Abstract
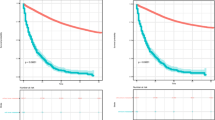
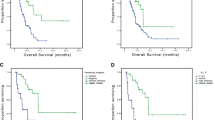
Prognostic factors of synchronous bone metastatic colorectal cancer (CRC) are still undetermined. We aimed to investigate survival outcome and prognostic factors of patients with synchronous bone metastatic CRC. Information of patients with synchronous bone metastatic CRC were obtained from the Surveillance, Epidemiology, and End Results (SEER) and West China Hospital (WCH) databases. Cases from SEER database composed construction cohort, while cases from WCH database were used as validation cohort. A novel nomogram was constructed to predict individual survival probability based on Cox regression model. The performance of the nomogram was internally and externally validated using calibration curves and concordance index (C-index). Three hundred and eighty-one patients from SEER database were eligible. The median disease specific OS was 9.0 months (95% confidence interval [CI]: 7.3–10.7 months). Multivariate Cox analysis identified seven independent prognostic factors including histological type, differentiation grade, T stage of primary tumor, CEA level, systemic chemotherapy, combined with liver metastasis and combined with lung metastasis. A novel nomogram was established based on these variables. In the internal validation, the C-index (0.72, 95% CI 0.69–0.75) and calibration curve indicated well performance of this nomogram at predicting survival outcome in bone metastatic CRC. In the external validation, the C-index was 0.57 (95% CI 0.46–0.68). The prognosis of synchronous bone metastatic CRC is very poor. Histological type, differentiation grade, T stage of primary tumor, CEA level, systemic chemotherapy, combined with liver metastasis and combined with lung metastasis are independent prognostic factors. Further study is warranted to confirm the practicality of the prognostic nomogram.




Similar content being viewed by others
Abbreviations
- CEA:
-
Carcinoembryonic antigen
- CI:
-
Confidence interval
- C-index:
-
Concordance index
- CRC:
-
Colorectal cancer
- HR:
-
Hazard ratio
- OS:
-
Overall survival
- SEER:
-
The Surveillance, Epidemiology, and End Results
- ULN:
-
Upper limit of normal
- US:
-
United States
- WCH:
-
West China Hospital
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Schlüter K, Gassmann P, Enns A et al (2006) Organ-specific metastatic tumor cell adhesion and extravasation of colon carcinoma cells with different metastatic potential. Am J Pathol 169(3):1064–1073
Disibio G, French SW (2008) Metastatic patterns of cancers: results from a large autopsy study. Arch Pathol Lab Med 132(6):931–939
Kanthan R, Loewy J, Kanthan SC (1999) Skeletal metastases in colorectal carcinomas: a Saskatchewan profile. Dis Colon Rectum 42(12):1592–1597
Sundermeyer ML, Meropol NJ, Rogatko A, Wang H, Cohen SJ (2005) Changing patterns of bone and brain metastases in patients with colorectal cancer. Clin Colorectal Cancer 5(2):108–113
Khattak MA, Martin HL, Beeke C et al (2012) Survival differences in patients with metastatic colorectal cancer and with single site metastatic disease at initial presentation: results from South Australian clinical registry for advanced colorectal cancer. Clin Colorectal Cancer 11(4):247–254
Coleman RE (1997) Skeletal complications of malignancy. Cancer 80:1588–1594
Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence—SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2018 Sub (1975–2016 varying)—Linked To County Attributes—Total U.S., 1969–2017 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2019, based on the November 2018 submission. www.seer.cancer.gov
Santini D, Tampellini M, Vincenzi B et al (2012) Natural history of bone metastasis in colorectal cancer: final results of a large Italian bone metastases study. Ann Oncol 23(8):2072–2077
Bostel T, Förster R, Schlampp I et al (2017) Spinal bone metastases in colorectal cancer: a retrospective analysis of stability, prognostic factors and survival after palliative radiotherapy. Radiat Oncol 12(1):115
Zhenghong, Zhu Z, Guoweijian Z et al (2017) Retrospective study of predictors of bone metastasis in colorectal cancer patients. J Bone Oncol 9:25–28
Kawamura H, Yamaguchi T, Yano Y et al (2018) Characteristics and prognostic factors of bone metastasis in patients with colorectal cancer. Dis Colon Rectum 61(6):673–678
Lei S, Ge Y, Tian S et al (2020) Colorectal cancer metastases to brain or bone and the relationship to primary tumor location: a population-based study. J Gastrointest Surg 24:1833–1842
Liu F, Zhao J, Xie J et al (2016) Prognostic risk factors in patients with bone metastasis from colorectal cancer. Tumour Biol. https://doi.org/10.1007/s13277-016-5465-4
Han L, Dai W, Mo S et al (2020) Nomogram to predict the risk and survival of synchronous bone metastasis in colorectal cancer: a population-based real-world analysis. Int J Color Dis 35:1575–1585
Ge H, Yan Y, Xie M, Guo L, Tang D (2019) Construction of a nomogram to predict overall survival for patients with M1 stage of colorectal cancer: a retrospective cohort study. Int J Surg 72:96–101
Lee WS, Yun SH, Chun HK et al (2007) Pulmonary resection for metastases from colorectal cancer: prognostic factors and survival. Int J Color Dis 22(6):699–704
Li A, Käsmann L, Rades D, Fu C (2017) A scoring system to predict the development of bone metastasis after radical resection of colorectal cancer. Anticancer Res 37(9):5169–5172
Guan X, Ma CX, Quan JC et al (2019) A clinical model to predict the risk of synchronous bone metastasis in newly diagnosed colorectal cancer: a population based study. BMC Cancer 19(1):704
National Comprehensive Cancer Network (2020) NCCN clinical practice guidelines in oncology: colon cancer. Version 3. www.nccn.org. Accessed 6 May 2020
National Comprehensive Cancer Network (2020) NCCN clinical practice guidelines in oncology: rectal cancer. Version 3. www.nccn.org. Accessed 6 May 2020
Falcone A, Ricci S, Brunetti I et al (2007) Phase III trial of infusional fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) compared with infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) as first-line treatment for metastatic colorectal cancer: the Gruppo Oncologico Nord Ovest. J Clin Oncol 25:1670–1676
Loupakis F, Cremolini C, Masi G et al (2014) Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med 371:1609–1618
Cremolini C, Antoniotti C, Rossini D et al (2020) Upfront FOLFOXIRI plus bevacizumab and reintroduction after progression versus mFOLFOX6 plus bevacizumab followed by FOLFIRI plus bevacizumab in the treatment of patients with metastatic colorectal cancer (TRIBE2): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol 21(4):497–507
Acknowledgements
The authors acknowledge the National Cancer Institute for providing the SEER dataset.
Funding
This work was supported by the Youth Program of National Natural Science Foundation of China (No. 81402358).
Author information
Authors and Affiliations
Contributions
XL and HG conceived of and designed this study. XL, WH performed the analyses. XL, WH and HS prepared tables and figures. XL wrote the main manuscript. All authors approved to the submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the West China Hospital, Sichuan University Ethic Committee for Clinical Investigation.
Informed consent
Written informed consent for publication was obtained from all patients at the time of admission as a routine practice at West China Hospital, Sichuan University.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, X., Hu, W., Sun, H. et al. Survival outcome and prognostic factors for colorectal cancer with synchronous bone metastasis: a population-based study. Clin Exp Metastasis 38, 89–95 (2021). https://doi.org/10.1007/s10585-020-10069-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-020-10069-5