Abstract
While colorectal and gastroesophageal cancer represent the two gastrointestinal (GI) tumor entities with the highest incidence of brain metastatic (BM) disease, data on the clinical course of BM patients from hepatopancreatobiliary malignancies are rare. Patients with cholangiocarcinoma (CCA), hepatocellular carcinoma (HCC), pancreatic ductal adenocarcinoma (PDAC) and gastroenteropancreatic neuroendocrine neoplasms (GEP NEN). Treated for BM between 1991 and 2017 at an academic care center were included. Brain metastases-free survival (BMFS) was defined as interval from first diagnosis until BM development. Overall survival (OS) was defined as interval from diagnosis of BM until death or last date of follow-up. Outcome was correlated with clinical and treatment factors. 29 patients from overall 6102 patients (0.6%) included in the Vienna Brain Metastasis Registry presented with BM from hepatopancreatobiliary primaries including 9 (31.0%) with CCA, 10 (34.5%) with HCC, 7 (24.1%) with PDAC and 3 (10.3%) with GEP NEN as primary tumor. Median BMFS was 21, 12, 14 and 7 months and median OS 4, 4, 6 and 4 months, respectively. Karnofsky Performance Status (KPS) below 80% (p = 0.08), age above 60 years (p = 0.10) and leptomeningeal carcinomatosis (LC) (p = 0.09) diagnosed concomitant to solid BM showed an inverse association with median OS (Cox proportional hazards model). In this cohort of patients with BM from hepatopancreatobiliary tumor entities, prognosis was shown to be very limited. Performance status, age and diagnosis of LC were identified as negative prognostic factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The incidence of brain metastatic (BM) disease is increasing among several tumor entities potentially due to better diagnostic modalities and an improved control of extracranial disease achieved by systemic therapies [1, 2]. Lung cancer, breast cancer and melanoma patients thereby exhibit the highest incidence of BM with up to 50%, 15% and 10%, respectively and therefore available data on the clinical course of disease of these patients in the meanwhile seem well explored [1, 3, 4]. The prognosis of patients with BM varies extensively not only between different tumor entities, but even between distinct tumor subtypes. Age, performance status, presence or absence of extracranial metastases as well as number of BM were shown to represent the most important clinical prognosticators of survival in these patients as described by the Graded Prognostic Assessment (GPA) score [5].
Since patients with gastrointestinal (GI) primary tumors represent approximately only 6% of BM patients, clinical data is very limited. Patients with colorectal and gastroesophageal tumors are most likely to develop BM lesions throughout their course of disease [6]. Once BM are diagnosed in these patients, overall survival (OS) remains very limited with a median of 8 months among all GI primaries. Here, the same clinical biomarkers as in breast, lung and melanoma patients were recently identified as independent prognosticators for OS, which has been summarized within the graded prognostic assessment for gastrointestinal cancers (GI-GPA) [7]. However, other primary GI tumors beside colorectal and gastroesophageal cancer have been barely investigated and therefore data on these patients remain scarce after diagnosis of BM.
Within the present study we therefore aimed to describe the clinical characteristics as well as the outcome of patients with BM from rare GI cancer treated at our tertiary care center. We took advantage of the joined focus on GI cancers as well as the Vienna Brain Metastasis Registry to identify patients with GI cancers less frequently developing BM compared to colorectal and gastroesophageal tumors. We investigated clinical risk factors and different BM therapies associated with OS. We thereby focused on patients with cholangio- (CCA), hepatocellular (HCC) and pancreatic ductal adenocarcinoma (PDAC) as well as gastroenteropancreatic neuroendocrine neoplasms (GEP NEN).
Methods
Patients
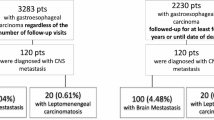
From 6102 patients with BM registered in the Vienna Brain Metastasis Registry, 34 patients (0.6%) had a CCA, HCC, PDAC or GEP NEN as primary tumor. After exclusion of patients with missing clinical data, 29 patients remained for the final analysis of this study (Fig. 1). All of these patients were treated between 1991 and 2017 at the Medical University of Vienna. If leptomeningeal carcinomatosis (LC) was present concomitantly to diagnosis of parenchymal BM, patients were also eligible for inclusion. Information relating to patient demographics, case history, and survival was collected by retrospective chart review. This study was conducted in accordance with the Declaration of Helsinki and approval by the institutional review board (IRB) was obtained (1167/2019).
All patients were managed by a dedicated team of GI cancer and BM specialists. Treatment was performed according to best clinical evidence and according to current standard of care at the respective time.
Statistical analysis
The primary aim of this study was to describe the clinical characteristics of a cohort of hepatopancreatobiliary cancer patients (CCA, HCC, PDAC, GEP NEN) with BM in a descriptive manner. The secondary aim was to identify prognostic clinical factors with regards to patient’s outcome after diagnosis of BM as well as to compare different BM therapies. Brain metastases-free survival (BMFS) was defined as the interval from diagnosis of GI cancer until diagnosis of BM. OS was defined as interval from first diagnosis of BM until death or last date of follow-up. Both endpoints were estimated with the Kaplan–Meier product limit method. To test for differences between survival curves, the log-rank test was used. Two-tailed p values < 0.05 were considered to indicate statistical significance.
The recently updated GI-GPA including KPS (< 80, 80, 90–100), age (< 60, ≥ 60 years), extracranial metastases (present, absent) and number of BM (1, 2–3, > 3) represents the so far best established prognosticator of outcome in GI BM patients [7]. Therefore, we predefined a priori the inclusion of these 4 clinical parameters together with the GI-GPA as well as other important clinical parameters (gender, visceral metastases, tumor entity, status of extracranial disease at diagnosis of BM, symptomatic BM, LC) into the multivariate model, depending on their significance in the univariate analysis. A multivariate analysis was performed using the Cox Regression model. Due to the exploratory and hypothesis-generating design of the present study, no adjustment for multiple testing was applied and no formal sample-size calculation was conducted [8]. All statistics were calculated using statistical package for the social sciences (SPSS®) 28.0 software (SPSS Inc., Chicago, IL, USA).
Results
Among 6102 patients with BM from the Vienna Brain Metastasis Registry 474 (7.8%) presented with a GI primary tumor. 440 patients with colorectal or gastroesophageal primaries and 5 patients with incomplete data were excluded. Therefore, 29 patients were available for the present study comprising 9 patients with CCA (31.0%), 10 patients with HCC (34.5%), 7 patients with PDAC (24.1%) and 3 patients with GEP NEN (10.3%) as primary tumor diagnosis (Fig. 1). BM were diagnosed in 4/29 patients (13.8%) before the year 2000, in 7/29 patients (24.1%) between 2000 and 2010 and in 18/29 patients (62.1%) after the year 2010. Median BMFS was 18 months (range 0 to 111) among all included patients. Median OS from first diagnosis was 21 months (range 1 to 115), from diagnosis of metastatic disease 16 months (range 0 to 71) and from diagnosis of BM 4 months (range 0 to 29).
CCA patients
Median age of CCA patients at diagnosis of BM was 69 years (range 52 to 76) and median KPS 70% (range 40 to 80). Patients had a median number of 1 extracranial metastatic site (range 0 to 3) at diagnosis of BM and were treated with a median number of 1 line of systemic therapy (range 0 to 3) before. Before diagnosis of BM, liver metastases were present in 4/9 patients (44.4%), lung metastases in 4/9 patients (44.4%) and peritoneal metastases in 1/9 patients (11.1.%). At diagnosis of BM, extracranial disease was progressive in 5/9 patients (55.6%), stable in 1/9 patients (11.1%) and in remission in 3/9 patients (33.3%). All 9 patients (100.0%) were symptomatic with regards to BM diagnosis. Median number of BM lesions was 1 (range 1 to 4). 2/9 patients (22.2%) presented with LC concomitant to solid BM diagnosis. CCA patient characteristics are listed within Table 1. Median BMFS was 21 months (range 0 to 34) and median OS 4 months (range 0 to 7) (Fig. 2).
Kaplan–Meier curves of A brain metastasis-free survival (BMFS) and B overall survival (OS) according to different tumor entities (BMFS brain metastasis-free survival, CCA cholangiocarcinoma, GEP NEN gastroenteropancreatic neuroendocrine neoplasm, HCC hepatocellular carcinoma, OS overall survival, PDAC pancreatic ductal adenocarcinoma)
HCC patients
Median age of HCC patients at diagnosis of BM was 61 years (range 48 to 81) and median KPS 80% (range 50 to 90). Patients had a median number of 0 extracranial metastatic sites (range 0 to 3) at diagnosis of BM and were treated with a median number of 0 lines of systemic therapy (range 0 to 3) before. Before diagnosis of BM, liver metastases were present in 3/10 patients (30.0%), lung metastases in 3/10 patients (30.0%) and peritoneal metastases in 0/10 patients (0.0%). At diagnosis of BM, extracranial disease was progressive in 4/10 patients (44.4%), stable in 3/10 patients (33.3%) and in remission in 2/10 patients (22.2%) (1 unknown). Six/10 patients (60.0%) were symptomatic and 4/10 patients (40.0%) asymptomatic with regards to BM diagnosis. Median number of BM lesions was 1 (range 1 to 4). One/10 patients (10.0%) presented with LC concomitant to solid BM diagnosis. HCC patient characteristics are listed within Table 1. Median BMFS was 12 months (range 0 to 111) and median OS 4 months (range 0 to 29) (Fig. 2).
PDAC patients
Median age of PDAC patients at diagnosis of BM was 64 years (range 44 to 82) and median KPS 80% (range 60 to 90). Patients had a median number of 1 extracranial metastatic site (range 0 to 3) at diagnosis of BM and were treated with a median number of 1 line of systemic therapy (range 0 to 6) before. Before diagnosis of BM, liver metastases were present in 1/7 patients (16.7%, 1 missing), lung metastases in 2/7 patients (33.3, 1 missing) and peritoneal metastases in 0/7 patients (0.0%, 1 missing). At diagnosis of BM, extracranial disease was progressive in 4/7 patients (66.7%), stable in 1/7 patients (16.7%) and in remission in 1/7 patients (16.7%) (1 unknown). All of the 7 patients (100.0%) were symptomatic with regards to BM diagnosis. Median number of BM lesions was 3 (range 1 to 10). One/7 patients (14.3%) presented with LC concomitant to solid BM diagnosis. PDAC patient characteristics are listed within Table 1. Median BMFS was 14 months (range 0 to 102) and median OS 6 months (range 0 to 14) (Fig. 2).
GEP NEN patients
Among the 3 GEP NEN patients, one patient presented with a neuroendocrine tumor of the pancreas, one patient with a neuroendocrine carcinoma of the pancreas and one patient with a neuroendocrine carcinoma of the small intestine. Median age of GEP NEN patients at diagnosis of BM was 70 years (range 45 to 73) and median KPS 70% (range 70 to 80). Patients had a median number of 3 extracranial metastatic sites (range 0 to 3) at diagnosis of BM and were treated with a median number of 1 line of systemic therapy (range 0 to 2) before. Before diagnosis of BM, liver metastases were present in 2/3 patients (66.7%), lung metastases in 1/3 patients (33.3%) and peritoneal metastases in 0/3 patients (0.0%). At diagnosis of BM, extracranial disease was progressive in 2/3 patients (66.7%) and in remission in 1/13 patients (33.3%). One/3 patients (33.3%) was symptomatic and 2/3 patients (66.7%) asymptomatic with regards to BM diagnosis. Median number of BM lesions was 3 (range 1 to 4). None/3 patients (0.0%) presented with LC concomitant to solid BM diagnosis. GEP NEN patient characteristics are listed within Table 1. Median BMFS was 7 months (range 0 to 12) and median OS 4 months (range 1 to 12) (Fig. 2).
BM treatment in patients with BM from rare GI tumors
In the overall patient’s cohort, 11/29 (37.9%) of patients were treated with stereotactic radiosurgery (SRS) as initial therapy for BM, 7 (24.1%) with neurosurgical resection, 6 (20.7%) with whole brain radiotherapy (WBRT) and 5 (17.2%) with best supportive care (BSC). Median OS after BM was 4 months in patients treated with GK, 6 months with neurosurgical resection, 3 months with WBRT and 1 month with BSC (p = 0.23; log-rank test) (Fig. 3).
Identification of prognostic biomarkers
Uni- and multivariable analyses of the overall patient cohort were performed to identify prognosticators of OS. Here, a KPS under 80% (p = 0.08), an age above 60 years (p = 0.10) and LC (p = 0.09) at diagnosis of BM were identified as being significantly associated with OS according to univariable analysis. No significant association was observed with regards to number of BM lesions or extracranial metastases (p > 0.1). Within multivariable analysis none of the factors remained independently and significantly associated with OS. Results of uni- and multivariable analyses are listed within Table 2.
Discussion
Within the present study we aimed to characterize patients with BM from hepatopancreatobiliary tumor entities. Among over 6000 BM patients registered in the Vienna Brain Metastasis Registry representing one of the largest datasets on this distinct patient population worldwide, only 29 patients had a rare GI tumor as primary disease. As this represents such an infrequent cohort of patients, our data may provide insight into the clinical course of disease and support treatment decisions in daily clinical practice.
Only recently, the GI-GPA postulated the KPS, age, extracranial disease and number of BM lesions as major prognostic factors after diagnosis of BM in patients with GI primaries [7]. Prognostic biomarkers for survival after diagnosis of BM identified in our study were the KPS, age and the presence of LC, whereas presence or absence of extracranial disease as well as number of BM lesions were not associated with survival and thus seem less relevant in the present cohort. A controlled extracranial disease, however, was shown to act as highly important prognosticator among several tumor entities even after BM diagnosis [9]. Patients with a progressive extracranial disease in our study yielded also an—albeit not significantly—worse survival compared to patients in remission or stable disease within the multivariable analysis (HR 2.12). Therefore, the control of extracranial metastases may be prognostically more relevant after diagnosis of BM than its absence or presence. Another explanation why the extracranial disease may be less relevant in the present patient cohort once BM are diagnosed may be the limited prognosis thereafter.
Interestingly, we observed a rising incidence of BM over the last decades. This is well in line with larger clinical trials including different tumor entities pointing into the same direction [10]. Several factors may contribute to the rising number of BM. There certainly has been a significant improvement of diagnostic imaging techniques. Moreover, awareness of treating physicians to perform cranial imaging in case of BM related symptoms even in tumor entities rarely developing BM may have increased as well. As larger clinical trials observed that especially the number of asymptomatic BM patients is rising, screening implementation may also be important in tumor entities with a high BM probability. Most importantly, prognosis of BM patients improved remarkably over the last decades most likely due to an improvement in local therapies as well as a broader spectrum of systemic therapies available [11].
Compared to other tumor entities, however, the OS after BM of 4 months observed in our study was considerably lower. Patients with BM exhibit the most favorable prognosis with breast, lung and renal cancer primaries with a median of 16, 15 and 12 months, respectively [12]. But also in the cohort of patients included for the GI-GPA assessment, the observed median OS was 8 months [7]. Since included patients consisted primarily of gastroesophageal and colorectal cancer patients, outcome with CCA, HCC, PDAC and GEP NEN may therefore even be worse. One reason for the favorable prognosis of BM patients with other cancer entities most likely lies in an efficient systemic disease control achieved by applied systemic therapies. Furthermore, there is increasing evidence about remarkable intracranial responses achieved by several targeted therapies in certain tumor entities [13,14,15,16]. For patients with CCA, PDAC and GEP NEN, however, targeted therapy approaches so far have not entered clinical routine and intracranial efficacy of chemotherapeutic agents remains limited. Patients with HCC included into the present study were treated before 2017 and thus immunotherapy and the vascular endothelial growth factor receptor (VEGFR) targeted antibody bevacizumab, potentially having some intracranial activity, not yet used. Another reason for the limited prognosis of patients included into the present study may be the generally more aggressive nature of their tumor entities and therefore intracranial tumor cells may bare a more aggressive tumor biology as well.
Patients treated with neurosurgical resection in our study had the best prognosis after BM followed by STS, WBRT and BSC. This is well in line with actual treatment guidelines in this field, that targeted local therapies like resection and STS should be the preferred treatment approach in patients with oligometastatic disease whenever technically feasible [1]. Most operated patients included into this study were diagnosed and treated between the year 2000 and 2010, and postoperative radiation was not standard of care to that time. Therefore, intracranial tumor control may be even favorable nowadays with STS after resection, even though survival times may not be longer compared to observation alone according to a randomized clinical trial [17]. WBRT had been the first-line treatment of choice in patients with multiple BM historically. However, as observed within this study and also within previous studies including other cancer primaries, its efficacy seems comparable to BSC [18, 19]. Therefore, and due to its unfavorable toxicity profile, systemic therapies became the preferred treatment option whenever available in this indication in patients with multiple, asymptomatic BM lesions. In patients with GI cancer entities, however, WBRT may still be considered especially in patients with multiple BM.
Our study clearly faces some limitations manly due to its retrospective design. Moreover, sample sizes of patients within the included tumor subgroups were low and therefore the detected results have to be interpreted with caution. Also, the inclusion period of patients comprised 26 years and therefore respective standards of diagnostic and treatment modalities may be heterogenous. Nevertheless, patients had the benefit of being treated in a GI specialized tertiary care center from their initial diagnosis onwards during their complete course of disease and beyond their BM diagnosis. This gains valuable insight in this rare event to put the prognosis of patients into context. Moreover, this study represents the first characterization of patients with hepatopancreatobiliary cancer entities after diagnosis of BM.
In conclusion, patients with CCA, HCC, PDAC and GEP NEN still face a rather limited OS prognosis of 4 months after diagnosis of BM. Established prognostic factors were shown to apply also for these distinct patient populations. Performance status, age and concomitant LC thereby were the most important clinical factors. Overall, patients with targeted local therapies for BM exhibited the best outcome.
Abbreviations
- BM :
-
Brain metastases
- BMFS:
-
Brain metastases-free survival
- BSC :
-
Best supportive care
- CCA:
-
Cholangiocarcinoma
- GEP NEN:
-
Gastroenteropancreatic neuroendocrine neoplasms
- GI:
-
Gastrointestinal
- GI-GPA:
-
Graded prognostic assessment for gastrointestinal cancers
- GPA:
-
Graded Prognostic Assessment
- HCC:
-
Hepatocellular carcinoma
- IRB:
-
Institutional review board
- KPS:
-
Karnofsky Performance Status
- LC:
-
Leptomeningeal carcinomatosis
- OS:
-
Overall survival
- PDAC:
-
Pancreatic ductal adenocarcinoma
- SPSS:
-
Statistical package for the social sciences
- SRS:
-
Stereotactic radiosurgery
- VEGFR:
-
Vascular endothelial growth factor receptor
- WBRT:
-
Whole brain radiotherapy
References
Le Rhun E, Guckenberger M, Smits M et al (2021) EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Ann Oncol 32:1332–1347
Vogelbaum MA, Brown PD, Messersmith H et al (2022) Treatment for brain metastases: ASCO-SNO-ASTRO Guideline. J Clin Oncol Off J Am Soc Clin Oncol 40:492–516
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep 14:48–54
Cagney DN, Martin AM, Catalano PJ et al (2017) Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: a population-based study. Neuro Oncol 19:1511–1521
Sperduto PW, Berkey B, Gaspar LE et al (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70:510–514
Bartelt S, Momm F, Weissenberger C et al (2004) Patients with brain metastases from gastrointestinal tract cancer treated with whole brain radiation therapy: prognostic factors and survival. World J Gastroenterol 10:3345–3348
Sperduto PW, Fang P, Li J et al (2019) Estimating survival in patients with gastrointestinal cancers and brain metastases: an update of the graded prognostic assessment for gastrointestinal cancers (GI-GPA). Clin Transl Radiat Oncol 18:39–45
Bender R, Lange S (2001) Adjusting for multiple testing–when and how? J Clin Epidemiol 54:343–349
Nieder C, Mehta MP, Guckenberger M et al (2021) Assessment of extracranial metastatic disease in patients with brain metastases: how much effort is needed in the context of evolving survival prediction models? Radiother Oncol J Eur Soc Ther Radiol Oncol 159:17–20
Aizer AA, Lamba N, Ahluwalia MS et al (2022) Brain metastases: a Society for Neuro-Oncology (SNO) consensus review on current management and future directions. Neuro Oncol 24:1613–1646
Steindl A, Brunner TJ, Heimbach K et al (2022) Changing characteristics, treatment approaches and survival of patients with brain metastasis: data from six thousand and thirty-one individuals over an observation period of 30 years. Eur J Cancer 162:170–181
Sperduto PW, Mesko S, Li J et al (2020) Survival in patients with brain metastases: summary report on the updated diagnosis-specific graded prognostic assessment and definition of the eligibility quotient. J Clin Oncol Off J Am Soc Clin Oncol 38:3773–3784
Reungwetwattana T, Nakagawa K, Cho BC et al (2018) CNS response to osimertinib versus standard epidermal growth factor receptor tyrosine kinase inhibitors in patients with untreated EGFR-mutated advanced non-small-cell lung cancer. J Clin Oncol Off J Am Soc Clin Oncol 36:3290–3297
Lin NU, Borges V, Anders C et al (2020) Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol Off J Am Soc Clin Oncol 38:2610–2619
Bartsch R, Berghoff AS, Furtner J et al (2022) Trastuzumab deruxtecan in HER2-positive breast cancer with brain metastases: a single-arm, phase 2 trial. Nat Med 28:1840–1847
Davies MA, Saiag P, Robert C et al (2017) Dabrafenib plus trametinib in patients with BRAF(V600)-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol 18:863–873
Mahajan A, Ahmed S, McAleer MF et al (2017) Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol 18:1040–1048
Nieder C, Norum J, Dalhaug A et al (2013) Radiotherapy versus best supportive care in patients with brain metastases and adverse prognostic factors. Clin Exp Metastasis 30:723–729
Mulvenna P, Nankivell M, Barton R et al (2016) Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority. Lancet (London, England) 388:2004–2014
Funding
Open access funding provided by Medical University of Vienna. The financial support by the Austrian Federal Ministry for Digital and Economic Affairs, the National Foundation for Research, Technology and Development and the Christian Doppler Research Association is gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
1.Conceptualization: ESB, ASB 2.Data curation: ESB, AF, PS, PF 3.Formal analysis: ESB 4.Funding acquisition: MP, ASB 5.Investigation: ESB, ASB 6.Methodology: ESB, ASB 7.Project administration: ASB 8.Resources: ESB, ASB 9.Software: ESB 10.Supervision: ASB 11.Validation: AF, PS, PF, BK, GW, BKiesew, FE, GWP, MP, ASB 12.Visualization: ESB, ASB 13.Writing: original draft: ESB, ASB 14.Writing: review & editing: ESB, AF, PS, PF, BK, GW, BKiesew, FE, GWP, MP, ASB
Corresponding author
Ethics declarations
Conflict of interest
ESB has honoraria for lectures, consultation or advisory board participation from Servier. BKiesew. received honoraria for lectures or advisory board participation from the following for-profit companies: from AAA, Boehringer Ingelheim, Eli Lilly, Ipsen, Janssen-Cilag, MSD, Novartis, Roche, Eli Lilly (all outside of the submitted work). FE received speaker’s fees from Dr. Sennewald Medizintechnik GmbH. GWP declares advisory roles for Merck, Amgen, Roche, Servier, Bayer, Pierre Fabre, MSD, BMS, AstraZeneca and Daiichi Sankyo. MP has received honoraria for lectures, consultation or advisory board participation from the following for-profit companies: Bayer, Bristol-Myers Squibb, Novartis, Gerson Lehrman Group (GLG), CMC Contrast, GlaxoSmithKline, Mundipharma, Roche, BMJ Journals, MedMedia, Astra Zeneca, AbbVie, Lilly, Medahead, Daiichi Sankyo, Sanofi, Merck Sharp & Dome, Tocagen, Adastra, Gan & Lee Pharmaceuticals. Anna Sophie Berghoff has research support from Daiichi Sankyo, Roche and honoraria for lectures, consultation or advisory board participation from Roche Bristol-Meyers Squibb, Merck, Daiichi Sankyo, AstraZeneca, CeCaVa as well as travel support from Roche, Amgen and AbbVie. All other authors declare no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bergen, E.S., Friedrich, A., Scherleitner, P. et al. Brain metastases from hepatopancreatobiliary malignancies. Clin Exp Metastasis 40, 177–185 (2023). https://doi.org/10.1007/s10585-023-10201-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-023-10201-1