Abstract
Cardiac consequences of Covid-19 infection have been mentioned in various studies as a serious risk factor for in-hospital mortality. However, the existence of residual cardiac dysfunction after the acute phase is seldom investigated especially in people without a history of specific medical disease. One hundred health care workers with positive reverse transcription-polymerase chain reaction test underwent comprehensive 2D and 3D echocardiography six to eight weeks after infection. Patients were classified into Mild, Moderate, and Severe groups based on their clinical characteristics of covid-19 infection, and all echocardiographic parameters were compared between the three groups. Left ventricular (LV) stroke volume index was reduced in all groups compared to normal ranges and was more prominent in the severe group (P-value < 0.05). 3D-derived LV global longitudinal strain (GLS) was significantly lower in the severe group in comparison to the mild group (− 19.3 ± 1 Vs. − 22.2 ± 2, P-value < 0.001) and correlated with highly sensitive CRP level at the acute phase. Left atrial (LA) strains, including LA peak strain, LA contraction strain, and LA reservoir strain, were considerably higher and LA volume index was significantly lower in the clinically severe covid patients. Analysis based on the extent of lung involvement showed significantly increased 3D-derived right ventricular volumes in patients who experienced severe pneumonia despite normalized strains. Conclusion: subclinical LV dysfunction as reduced stroke volume index and GLS exists in the early recovery phase of normal individuals with severe course of covid-19. LA function indicated by LA strains paradoxically increases in severe covid-19 infection in this phase.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronavirus disease 2019 (Covid-19) pandemic is a worldwide serious condition that has resulted in over 6 million deaths [1]. Cardiac injury has been identified in several postmortem studies [2, 3] and mentioned as an independent predictor of mortality among hospitalized patients [4, 5]and was more prevalent in patients with coronary artery disease and cardiovascular comorbidities [6]. However few studies have been conducted to evaluate the cardiac impact of Covid-19 infection on non-hospitalized apparently normal individuals afflicted by the mild form of the disease. Moreover, the knowledge of the early recovery phase of covid-19 infection is lacking. A crucial period in which patients recommence their work with possible residual cardiac consequences. This could put them at risk of experiencing fatigue, various cardiac arrhythmias, and sudden cardiac death. One study of recently recovered subjects from Covid-19, comprising both hospitalized and non-hospitalized patients, demonstrated cardiac involvement in 78% and ongoing cardiac inflammation in 60% of these individuals using T1 and T2 Cardiac Magnetic Resonance imaging [7]. The other study used cardiac magnetic resonance on non-hospitalized competitive athletes after the complete recovery phase indicating a 15% prevalence of myocarditis despite normal troponin levels and mild symptoms [8]. This study aimed to identify detailed residual cardiac features of covid-19 infection during the early recovery phase, using comprehensive two-dimensional (2D) and three-dimensional (3D) echocardiographic assessment of all four cardiac chambers, including longitudinal strains and strain rates.
Materials and methods
Study population
We conducted a cross-sectional study between March 22, 2020, and January 20, 2021, during the Covid-19 third wave peak in Iran. The study population was composed of Rajaie cardiovascular medical and research center’s health care workers who get infected with SARS-COV-2. Three hundred nineteen employees in this period were advised to be quarantined due to suspicious symptoms by infectious disease specialists. We enrolled 137 individuals with a definite Covid-19 infection confirmed by a positive reverse transcription-polymerase chain reaction (rt-PCR) test. Thirty-three patients refused to undergo echocardiography. Four patients were excluded from the study due to preexisting cardiovascular disease (three had a history of cardiac surgery, and one had moderate valvular aortic stenosis). One hundred patients underwent comprehensive echocardiographic examination six to eight weeks after recovery and returning to work. They were otherwise healthy with no underlying disease (e.g., structural heart disease, chronic obstructive pulmonary disease, and chronic kidney disease). Patient’s demographic data consisting of age, Cardiovascular Risk Factors, Body surface area, and laboratory findings at the time of infection, including white blood cell count, lymphocyte count, presence of anemia; defined as hemoglobin (Hb) level < 12 gr/dl in women and Hb level < 13 gr/dl in men, and highly sensitive CRP level (hsCRP) were recorded.
Covid-19 severity definition
According to a recently published article in the New England Journal of Medicine [9], all patients were classified into four groups regarding clinical and radiological findings:
-
(1)
Mild illness: mild symptoms (e.g., cough, fever, change in smell/taste) without dyspnea.
-
(2)
Moderate illness: clinical or radiographic evidence of lower respiratory tract disease; oxygen saturation ≥ 94%.
-
(3)
Severe illness: oxygen saturation < 94% or respiratory rate ≥ 30 breaths/min or lung infiltrates > 50%.
-
(4)
Respiratory failure, shock, and multiorgan dysfunction and failure.
Chest computed tomography scan scoring
According to the infectious disease specialists order, 46 patients underwent chest computed tomography (CT) scan. Six normal CTs were excluded because the time interval from symptom onset to scan was less than one week. We included scans within 7–14 days from the disease onset with mild symptoms or shorter intervals if the patient presented with dyspnea or decreased O2 saturation.
All chest CTs were reviewed by a radiologist and assigned as lung total severity score (LTSS). This scoring system is based on a method for quantitative evaluation of lung involvement introduced by Kunwei Li et al. [10] and utilized to evaluate disease severity. The percentage of each five lung lobes was determined and classified as no (0%: zero point), minimal (1–25%: 1 point), mild (26–50%: 2 points), moderate (51–75%: 3 points), and severe (76–100%: 4 points). The sum of lobar points yields the final LTSS, ranging from 0 to 20. The cut-off value of ≥ 7.5 was correlated with severe to critical clinical disease with 100% specificity and 78% sensitivity.10 We categorize LTSS into three categories, 0 (LTSS = 0, as no lung involvement), 1 (LTSS = 1–7 scores, as non-severe lung involvement), and 2 (LTSS ≥ 7.5 scores, as severe lung involvement).
Echocardiographic examinations
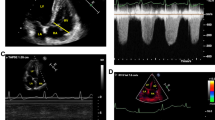
All echocardiograms were obtained in standard parasternal and apical views using Philips Epic 7 C system (Philips Medical Systems, Andover, MA, USA) and Philips X5-1 matrix Probe. 2D and 3D image acquisitions were made by experienced cardiac sonographers. All measurements and 2D and 3D analyses were done offline using commercially available post-processing software (TomTec V4.6) by a cardiologist with an echocardiography fellowship. 3D Left Ventricular (LV) evaluation comprises assessments of 3D volumes, Ejection Fraction (EF), stroke volume index (SVI), Global longitudinal strain (GLS), Global Circumferential Strain (GCS), Global Radial strain (GRS), twist, and torsion values using Tomtec dedicated application for 3D LV analysis (Fig. 1).
Diastolic indices consisted of mitral inflow E and A wave velocity and septal (septal e’) and lateral (lateral e’) early diastolic tissue myocardial velocities using a tissue Doppler imaging method. E/e’ ratio was calculated by dividing E velocity by average septal and lateral e’ velocities. Finally, a cardiologist determined the global diastolic dysfunction grading concerning the other related factors such as left atrial volume index (LAVI) and Tricuspid regurgitation velocity, according to guidelines of the American Society of Echocardiography 2016 [11]. Right Ventricular (RV) anatomical assessment including 3D RV volumes, EF, and Fractional Area Change (FAC) was made using a dedicated application for 3D RV analysis (TomTec V 4.6) (Fig. 2). Parameters of RV function consisted of measurement of Tricuspid Annular Plane Systolic Excursion (TAPSE) by M-Mode, Peak basal systolic RV tissue velocity by tissue doppler imaging (RVsm), RV Myocardial Performance Index (RV MPI) by tissue doppler imaging using this formula: isovolumic contraction time + isovolumic relaxation time/ejection time. RV free wall longitudinal strains (RVFW strain) and Peak strain rate were measured using the RV-focus view by 2D Tomtec strain software.
Left and right atrial (LA and RA) evaluation comprise end-systolic volume indexes (LAVI and RAVI), reservoir, conduit, and contraction phases strain as well as peak strain rate using speckle tracking technique and TomTec V4.6 dedicated application for atrial strain. Standard non-foreshortened apical four-chamber views according to the expert consensus recommendations for standardization of LA and RA strain were utilized [12]. (Fig. 3)
Measurement of right atrial and left atrial strain according to the task force recommendation of EACVI consensus12; Nadir of Atrial average strain curve (white curve) at end-diastole was defined as zero reference point. Atrial reservoir phase strain was calculated as the difference between the onset of diastolic filling and the end-diastolic value. Atrial conduit phase strain was measured as the difference between the onset of filling and the onset of atrial contraction. Atrial contraction phase strain was calculated as the difference between the onset of filling and the onset of atrial contraction
Systolic Pulmonary Arterial Pressure (sPAP) was calculated from tricuspid regurgitation gradient plus RA pressure (defined by IVC size and collapsibility). Pulmonary valve acceleration time (PVAT); the time from the beginning of PW Doppler signal of pulmonary flow at the level of pulmonary valve to the peak, was also assessed and corrected by HR by this formula: Corrected PVAT = PVAT*75/HR.
Valvular regurgitation and severity were evaluated, and more than mild degrees of regurgitation or any degree of stenosis made the patient excluded from the study.
The protocol and objectives of the study have been reviewed and approved by the institutional review board of Rajaie Cardiovascular Medical and Research Center, Tehran, Iran. All patients signed informed written consent and gave permission for the use of their data for clinical research purposes.
Statistical analysis
Continuous variables were reported as mean ± SD or median (interquartile range) based on the normality of distribution. Categorical variables were reported as numbers (percentage). The chi-squared test or Fisher’s exact test was used as appropriate. Based on the normality of data distribution, continuous variables were compared between groups using the t-test or Mann-Whitney U test as appropriate. Two-sided p values were reported. All statistical analyses were performed using the STATA software (StataCorp, TX, USA).
Results
A total of 100 patients diagnosed with Covid-19 confirmed by the rt-PCR test were included in this study. Based on the survey by Gandhi R et al.[9] sixty, twenty-four, and sixteen patients were categorized into mild, moderate, and severe Covid-19, respectively. None had experienced respiratory failure. The mean time passed from the Covid-19 was 52.34 ± 9 days, and it was comparable between the Covid-19 severity groups. The length of the homestay was 17.8 ± 6.4 days among patients; however, it was significantly different among groups (P-value = 0.008), and considerably higher in patients with severe and moderate Covid-19 compared to those with mild Covid-19 (P-value < 0.05). The hsCRP level was significantly higher in the severe group compared to the mild and moderate Covid-19 group. Other baseline characteristics are summarized in Table 1.
Of echocardiographic parameters, 3D LV volume indices were comparable between three groups of clinical severity. However, the 3D derived SVI was lower than the normal reference range for the 3D SVI by the EACVI-NORRE study [13], and it was more reduced in Severe Covid-19 disease than in the mild Covid-19 group (P-value < 0.05). Mean 3-D derived LV EF was above 55% in all groups with a trend to decrease in EF from 61% in the Mild group to 58% in the Severe group (P-value = 0.07). 3D global LV GLS was significantly lower in the Severe group compared to the Mild group (− 19.3 ± 1 Vs. − 22.2 ± 2, P-value < 0.001)(Fig. 4) and correlated with hsCRP level (ρ = 0.29, P-value = 0.04) (Fig. 5). GCS was similar in three groups. For GRS, there was a trend in reducing values in the Severe group contrasted to the mild group (37 ± 3 VS 40 ± 4.5, P-value = 0.08). Twist, Torsion, and Strain rates were equivalent in all groups.
Diastolic function and all diastolic indices, including E/e’ ratio, were normal in all patients. In addition, LV tissue doppler indices were comparable. However, there was a trend for lateral e’ velocity to be lower in patients with severe Covid-19 compared to those with mild Covid-19 (15.3 ± 3.5 vs. 13.1 ± 2.7 cm/sec, P-value = 0.07). All groups had similar RV parameters, including 3D Volumes and EF, 2D strains and FAC, TAPSE, and Tei index. Among RA indices, the RA volume index was significantly higher in the severe Covid-19 group than in the moderate ones (18.9 ± 5 versus 15.2 ± 4 ml/m2, P-value = 0.05). Other RA parameters were unremarkable. Left atrial stains, including LA peak strain, LA contraction strain, and LA reservoir strain, were significantly higher in the clinically Severe group (Fig. 6). Moreover, the LA volume index was lower in this group in comparison to the Mild group (14.9 ± 5 Vs. 19.9 ± 5 cc/m2, P-value = 0.01). The mean of Systolic PAP was in the normal range in all groups, although it was slightly higher in the Severe group (P Value: 0.012). Corrected PV acceleration time (corrected PVAT) was significantly lower in the Severe category compared to the mild category (109 ± 37 Vs. 132 ± 24 msec, P-value = 0.006); the difference was also noted between the moderate and mild categories. Other echocardiographic findings among groups by Covid-19 severity have been summarized in Table 1.
Of one hundred covid-19 patients, thirty-nine patients underwent CT scan imaging of the lung. According to the defined criteria, fourteen, twenty-one, and four patients had no lung involvement, non-severe lung involvement, and severe lung involvement, respectively. With increasing the lung involvement identified by CT imaging, the amount of body surface area and male predominance enhance (both P-values < 0.05). Moreover, the hsCRP level was dramatically enhanced by increasing the involvement of the lungs in CT imaging (P-value = 0.022). Among groups by lung involvement, all measured LV parameters were comparable. Of values for diastolic dysfunction, lateral e’ velocity was significantly different among groups (P-value = 0.041), and it was lower in patients with severe lung involvement compared to the other groups. Of measured RV features, 3D RV end-systolic and end-diastolic volume indices were significantly higher in those with severe lung disease compared to other groups (P-value = 0.009 and P-value = 0.001, respectively). The remaining parameters of RV were similar in all groups. All measured LA, and RA echocardiographic features were comparable among groups, but the RA volume index was significantly higher in patients with severe lung involvement (24.2 ± 7 vs. 15,7 ± 4.2, P-value = 0.006). Among RA strains, the RA reservoir strain was lower in patients with severe lung involvement than in the non-Severe group (48 ± 10 vs. 36 ± 9, P-value = 0.05). Baseline characteristics and echocardiographic measures analyzed based on CT imaging are summarized in Table 2.
Discussion
Our investigation revealed that in the early recovery phase, 3-D-derived LV GLS was lower in individuals who had suffered from a severe form of covid-19 compared to others who experienced a milder clinical course. GLS values were correlated with the hsCRP level at the acute phase. The SVI was decreased in all groups compared to normal reference ranges of 3D-derived SVI in the EACVI NORRE study (32–43 cc/m2) [13]. Although we don’t have their pre-covid data, they were supposed to have normal SVI since all were healthy, low-risk individuals. Mean SVI was significantly correlated with disease severity and was lower in those with severe clinical courses. EF remained in the normal range in all patients. However, there was a trend in reducing EF from 61% in milder groups to 55% in the severe group (P-value = 0.07). A decrease in longitudinal strain has been described in various investigations in the acute phase of disease in hospitalized or critically ill patients. It was linked with higher in-hospital mortality risk [14, 15, 16]. In the COVID-WASE study [16], 722 worldwide hospitalized patients with covid-19, underwent echocardiographic examination on 1–9 days of admission; 83% of patients had normal EF, 11% had mild LV dysfunction, and 5% and 3% had moderate and severe LV dysfunction respectively. Mean LV GLS was − 18.7%, and twenty-two% had severely reduced GLS. LV GLS was reported as one of the independent predictors of in-hospital death. In the study of Bhatia et al. on 96 hospitalized patients with covid-19, 2D GlS were abnormal in 91% of patients in the acute phase, and patients with cardiovascular disease had worse median GLS. EF was in the normal range [17]. In addition, the study of Li R et al. on 216 hospitalized patients with covid-19 without underlying cardiovascular disease demonstrated more 2D GLS reduction in critically ill patients than non-critical ones, and it was correlated with hsCRP. EF was mildly reduced in the hospitalization phase in the critical group (− 47.8%), whereas it was in the normal range in the non-critical group (57.8%) [18]. We could find only one study that included the early recovery phase of low-risk outpatients with covid-19 that showed substantially lower 2D GLS after 11–89 days of recovery compared to the control group who did not experience covid infection (− 19.17 vs. − 20.07, p = 0.03) [19]. Longer follow-up data were reported in the follow-up study of Wase-Covid after a mean of 120 days of hospitalization. It concluded no significant changes in LV and RV function at follow-up except for patients with impaired LV and RV function and strains who improved markedly in relation to the baseline [20].
Results of our research established subclinical LV dysfunction with apparent normal EF, more pronounced reduced SVI, and lower 3D LV GLS in the early recovery phase of patients with the severe clinical course of covid-19. Reduced SVI may be one of the explanations for feeling fatigued on the first days returning to work necessitating more caution to be exercised in this group for restarting the work.
All patients had a normal diastolic function, and LV diastolic measures were within normal reference limits. There was a trend for reducing lateral e’ in severe diseases than mild conditions. The prevalence of diastolic dysfunction in one hundred patients hospitalized for covid-19 has been reported 16% in the acute phase by Yishay Szekely and colleagues[21]. However, comorbidities were present in 72% of the participants in this study. Our study revealed no evidence of diastolic dysfunction or increased LV filling pressures in otherwise healthy people in the early convalescence period.
RV 3D volumes, EF, other functional parameters, and RVFW strain were in the normal range and comparable in three groups. Similar to LV GLS, abnormal RV strain was reported in several studies in hospitalized patients and mentioned as a predictor of in-hospital mortality [14, 16, 22]. In contrast to LV, RV could recover more rapidly after myocardial insult. Popescu et al. found that even at discharge, functional recovery of the RV after MI was considerable in the Gissi-3 Echo substudy [23]. In Baruch et al. study, echocardiography was performed in 80 patients with covid-19 during hospitalization and three months later RV functional parameters and RV strain improved dramatically in contrast to unrecovered LV strain [24]. Our research highlighted that even in the early stages of recovery from covid-19 infection, the RV is capable of rapid functional recovery with no residual impairment.
Despite being within normal reference ranges, the RA volume index was significantly higher in patients with a severe form of the disease than in moderate conditions. It could reflect probable RA dilation in severe form in the acute phase that recovered in this phase. Surprisingly LA peak, contraction, and reservoir strains were higher, and consistently, the LAVI was lower in the Severe group. In the study of Baycan et al., LA anteroposterior diameter was significantly higher in the Severe Covid-19 group in the acute phase [15]. In contrast, Goerlich et al. reported lower LAVI in hospitalized patients with covid-19 compared to the non-covid control group, lower LA strains in this study were more common in AF patients [25]. In a similar study, Beyls et al. discovered that in ICU patients with covid-19 and impaired LA strains, the occurrence of AF increases considerably [26]. Xie. et al. analyzed LA peak strain in two groups of hospitalized patients with and without cardiac injury based on elevated troponin levels, and there were no significant differences [27]. Nevertheless, Data of LA strains and volume in the acute phase is insufficient in the literature. The plausible explanation for this finding in our survey could be either the paradoxical compensatory activity of LA in the setting of subclinical LV dysfunction or overcorrection of previously impaired LA function in the acute phase.
The mean of Systolic PAP was in the normal range in all groups, but Corrected PVAT was significantly lower in the severe group. It suggests PVAT (an indicator of mean PAP) may be more consistently compromised than systolic PAP, indicating higher PA pressure in the acute and early recovery phases in a clinically severe type of the disease.
Furthermore, we analyzed all echocardiographic parameters with patients LTSS regardless of their clinical presentation. In this survey, the RAVI and 3D RV end-diastolic and end-systolic volume indices were significantly higher in patients with severe lung involvement in comparison to non-Severe lung involvement and no lung involvement. 3D RV EF, SVI, and RVFW strain were comparable among all groups. In the Covid-Wase study, 33% of hospitalized patients had increased RV basal diameters in the acute phase; in 120 days follow up, those with dilated RV improved significantly, although the mean RV basal diameter remained increased [16, 17, 18, 19, 20]. We demonstrated increased right chambers volumes in patients with extensive lung involvement in the early recovery phase while both RV function and strain are preserved. Despite this, one of the right atrial functional metrics, RA reservoir strain, was significantly lower in severe lung involvement compared to “no lung involvement” (48 ± 10 vs. 36 ± 9, P-value = 0.05). It emphasizes the rapid recovery of RV function; even so, increased right chambers volumes and decreased RA strain could be the imprints of severe pneumonia in the acute phase.
Conclusion
In this investigation of otherwise healthy health care workers infected with covid-19, 3D LV GLS, and 3D LV SVI were considerably lower in the early recovery phase in the Severe group compared to the mild group and correlated with hsCRP level in the acute phase. However, LA reservoir, and contraction strains were higher in this group, and the LAVI was lower, suggesting a paradoxical compensatory role or overcorrection in this phase. RV functional parameters and strain were normal, indicating RV’s ability for fast recovery.
Limitaions
All data were collected cross-sectionally in the early recovery phase and acute phase features were not recorded due to the high transmission capability of potentially life-threatening coronavirus infection. Longer follow-up data could be worth comparing and is under investigation.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Schaller T, Hirschbühl K, Burkhardt K, Braun G, Trepel M, Märkl B, Claus R (2020) Postmortem examination of patients with COVID-19. JAMA 323(24):2518–2520
Lala A, Johnson K, Januzzi J et al (2020) Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol 76(5):533–546. https://doi.org/10.1016/j.jacc.2020.06.007
Ni W, Yang X, Liu J, Bao J, Li R, Xu Y et al (2020) Acute myocardial injury at hospital admission is associated with all-cause mortality in COVID-19. J Am Coll Cardiol 76(1):124–125. https://doi.org/10.1016/j.jacc.2020.05.007. V.O
Nishiga M, Wang DW, Han Y et al (2020) COVID-19, and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol 17:543–558. https://doi.org/10.1038/s41569-020-0413-9
Dan S, Pant M, Upadhyay SK (2020) The case fatality rate in COVID-19 patients with cardiovascular disease: global health challenge and paradigm in the current pandemic. Curr Pharmacol Rep 6:1–10. https://doi.org/10.1007/s40495-020-00239-0
Puntmann VO, Carerj ML, Wieters I et al (2020) Outcomes of Cardiovascular magnetic resonance imaging in patients recently recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 5(11):1265–1273. https://doi.org/10.1001/jamacardio.2020.3557
Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, Simonetti OP, Daniels CJ (2021) Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol 6(1):116–118
Gandhi RT et al (2020) Mild or moderate Covid-19.“ New England. J Med 383(18):1757–1766. https://doi.org/10.1056/NEJMcp2009249
Li K, Fang Y, Li W et al (2020) CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19). Eur Radiol 30:4407–4416. https://doi.org/10.1007/s00330-020-06817-6
Nagueh SF et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the european. Assoc Cardiovasc Imag "Eur J Echocardiogr 17(12):1321–1360. https://doi.org/10.1093/ejechocard/jep2007
Badano LP et al (2018) Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task force to standardize deformation imaging. Eur Heart J-Cardiovasc Imag 19(6):591–600. https://doi.org/10.1093/ehjci/jey042
Bernard A, Addetia K, Dulgheru R, Caballero L, Sugimoto T, Akhaladze N, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Hagendorff A, Hristova K, Ilardi F, Lopez T, de la Morena G, Popescu BA, Penicka M, Ozyigit T, David Rodrigo Carbonero J, van de Veire N, Von Bardeleben S, Vinereanu R, Luis Zamorano D, Martinez J, Magne C, Cosyns J, Donal B, Habib E, Badano G, Lang LP, Lancellotti RM (2017) P 3D echocardiographic reference ranges for normal left ventricular volumes and strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imag 18(4):475–483. https://doi.org/10.1093/ehjci/jew284. (PMID: 28329230)
Lassen MC, Højbjerg, et al (2020) Echocardiographic abnormalities and predictors of mortality in hospitalized COVID-19 patients: the ECHOVID-19 study. ESC heart failure 7(6):4189–4197. https://doi.org/10.1002/ehf2.13044
Baycan OF, Barman HA, Atici A et al (2021) Evaluation of biventricular function in patients with COVID-19 using speckle tracking echocardiography. Int J Cardiovasc Imaging 37:135–144. https://doi.org/10.1007/s10554-020-01968-5
Karagodin I, Carvalho Singulane C, Woodward GM, Xie M, Tucay ES, Tude Rodrigues AC, Vasquez-Ortiz ZY, Alizadehasl A, Monaghan MJ, Ordonez Salazar BA, Soulat-Dufour L, Mostafavi A, Moreo A, Citro R, Narang A, Wu C, Descamps T, Addetia K, Lang RM, Asch FM (2021) WASE-COVID investigators echocardiographic correlates of in-hospital death in patients with acute COVID-19 infection: the World Alliance Societies of Echocardiography (WASE-COVID) study. J Am Soc Echocardiogr 34(8):819–830
Bhatia HS, Bui QM, King K, DeMaria A, Daniels LB (2021) Subclinical left ventricular dysfunction in COVID-19. Int J Cardiol Heart Vasc 34:100770. https://doi.org/10.1016/j.ijcha.2021.100770
Li R, Wang H, Ma F et al (2021) Widespread myocardial dysfunction in COVID-19 patients detected by myocardial strain imaging using 2-D speckle-tracking echocardiography. Acta Pharmacol Sin 42:1567–1574. https://doi.org/10.1038/s41401-020-00595-z
Turan T et al (2021) Left ventricular global longitudinal strain in low cardiac risk outpatients who recently recovered from coronavirus disease 2019. Int J Cardiovasc Imag 37(10):2979–2989. https://doi.org/10.1007/s10554-021-02376-z
Karagodin I et al (2021) Ventricular changes in patients with Acute COVID-19 infection: Follow-Up of the World Alliance Societies of Echocardiography (WASE-COVID) study. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2021.10.015
Szekely Y (2020) Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation 142:342–353
Li Y et al (2020) Prognostic value of right ventricular longitudinal strain in patients with COVID-19. Cardiovasc Imag 13(11):2287–2299
Popescu BA et al (2005) Right ventricular functional recovery after acute myocardial infarction: relation with left ventricular function and interventricular septum motion GISSI-3 echo substudy. Heart 91(4):484–488. https://doi.org/10.1136/hrt.2003.028050
Baruch G et al (2021) Evolution of right and left ventricle routine and speckle-tracking echocardiography in patients recovering from coronavirus disease 2019: a longitudinal study. Eur Heart J: Cardiovasc Imag 23(8):1055–1065. https://doi.org/10.1093/ehjci/jeab190
Goerlich E et al (2021) Left atrial function in patients with COVID-19 and its association with incident atrial fibrillation/flutter. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2021.05.015
Beyls C, Hermida A, Bohbot Y et al (2021) Automated left atrial strain analysis for predicting atrial fibrillation in severe COVID-19 pneumonia: a prospective study. Ann Intensive Care 11:168. https://doi.org/10.1186/s13613-021-00955-w
Xie Y et al (2020) Biventricular longitudinal strain Predict Mortality in COVID-19 patients. Front Cardiovasc Med 7:418. https://doi.org/10.3389/fcvm.2020.632434
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Author information
Authors and Affiliations
Contributions
NS: concept and design of the study, BGH: methodology, NSH: resources, management of covid patients, MK: clinical data collection, ZR: echocardiographic images acquisition, ZR: three-dimensional analysis of echocardiographic acquisitions, SA: interpretation of computed tomographic scans, YR: statistical analysis, ZR and YR: drafting the manuscript, NS, ZR, YR: editing and approval of the final version of manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Research involving human and animal participants
All procedures were according to the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and its modifications.
Informed consent
All patients signed written informed consent and gave permission for being included in this study and publication of it.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Samiei, N., Rahnamoun, Z., Kamali, M. et al. Paradoxical increase in left atrial strains early after Covid-19 infection, a result of comprehensive recovery phase four-chamber strains study. Int J Cardiovasc Imaging 39, 1437–1447 (2023). https://doi.org/10.1007/s10554-023-02865-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02865-3