Abstract
Background
Clinical guidelines recommend peri-cardioversion anticoagulation in patients with atrial fibrillation (AF). We performed a systematic review and meta-analysis to compare the safety and efficacy of direct oral anticoagulants (DOACs) versus vitamin K antagonists (VKAs) in patients with AF undergoing cardioversion.
Methods
We searched CENTRAL, MEDLINE, and EMBASE for randomized controlled trials (RCTs) and observational studies comparing DOACs to VKAs in patients undergoing cardioversion for AF. We performed title, abstract, and full-text screening, data extraction, and risk of bias evaluation independently and in duplicate. We pooled data using a random effects model and evaluated the overall quality of evidence using Grading of Recommendations Assessment, Development and Evaluation.
Results
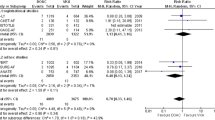
We identified three eligible RCTs (n = 5203) and 21 observational studies (n = 11,855). The three RCTs and four observational studies were at low risk of bias. In RCTs (mean follow-up, 30 days), thromboembolic events occurred in 0.18% of patients receiving DOACs, as compared with 0.55% receiving VKAs (relative risk [RR] 0.40, 95% CI [0.13, 1.24], moderate quality). Major bleeding occurred in 0.42% of patients receiving DOACs as compared with 0.64% receiving VKAs (RR 0.62, 95% CI [0.28, 1.35], moderate quality), and death occurred in 0.28% of patients receiving DOACs as compared with 0.38% receiving VKAs (RR 0.70, 95% CI [0.23, 2.10], low quality). Confidence in the estimates of effect for observational studies was very low.
Conclusion
DOACs peri-cardioversion in patients with AF appears safe from both a bleeding and thromboembolic risk perspective. Available evidence supports the use of DOACs as standard of care peri-cardioversion in patients with AF.





Similar content being viewed by others
References
Humphries KH, Jackevicius C, Gong Y, et al. Population rates of hospitalization for atrial fibrillation/flutter in Canada. Can J Cardiol. 2004;20:869–76.
de Lusignan S, van Vlymen J, Hague N, Thana L, Dzregah B, Chan T. Preventing stroke in people with atrial fibrillation: a cross-sectional study. J Public Health (Oxf). 2005;27:85–92.
Carroll K, Majeed A. Comorbidity associated with atrial fibrillation: a general practice-based study. Br J Gen Pract. 2001;51:884–6 889-91.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:e1–76.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–962.
Macle L, Cairns J, Leblanc K, Tsang T, Skanes A, Cox JL, et al. 2016 focused update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2016;32:1170–85.
Klein HH, Trappe HJ. Cardioversion in non-valvular atrial fibrillation. Dtsch Arztebl Int. 2015;112:856–62.
Laszlo R, Laszlo S, Graze H, Schreieck J. Electrical cardioversion for atrial fibrillation. Dtsch Med Wochenschr. 2010;135:750–4.
Camm AJ, Savelieva I, Lip GY. Guideline Development Group for the NICE Clinical Guidelines For the management of atrial fibrillation. Rate control in the medical management of atrial fibrillation. Heart. 2007;93:35–8.
Cutro R Jr, Burkart TA, Curtis AB. Rapid achievement of therapeutic anticoagulation positively affects outcome in patients undergoing cardioversion for persistent atrial fibrillation. Clin Cardiol. 2006;29:78–82.
Reiffel JA. Cardioversion for atrial fibrillation: treatment options and advances. Pacing Clin Electrophysiol. 2009;32:1073–84.
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:e199–267.
Gibson CM, Basto AN, Howard ML. Direct oral anticoagulants in cardioversion: a review of current evidence. Ann Pharmacother. 2018;52:277–84.
You JJ, Singer DE, Howard PA, Lane DA, Eckman MH, Fang MC, et al. Antithrombotic therapy for atrial fibrillation: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e531S–75S.
Goette A, Hammwohner M, Bukowska A, et al. The impact of rapid atrial pacing on ADMA and endothelial NOS. Int J Cardiol. 2012;154:141–6.
Lendeckel U, Arndt M, Wrenger S, Nepple K, Huth C, Ansorge S, et al. Expression and activity of ectopeptidases in fibrillating human atria. J Mol Cell Cardiol. 2001;33:1273–81.
Bukowska A, Zacharias I, Weinert S, Skopp K, Hartmann C, Huth C, et al. Coagulation factor Xa induces an inflammatory signalling by activation of protease-activated receptors in human atrial tissue. Eur J Pharmacol. 2013;718:114–23.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–62.
Papp J, Zima E, Bover R, Karaliute R, Rossi A, Szymanski C, et al. Changes in oral anticoagulation for elective cardioversion: results from a European cardioversion registry. Eur Heart J Cardiovasc Pharmacother. 2017;3:147–50.
Covidence systematic review software VHI, Melbourne, Australia. Available at www.covidence.org. Accessed 12 Jan 2018.
Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Tool to Assess Risk of Bias in Cohort Studies The Clarity Review Group. http://help.magicapp.org/knowledgebase/articles/327941-tool-to-assess-risk-of-bias-in-cohort-studies. Accessed 1 June 2018.
Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre TCC; 2014.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Antonopoulos P. Anticoagulation with rivaroxaban in cardioversion - the ARC Study (ARC). Stroger Hospital: John H; 2015.
Cappato R, Ezekowitz MD, Klein AL, Camm AJ, Ma CS, le Heuzey JY, et al. Rivaroxaban vs. vitamin K antagonists for cardioversion in atrial fibrillation. Eur Heart J. 2014;35:3346–55.
Ezekowitz MD, Pollack CV Jr, Halperin JL, England RD, VanPelt Nguyen S, Spahr J, et al. Apixaban compared to heparin/vitamin K antagonist in patients with atrial fibrillation scheduled for cardioversion: the EMANATE trial. Eur Heart J. 2018;39:2959–71.
Goette A, Merino JL, Ezekowitz MD, Zamoryakhin D, Melino M, Jin J, et al. Edoxaban versus enoxaparin-warfarin in patients undergoing cardioversion of atrial fibrillation (ENSURE-AF): a randomised, open-label, phase 3b trial. Lancet. 2016;388:1995–2003.
Nagarakanti R, Ezekowitz MD, Oldgren J, Yang S, Chernick M, Aikens TH, et al. Dabigatran versus warfarin in patients with atrial fibrillation: an analysis of patients undergoing cardioversion. Circulation. 2011;123:131–6.
Barysiene J, Zebrauskaite A, Petrikonyte D, Marinskis G, Aidietiene S, Aidietis A. Findings of transoesophageal echocardiogram in appropriately anticoagulated patients with persistent atrial fibrillation prior to planned cardioversion. BMC Cardiovasc Disord. 2017;17:67.
Basto AN, Fewel NP, Gupta R, Stock EM, Mia TM. A comparison between dabigatran and warfarin on time to elective cardioversion. J Atr Fibrillation. 2016;8:1355.
Carrizo AG, Lamelas P, Pinilla Echeverri N, Morillo CA. Real world usage of oral anticoagulants in patients undergoing electrical cardioversion for atrial tachyarrhythmias. Can J Cardiol. 2015;31:1.
Chirino Navarta DA, Palacios R, Leonardi MS, Trejo G, Baletti L, et al. Presence of thrombus and spontaneous contrast in the left atrium of patients with atrial fibrillation anticoagulated with dabigatran and acenocoumarol. Rev Argent Cardiol. 2015;83.
Femia G, Fetahovic T, Shetty P, Lee A. Novel oral anticoagulants in direct current cardioversion for atrial fibrillation. Heart Lung Circ. 2018;27:798–803.
Flaker G, Lopes RD, Al-Khatib SM, et al. Efficacy and safety of apixaban in patients after cardioversion for atrial fibrillation: insights from the ARISTOTLE trial (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation). J Am Coll Cardiol. 2014;63:1082–7.
Rostock T, Sonnenschein S, et al. Long-term anticoagulation is not associated with reliable absence of left atrial appendage thrombi in atrial fibrillation patients referred for electrical cardioversion. Heart Rhythm. 2016;13:1.
Lejnieks A, Erglis A, et al. Comparison of dabigatran and rivaroxaban versus warfarin in patients with persistent and long-standing atrial fibrillation undergoing electrical cardioversion with high risk of stroke and embolism. Circulation. 2016;134.
Kochhauser S, Khaykin Y, Beardsall J, et al. Comparison of outcomes after cardioversion or atrial fibrillation ablation in patients with differing periprocedural anticoagulation regimens. Can J Cardiol. 2014;30:1541–6.
Pallisgaard JL, Lindhardt TB, Hansen ML, Schjerning AM, Olesen JB, Staerk L, et al. Cardioversion and risk of adverse events with dabigatran versus warfarin-a nationwide cohort study. PLoS One. 2015;10:e0141377.
Persidskikh Y, Mrochek A, Goncharik D, Chasnoits A, Plashchinskaya L, Barsukevich V, et al. Short-term pre cardioversion anticoagulation with dabigatran etexilate in patients with persistent atrial fibrillation. Europace. 2017;19:iii398.
Plitt A, Ezekowitz MD, De Caterina R, et al. Cardioversion of atrial fibrillation in ENGAGE AF-TIMI 48. Clin Cardiol. 2016;39:345–6.
Russo V, Rago A, Papa AA, D’Onofrio A, Golino P, Nigro G. Efficacy and safety of dabigatran in patients with atrial fibrillation scheduled for transoesophageal echocardiogram-guided direct electrical current cardioversion: a prospective propensity score-matched cohort study. J Thromb Thrombolysis. 2018;45:206–12.
Serpytis P, Palsauskaite R, Navickas G, Tamosiunas T, et al. Dabigatran vs. warfarin and the postcardioversion thromboembolic risk. Eur Heart J. 2015;4:1.
Sharif Z, Srinivas B, Tiedt I, Ryan N, Awadalla M, Sullivan V, et al. Evaluating cardioversion outcomes for atrial fibrillation on novel oral anticoagulants versus warfarin: experience at a tertiary referral centre. Ir J Med Sci. 2017;186:615–20.
Zylla MM, Pohlmeier M, Hess A, Mereles D, Kieser M, Bruckner T, et al. Prevalence of intracardiac thrombi under phenprocoumon, direct oral anticoagulants (dabigatran and rivaroxaban), and bridging therapy in patients with atrial fibrillation and flutter. Am J Cardiol. 2015;115:635–40.
Arujuna A, Ooues G, Abbas A, Sivanandarajah P, Sidhu B, et al. Electrical cardioversion of atrial fibrillation with the novel oral anticoagulants: a single centre UK-based registry experience. EP Eur. 2014;16:iii16.
Cohen R, Aroney N, Blenkhorn A, Cross J. The incidence of left atrial appendage thrombus in warfarin versus NOACS prior to transoesophageal echocardiogram guided cardioversion. Heart Lung Circ. 2016;25:S279–80.
Verma A, Beardsall J, Juta R, Hache P, Lenton-Brym T, Tsang B, et al. Comparison of outcomes post-cardioversion of patients with differing peri-procedural anticoagulation regimens. Can J Cardiol. 2014;30:S182.
Emily Keltner CW, Becker A, Davis C, Wilson WW. No difference in 30-day adverse event rate or recurrence of atrial fibrillation between warfarin and direct oral anticoagulants used in elective cardioversion: an outpatient registry analysis. Circulation. 2018;136(suppl_1):1.
Mayer F, Kirchmayer U, Coletta P, Agabiti N, Belleudi V, Cappai G, di Martino M, Schneeweiss S, Davoli M, Patorno E. Safety and effectiveness of direct oral anticoagulants versus vitamin K antagonists: pilot implementation of a near-real-time monitoring program in Italy. J Am Heart Assoc. 2018;7.
Optimal warfarin management for the prevention of thromboembolic events in patients with atrial fibrillation: a systematic review of the clinical evidence. Ottawa (ON), 2011.
Fitzmaurice DA, Blann AD, Lip GY. Bleeding risks of antithrombotic therapy. BMJ. 2002;325:828–31.
Schein JR, White CM, Nelson WW, Kluger J, Mearns ES, Coleman CI. Vitamin K antagonist use: evidence of the difficulty of achieving and maintaining target INR range and subsequent consequences. Thromb J. 2016;14:14.
Alexander JH, Lopes RD, Thomas L, Alings M, Atar D, Aylward P, et al. Apixaban vs. warfarin with concomitant aspirin in patients with atrial fibrillation: insights from the ARISTOTLE trial. Eur Heart J. 2014;35:224–32.
Schulman S, Kakkar AK, Goldhaber SZ, Schellong S, Eriksson H, Mismetti P, et al. Treatment of acute venous thromboembolism with dabigatran or warfarin and pooled analysis. Circulation. 2014;129:764–72.
Investigators E, Bauersachs R, Berkowitz SD, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363:2499–510.
Investigators E-P, Buller HR, Prins MH, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366:1287–97.
Grzymala-Lubanski B, Labaf A, Englund E, Svensson PJ, Sjalander A. Mechanical heart valve prosthesis and warfarin - treatment quality and prognosis. Thromb Res. 2014;133:795–8.
Korenstra J, Wijtvliet EP, Veeger NJ, et al. Effectiveness and safety of dabigatran versus acenocoumarol in ‘real-world’ patients with atrial fibrillation. Europace. 2016;18:1319–27.
Raval AN, Cigarroa JE, Chung MK, et al. Management of patients on non-vitamin K antagonist oral anticoagulants in the acute care and periprocedural setting: a scientific statement from the American Heart Association. Circulation. 2017;135:e604–33.
Habert JS. Minimizing bleeding risk in patients receiving direct oral anticoagulants for stroke prevention. Int J Gen Med. 2016;9:337–47.
Eikelboom J, Merli G. Bleeding with direct oral anticoagulants vs warfarin: clinical experience. Am J Med. 2016;129:S33–40.
Hansen ML, Jepsen RM, Olesen JB, et al. Thromboembolic risk in 16 274 atrial fibrillation patients undergoing direct current cardioversion with and without oral anticoagulant therapy. Europace. 2015;17:18–23.
Benzimra M, Bonnamour B, Duracinsky M, Lalanne C, Aubert JP, Chassany O, et al. Real-life experience of quality of life, treatment satisfaction, and adherence in patients receiving oral anticoagulants for atrial fibrillation. Patient Prefer Adherence. 2018;12:79–87.
Brunetti ND, Tarantino N, De Gennaro L, Correale M, Santoro F, Di Biase M. Direct oral anti-coagulants compared to vitamin-K antagonists in cardioversion of atrial fibrillation: an updated meta-analysis. J Thromb Thrombolysis. 2018;45:550–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Gupta, S., Um, K.J., Pandey, A. et al. Direct Oral Anticoagulants Versus Vitamin K Antagonists in Patients Undergoing Cardioversion for Atrial Fibrillation: a Systematic Review and Meta-analysis. Cardiovasc Drugs Ther 33, 339–352 (2019). https://doi.org/10.1007/s10557-019-06869-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-019-06869-x