher rates of gastrointestinal bleeding and thromboembolic events with left Wventricular assist devices. Clin Gastroenterol Hepatol. 2014;12:1461–1467.
Draper KV, Huang RJ, Gerson LB. GI bleeding in patients with continuous-flow left ventricular assist devices: a systematic review and meta-analysis. Gastrointest Endosc. 2014;80:435–446.
Ammar KA, Umland MM, Kramer C. The ABCs of left ventricular assist device echocardiography: a systematic approach. Eur Heart J Cardiovasc Imaging. 2012;13:885–899.
Martin DO, Austin H. Exact estimates for a rate ratio. Epidemiology. 1996;7:29–33.
Klein JP, Moeschberger ML. Survival Analysis Techniques for Censored and Truncated Data. Chapter 13. New York: Springer 1997:405–421.
Elmunzer BJ, Padhya KT, Lewis JJ, et al. Endoscopic findings and clinical outcomes in ventricular assist device recipients with gastrointestinal bleeding. Dig Dis Sci. 2011;56:3241–3246.
Eckman PM, John R. Bleeding and thrombosis in patients with continuous-flow ventricular assist devices. Circulation. 2012;125:3038–3047.
Karimi A, Beaver TM, Hess PJ, et al. Close anti-platelet therapy monitoring and adjustment based upon thrombelastography may reduce late-onset bleeding in HeartMate II recipients. Interact Cardiovasc Thorac Surg. 2014;18:457–465.
Daas A, Small MB, Pinkas H, et al. Safety of conventional and wireless capsule endoscopy in patients supported with nonpulsatile axial flow HeartMate II left ventricular assist device. Gastrointest Endosc. 2008;68:379–382.
Bhat G, Gopalakrishnan M, Aggarwal A. Recent Advances in the Field of Ventricular Assist Devices, Chapter 3—Gastrointestinal Bleeding with Continuous Flow Left Ventricular Assist Devices.Rijeka, Croatia: InTech, 2013:51–65.
Chong AY, Blann AD, Patel J, et al. Endothelial dysfunction and damage in congestive heart failure. Relation of flow-mediated dilation to circulating endothelial cells, plasma indexes of endothelial damage, and brain natriuretic peptide. Circulation. 2004;110:1794–1798.
Omar WP, Selzman CH, Stavros GD, et al. Pulsatility and the risk of nonsurgical bleeding in patients supported with the continuous-flow left ventricular assist device HeartMate II. Circ Heart Fail. 2013;6:517–526.
MacGowan GA, Scheuler S. Right heart failure after left ventricular assist device implantation: early and late. Curr Opin Cardiol. 2012;27:296–300.
Topkara VK, Kondareddy S, Malik F, et al. Infectious complications in patients with left ventricular assist device: etiology and outcomes in the continuous-flow era. Ann Thorac Surg. 2010;90:1270–1277.
Matthews JC, Koelling TM, Pagani FD, et al. The right ventricular failure risk score a pre-operative tool for assessing the risk of right ventricular failure in left ventricular assist device candidates. J Am Coll Cardiol. 2008;51:2163–2172.
Samsky MD, Patel CB, DeWald TA, et al. Cardiohepatic interactions in heart failure: an overview and clinical implications. J Am Coll Cardiol. 2013;61:2397–2405.
Moller S, Bernardi M. Interactions of the heart and the liver. Eur Heart J. 2013;34:2804–2811.
Krim S, Vivo R, Cordero-Reyes A et al. Total bilirubin/albumin ratio has an independent and incremental role in predicting right ventricular failure after left ventricular assist device implantation. J Am Coll Cardiol. 2013;61.
Czul F, Barkin J. Continuous-flow left ventricular assist devices as a cause of acquired von Willebrand syndrome and GI bleeding. Gastrointest Endosc. 2015;81:776–777.
Kushnir VM, Sharma S, Ewald GA, et al. Evaluation of GI bleeding after Implantation of left ventricular assist device. Gastrointest Endosc. 2012;75:973–979.
Aggarwal A, Pant R, Kumar S, et al. Incidence and management of gastrointestinal bleeding with continuous flow assist devices. Ann Thoracic Surg. 2012;93:1534–1540.
Demirozu ZT, Radovancevic R, Hochman LF, et al. Arteriovenous malformations and gastrointestinal bleeding in patients with HeartMate II Left ventricular assist device. J Heart Lung Transplant. 2011;30:849–853.
Morgan JA, Paone G, Nemeh HW, et al. Gastrointestinal bleeding with the HeartMate II for left ventricular assist device. J Heart Lung Transplant. 2012;31:715–718.
Stern DR, Kazam J, Edwards P, et al. Increased incidence of gastrointestinal bleeding following implantation of the HeartMate II LVAD. J Card Surg. 2012;25:352–356.
Lestou GV, Shah N, Gregoric ID, et al. Gastrointestinal bleeding from arteriovenous malformations in patients supported by the Jarvik 2000 axial flow left ventricular assist device. J Heart Lung Transplant. 2005;24:105–109.
Uriel N, Pak SW, Jorde UP, et al. Acquired von Willebrand syndrome after continuous flow mechanical device support contributes to a high prevalence of bleeding during long-term support and at the time of transplantation. J Am Coll Cardiol. 2010;56:1207–1213.
John R, Kamdar F, Eckman P et al. Lessons learned from experience with over 100 consecutive HeartMate II left ventricular assist devices. Ann Thorac Surg 2011:92:1593–1599; discussion 1599–1600.
Crow S, Chen D, Milano C et al. Acquired von Willebrand syndrome in continuous flow ventricular assist device recipients: Ann Thorac Surg 2010:90:1263–1269; discussion 1269.
Crow S, John R, Boyle A, et al. Gastrointestinal bleeding rates in recipients of nonpulsatile and pulsatile left ventricular assist devices. J Thorac Cardiovasc Surg. 2009;137:208–215.
Heyde EC. Gastrointestinal bleeding in aortic stenosis. N Engl J Med. 1958;259:196.
Islam S, Cevik C, Islam E, et al. Heyde’s syndrome: a critical review of the literature. J Heart Valve Dis. 2011;20:366–375.
Boley SJ, Sammartano R, Adams A, et al. On the nature and etiology of vascular ectasias of the colon. Degenerative lesions of aging. Gastroenterology. 1977;72:650–660.
Klovaite J, Gustafson F, Mortensen SA, et al. Severely impaired von Willebrand’s factor-dependent platelet aggregation in patients with a continuous flow left ventricular assist device (HeartMate II). J Am Coll Cardiol. 2009;53:2162–2167.
Slaughter MS. Hematologic effects of continuous flow left ventricular assist devices. J CardiovascTransl Res. 2010;3:618–624.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jabbar, H.R., Abbas, A., Ahmed, M. et al. The Incidence, Predictors and Outcomes of Gastrointestinal Bleeding in Patients with Left Ventricular Assist Device (LVAD). Dig Dis Sci 60, 3697–3706 (2015). https://doi.org/10.1007/s10620-015-3743-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3743-4