Abstract
The pervasive impact of trauma across populations and stages of life has made it imperative that the field of social work remain at the forefront of trauma-informed theory, research, and practice. The limited, adjunctive use of 3,4-methylenedioxymethamphetamine (MDMA) in the psychotherapeutic treatment of posttraumatic stress disorder (PTSD) is a promising new treatment model that has shown impressive efficacy in phase I and II clinical trials. Preliminary meta-analysis suggests that MDMA-assisted psychotherapy (MDMA-PT) may be superior to prolonged exposure, a first-line treatment for PTSD, and the U.S. Food and Drug Administration (FDA) has granted the treatment “breakthrough therapy” designation, a process of expedited review which signals that a treatment may demonstrate substantial improvement over existing therapies. Though these results are encouraging, much remains unknown and it is essential that the field of social work become informed and engaged in this new body of research. This paper will review the existing literature on MDMA-PT for PTSD, examine ethical and safety concerns, present a preliminary conceptualization of MDMA-PT’s impact on the therapeutic process, and discuss implications for future social work research and practice. This paper finds that the current literature suggests that MDMA-PT is a safe and efficacious treatment that has the potential to revolutionize the treatment of trauma. At the same time, issues of safety, cost, and accessibility should be examined in depth to ensure that this treatment—if approved by the FDA—is accessible to racially and economically marginalized clients.
Similar content being viewed by others
Notes
All subjects at study entry had retained a CAPS score of 50 (signifying moderate to severe symptoms) following at least 3 months of prior pharmacological treatment in addition to at least 6 months of psychotherapy. Mean duration of PTSD was 19 years.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: American Psychiatric Publishing.
Amoroso, T., & Workman, M. (2016). Treating posttraumatic stress disorder with MDMA-assisted psychotherapy: A preliminary meta-analysis and comparison to prolonged exposure therapy. Journal of Psychopharmacology, 30(7), 595–600.
Bentley, K. J., Walsh, J., & Farmer, R. L. (2005). Social work roles and activities regarding psychiatric medication: Results of a national survey. Social Work, 50(4), 295–303.
Benzenhöfer, U., & Passie, T. (2010). Rediscovering MDMA (ecstasy): The role of the American chemist Alexander T. Shulgin. Addiction, 105(8), 1355–1361.
Bouso, J. C., Doblin, R., Farré, M., Alcázar, M., & Gómez-Jarabo, G. (2008). MDMA-Assisted psychotherapy using low doses in a small sample of women with chronic posttraumatic stress disorder. Journal of Psychoactive Drugs, 40(3), 225–236.
Charuvastra, A., & Cloitre, M. (2008). Social bonds and posttraumatic stress disorder. Annual Review of Psychology, 59(1), 301–328.
Clark, R. (2011). Why don’t more people use this drug? Myths, policy, and evidence. Presented at the University of Massachusetts Clinical and Translational Science Retreat, Shrewsbury, MA.
Cozolino, L. (2017). The neuroscience of psychotherapy: Healing the social brain. New York: W.W. Norton & Company.
Danforth, A. L., Struble, C. M., Yazar-Klosinski, B., & Grob, C. S. (2016). MDMA-assisted therapy: A new treatment model for social anxiety in autistic adults. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 64, 237–249.
de la Torre, R., Farré, M., Roset, P. N., Pizarro, N., Abanades, S., Segura, M., Segura, J., & Cami, J. (2004). Human pharmacology of MDMA: Pharmacokinetics, metabolism, and disposition. Therapeutic Drug Monitoring, 26(2), 137–144.
Domes, G., Heinrichs, M., Gläscher, J., Büchel, C., Braus, D. F., & Herpertz, S. C. (2007). Oxytocin attenuates amygdala responses to emotional faces regardless of valence. Biological Psychiatry, 62(10), 1187–1190.
Doukas, A., D’Andrea, W., Doran, J., & Pole, N. (2014). Psychophysiological predictors of working alliance among treatment-seeking women with complex trauma exposure. Journal of Traumatic Stress, 27(6), 672–679.
Drug Enforcement Administration. (1988). Schedules of controlled substances; scheduling of 3,4-methylenedioxymethamphetamine (MDMA) into schedule I of the Controlled Substances Act; Remand. Federal Register, 53(34), 5156–5158.
Egan, M., Combs-Orme, T., & Neely-Barnes, S. L. (2011). Integrating neuroscience knowledge into social work education: A case-based approach. Journal of Social Work Education, 47(2), 269–282.
Emerson, A. (2016). Treating PTSD with MDMA-assisted psychotherapy: Product development status and proposed design for phase 3 clinical trials. MAPS Bulletin Annual Report, 26, 26–29.
Ensink, K., Berthelot, N., Bégin, M., Maheux, J., & Normandin, L. (2017). Dissociation mediates the relationship between sexual abuse and child psychological difficulties. Child Abuse & Neglect, 69, 116–124.
Erskine, R. G. (1998). Attunement and involvement: Therapeutic responses to relational needs. International Journal of Psychotherapy, 3(3), 235–244.
Etkin, A., & Wager, T. D. (2007). Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. American Journal of Psychiatry, 164(10), 1476–1488.
Feduccia, A. A., Holland, J., & Mithoefer, M. C. (2018). Progress and promise for the MDMA drug development program. Psychopharmacology (Berl), 235(2), 561–571.
Foa, E. B., Hembree, E., & Rothbaum, B. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences, therapist guide. Oxford: Oxford University Press.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. (2009). Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. New York: Guilford Press.
Ford, J. G., Howerton, M. W., Lai, G. Y., Gary, T. L., Bolen, S., Gibbons, M. C., Tilburt, J., Baffi, C., Tanpitukpongse, T. P., Wilson, R. F., Power, N. R., & Bass, E. B. (2007). Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer, 112(2), 228–242.
Gamma, A., Buck, A., Berthold, T., Liechti, M., & Vollenweider, F. (2000). Methylenedioxymethamphetamine (MDMA) modulates cortical and limbic brain activity as measured by [H(2)(15)O]-PET in healthy humans. Neuropsychopharmacology, 23(4), 388–395.
Glassman, A. H., & Bigger, J. T. (2001). Antipsychotic drugs: prolonged QTc interval, torsade de pointes, and sudden death. American Journal of Psychiatry, 158(11), 1774–1782.
Greenberg, P. E., Sisitsky, T., Kessler, R. C., Finkelstein, S. N., Berndt, E. R., Davidson, J. R., Ballenger, J. C., & Fyer, A. J. (1999). The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatiry, 60, 427–435.
Greer, G., & Tolbert, R. (1986). Subjective reports of the effects of MDMA in a clinical setting. Journal of Psychoactive Drugs, 18(4), 319–327.
Greer, G., & Tolbert, R. (1998). A method of conducting therapeutic sessions with MDMA. Journal of Psychoactive Drugs, 30(4), 371–379.
Grob, C. (1998). MDMA research: Preliminary investigations with human subjects. International Journal of Drug Policy, 9(2), 119–124.
Gutner, C. A., Gallagher, M. W., Baker, A. S., Sloan, D. M., & Resick, P. A. (2016). Time course of treatment dropout in cognitive–behavioral therapies for post traumatic stress disorder. Psychological Trauma, 8(1), 115–121.
Hampton, L. M., Daubresse, M., Chang, H. Y., Alexander, G. C., & Budnitz, D. S. (2014). Emergency department visits by adults for psychiatric medication adverse events. JAMA Psychiatry, 71(9), 1006–1014.
Hauner, K. K., Mineka, S., Voss, J. L., & Paller, K. A. (2012). Exposure therapy triggers lasting reorganization of neural fear processing. Proceedings of the National Academy of Sciences, 109(23), 9203–9208.
Heifets, B. D., & Malenka, R. C. (2016). MDMA as a probe and treatment for social behaviors. Cell, 166(2), 269–272.
Herkt, D., Tumani, V., Grön, G., Kammer, T., Hofmann, A., & Abler, B. (2014). Facilitating access to emotions: Neural signature of EMDR stimulation. PLoS ONE. 9(8), e106350.
Herman, J. L. (1997). Trauma and recovery. New York: BasicBooks.
Hill, D. (2015). Affect regulation theory: A clinical model. New York: W.W. Norton & Company.
Holland, J. (2001). Ecstasy: The complete guide. Rochester: Park Street Press.
Institute of Medicine. (2008). Treatment of posttraumatic stress disorder: An assessment of the evidence. Washington, DC: The National Academies Press.
Jeffreys, M. (2018). Clinician’s guide to medications for PTSD. Retrieved from https://www.ptsd.va.gov/professional/treatment/overview/clinicians-guide-to-medications-for-ptsd.asp.
Jerome, L., Schuster, S., & Yazar-Klosinski, B. (2013). Can MDMA play a role in the treatment of substance abuse? Current Drug Abuse Reviews, 6(1), 54–62.
Johansen, P., & Krebs, T. (2009). How could MDMA (ecstasy) help anxiety disorders? A neurobiological rationale. Journal of Psychopharmacology, 23(4), 389–391.
Kessler, R. C. (2000). Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry, 61(Suppl. 5), 4–12.
Kessler, R. C., Somega, A., Bromet, E., Huges, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048.
Kodjack, A. (2016). Obama administration eases restrictions on doctors who treat opioid addiction. NPR. Retrieved from https://www.npr.org/sections/health-shots/2016/07/06/484843560/obama-administration-eases-restrictions-on-doctors-who-treat-opioid-addiction.
Lyons-Ruth, K. (2003). Dissociation and the parent-infant dialogue: A longitudinal perspective from attachment research. Journal of the American Psychoanalytic Association, 51(3), 883–911.
Mak, W. W. S., Law, R. W., Alvidrez, J., & Pérez-Stable, E. J. (2007). Gender and ethnic diversity in NIMH-funded clinical trials: Review of a decade of published research. Administrative Policy in Mental Health, 34, 497–503.
McGuire, T. G., & Miranda, J. (2008). Racial and ethnic disparities in mental health care: Evidence and policy implications. Health Affairs, 27(2), 393–403.
Meltzer, H. Y., Davidson, M., Glassman, A. H., & Vieweg, W. V. (2002). Assessing cardiovascular risks versus clinical benefits of atypical antipsychotic drug treatment. Journal of Clinical Psychiatry, 63(9), 25–29.
Miller, D. D. (2004). Atypical antipsychotics: Sleep, sedation, and efficacy. Primary Care Companion to the Journal of Clinical Psychiatry, 6(suppl 2), 3–7.
Mithoefer, M. C., Grob, C. S., & Brewerton, T. D. (2016). Novel psychopharmacological therapies for psychiatric disorders: Psilocybin and MDMA. The Lancet Psychiatry, 3(5), 481–488.
Mithoefer, M. C., Mithoefer, A., Jerome, L., Ruse, J., Doblin, R., Gibson, E., Ot’aulora, M. G., & Sola, E. (2017). A manual for MDMA-assisted psychotherapy in the treatment of PTSD. Retrieved from https://s3-us-west-1.amazonaws.com/mapscontent/research-archive/mdma/TreatmentManual_MDMAAssistedPsychotherapyVersion+8.1_22+Aug2017.pdf.
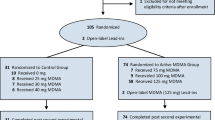
Mithoefer, M. C., Mithoefer, A. T., Feduccia, A. A., Jerome, L., Wagner, M., Wymer, J., Holland, J., Hamilton, S., Yazar-Klosinski, B., Emerson, A., & Doblin, R. (2018). 3, 4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy for post-traumatic stress disorder in military veterans, firefighters, and police officers: A randomised, double-blind, dose-response, phase 2 clinical trial. The Lancet Psychiatry, 5(6), 486–497.
Mithoefer, M. C., Wagner, M. T., Mithoefer, A. T., Jerome, L., & Doblin, R. (2011). The safety and efficacy of ± 3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant Posttraumatic stress disorder: The first randomized controlled pilot study. Journal of Psychopharmacology, 25(4), 439–452.
Mithoefer, M. C., Wagner, M. T., Mithoefer, A. T., Jerome, L., Martin, S. F., Yazar-Klosinski, B., Michael, Y., Brewerton, T. D., & Doblin, R. (2013). Durability of improvement in post-traumatic stress disorder symptoms and absence of harmful effects or drug dependency after 3,4-methylenedioxymethamphetamine-assisted psychotherapy: A prospective long-term follow-up study. Journal of Psychopharmacology, 27(1), 28–39.
Morina, N., Wicherts, J. M., Lobbrecht, J., & Priebe, S. (2014). Remission from post-traumatic stress disorder in adults: A systematic review and meta-analysis of long term outcome studies. Clinical Psychology Review, 34, 249–255.
Multidisciplinary Association for Psychedelic Studies (MAPS). (2017). Press release: FDA grants breakthrough therapy designation for MDMA-assisted psychotherapy for PTSD, agrees on special protocol assessment for phase 3 trials. Retrieved from https://www.maps.org/news/media/6786-press-release-fda-grants-breakthrough-therapy-designation-for-mdma-assisted-psychotherapy-for-ptsd,-agrees-on-special-protocol-assessment-for-phase-3-trials.
Multidisciplinary Association for Psychedelic Studies (MAPS). (2018). Documents from the DEA scheduling hearing of MDMA, 1984–1988. Retrieved from http://www.maps.org/index.php?option=com_content&view=article&id=5378.
National Association of Social Workers (NASW). (2008). Code of ethics of the National Association of Social Workers. Washington, DC: NASW Press.
National Association of Social Workers. (2016). NASW standards for social work practice in health care settings. Retrieved from https://www.socialworkers.org/LinkClick.aspx?fileticket=fFnsRHX-4HE%3D&portalid=0.
Nichols, D. E. (1986). Differences between the mechanism of action of MDMA, MBDB, and the classic hallucinogens. Identification of anew therapeutic class: Entactogens. Journal of Psychoactive Drugs, 18, 305–313.
Oehen, P., Traber, R., Widmer, V., & Schnyder, U. (2013). A randomized, controlled pilot study of MDMA (± 3,4-Methylenedioxymethamphetamine)-assisted psychotherapy for treatment of resistant, chronic post-traumatic stress disorder (PTSD). Journal of Psychopharmacology, 27(1), 40–52.
Ogden, P., Minton, K., & Pain, C. (2006). Trauma and the body: A sensorimotor approach to psychotherapy. New York: W.W. Norton.
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25(3), 456–465.
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2013). Physical health conditions associated with Posttraumatic Stress Disorder in U.S. older adults: Results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of the American Geriatrics Society, 60(2), 296–303.
Platt, A. (2014). Suboxone: A harm reduction approach. Alcoholism and Drug Dependence, 2(5), 1000.
Ramchand, R., Rudavsky, R., Grant, S., Tanielian, T., & Jaycox, L. (2015). Prevalence of, risk factors for, and consequences of posttraumatic stress disorder and other mental health problems in military populations deployed to Iraq and Afghanistan. Current Psychiatry Reports, 17(5), 37.
Resick, P. A., Monson, C. M., & Chard, K. M. (2017). Cognitive Processing Therapy for PTSD: A comprehensive manual. New York: Guilford Press.
Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2010). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41(01), 71–83.
Shapiro, F. (2001). Eye Movement Desensitization and Reprocessing: Basic principles, protocols, and procedures (2nd ed.). New York: Guilford Press.
Shulgin, A. T., & Nichols, D. E. (1978). Characterization of three new psychotomimetics. In R. C. Stillman & R. E. Willette (Eds.), The Pharmacology of Hallucinogens. New York: Pergamon.
Shulgin, A. T., & Shulgin, A. (1995). PiHKAL: A chemical love story. Berkeley: Transform Press.
Slopen, N., Shonkoff, J. P., Albert, M. A., Yoshikawa, H., Jacobs, A., Stoltz, R., & Williams, D. R. (2016). Racial disparities in child adversity in the U.S.: Interactions with family immigration history and income. American Journal of Preventive Medicine, 50(1), 47–56.
Smart, A. (2006). A multi-dimensional model of clinical utility. International Journal for Quality in Health Care, 18(5), 377–382.
Steenkamp, M. M., Tiz, B. T., Hoge, C. W., & Marmar, C. R. (2015). Psychotherapy for military-related PTSD: A review of randomized clinical trials. JAMA, 314(5), 489–500.
Szafranski, D. D., Gros, D. F., Menefee, D. S., Norton, P. J., & Wanner, J. L. (2015). Treatment adherence: An examination of why OEF/OIF/OND veterans discontinue inpatient PTSD treatment. Military Behavioral Health, 4(1), 25–31.
Templer, D. I., Arikawa, H., & Gariety, P. C. (2004). Psychotropic drugs in terminally ill patients: A review of the clinical and research literature. OMEGA - Journal of Death and Dying, 49(3), 249–274.
U.S. Department of Veterans Affairs (2016). How common is PTSD? Retrieved May 5, 2018 from http://www.ptsd.va.gov/public/PTSD-overview/basics/how-common-is-ptsd.asp.
U.S. Department of Veterans Affairs. (2017a). Prolonged exposure for PTSD. Retrieved June 2, 2018 from http://www.ptsd.va.gov/public/treatment/therapy-med/prolonged-exposure-therapy.asp.
U.S. Department of Veterans Affairs. (2017b). Cognitive processing therapy for PTSD. Retrieved May 2, 2018 from http://www.ptsd.va.gov/public/treatment/therapy-med/cognitive_processing_therapy.asp.
U. S. Food and Drug Administration. (2018). Fact sheet: Breakthrough therapies. Retrieved February 17, 2018 from https://www.fda.gov/RegulatoryInformation/LawsEnforcedbyFDA/SignificantAmendmentstotheFDCAct/FDASIA/ucm329491.htm.
Vandiver, V. (Ed.). (2013). Best Practices in Community Mental Health. New York: Oxford University Press.
Walpola, I. C., Nest, T., Roseman, L., Erritzoe, D., Fielding, A., Nutt, D. J., & Carhart-Harris, R. L. (2017). Alerted insulta connectivity under MDMA. Neuropsychopharmacology, 42(11), 2152–2162.
Zak, P. J., Kurzban, R., & Matzner, W. T. (2005). Oxytocin is associated with human trustworthiness. Hormones and Behavior, 48, 522–527.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research Involving in Human Participants
Research on human subjects were not involved in this manuscript.
Rights and permissions
About this article
Cite this article
Hutchison, C.A., Bressi, S.K. MDMA-Assisted Psychotherapy for Posttraumatic Stress Disorder: Implications for Social Work Practice and Research. Clin Soc Work J 48, 421–430 (2020). https://doi.org/10.1007/s10615-018-0676-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10615-018-0676-3