Abstract
Purpose
To investigate the association of the degree of stent expansion, as assessed by optical coherence tomography (OCT), following stent implantation, and clinical outcomes in ST-segment elevation myocardial infarction (STEMI) patients.
Methods
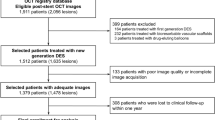
STEMI patients from the MATRIX (Minimizing Adverse Haemorrhagic Events by TRansradial Access Site and angioX) OCT study were selected; Clinical outcomes were collected through 1 year. Stent expansion index is a minimum stent area (MSA) divided by average lumen area (average of proximal and distal reference lumen area). The following variables were measured: MSA (< 4.5mm2), dissection (> 200 µm in width and < 5 mm from stent segment), malapposition (> 200 µm distance of stent from vessel wall), a thrombus (area > 5% of lumen area) were compared.
Results
A total of 151 patients were included; after excluding patients with suboptimal OCT quality, the population with available OCT was classified into 2 groups: under–expanded < 90% (N = 72, 51%) and well–expanded ≥ 90% (N = 67, 49%). In the well–expanded group, a significant number of the proximal vessels had a lumen area < 4.5mm2 (16.1%, p < 0.001) and a greater thrombus burden within stent (56.7%, p = 0.042). The overall 30 day and 1 year major adverse cardiovascular event (MACE) rates were 5% and 6.1%, respectively.
Conclusion
Irrespective of the degree of stent expansion, the OCT findings, in STEMI patients, and the MACE at 30 days and one year follow up was low; further, well–expanded stents led to a more significant residual thrombotic burden within the stent but seemed to have insignificant clinical impact. Acknowledged stent optimization criteria, traditionally related to worse outcomes in stable patients, do not seem to be associated with worse outcomes in this STEMI population.



Similar content being viewed by others
Abbreviations
- ACS:
-
Acute coronary syndrome
- MACE:
-
Major adverse cardiovascular event
- MLA:
-
Minimum lumen area
- MSA:
-
Minimum stent area
- NSTEMI:
-
Non-ST segment elevation myocardial infarction
- OCT:
-
Optical coherence tomography
- PCI:
-
Percutaneous coronary intervention
- PPCI:
-
Primary percutaneous coronary intervention
- STEMI:
-
ST segment elevation myocardial infarction
References
Koskinas KC, Ughi GJ, Windecker S, Tearney GJ, Räber L (2016) Intracoronary imaging of coronary atherosclerosis: validation for diagnosis, prognosis and treatment. Eur Heart J 37(6):524–535
Ali ZA, Maehara A, Généreux P, Shlofmitz RA, Fabbiocchi F, Nazif TM et al (2016) Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet Lond Engl 388(10060):2618–28
Prati F, Romagnoli E, Burzotta F, Limbruno U, Gatto L, La Manna A et al (2015) Clinical impact of OCT findings during PCI: the CLI-OPCI II study. JACC Cardiovasc Imaging 8(11):1297–1305
Valgimigli M, Frigoli E, Leonardi S, Vranckx P, Rothenbühler M, Tebaldi M et al (2018) Radial versus femoral access and bivalirudin versus unfractionated heparin in invasively managed patients with acute coronary syndrome (MATRIX): final 1-year results of a multicentre, randomised controlled trial. Lancet Lond Engl 392(10150):835–848
Valgimigli M, Frigoli E, Leonardi S, Rothenbühler M, Gagnor A, Calabrò P et al (2015) Bivalirudin or unfractionated heparin in acute coronary syndromes. N Engl J Med 373(11):997–1009
Gargiulo G, Carrara G, Frigoli E, Vranckx P, Leonardi S, Ciociano N et al (2018) Bivalirudin or heparin in patients undergoing invasive management of acute coronary syndromes. J Am Coll Cardiol. 71(11):1231–1242
Garcia-Garcia HM, Picchi A, Sardella G, Adamo M, Frigoli E, Limbruno U et al (2019) Comparison of intra-procedural vs. post-stenting prolonged bivalirudin infusion for residual thrombus burden in patients with ST-segment elevation myocardial infarction undergoing: the MATRIX (Minimizing Adverse Haemorrhagic Events by TRansradial Access Site and angioX) OCT study. Eur Heart J Cardiovasc Imaging 20(12):1418–1428
Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG et al (2012) Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol 59(12):1058–1072
Imola F, Mallus MT, Ramazzotti V, Manzoli A, Pappalardo A, GiorgioDi A et al (2010) Safety and feasibility of frequency domain optical coherence tomography to guide decision making in percutaneous coronary intervention. EuroIntervention 6(5):575–581
Bezerra HG, Costa MA, Guagliumi G, Rollins AM, Simon DI (2009) Intracoronary optical coherence tomography: a comprehensive review clinical and research applications. JACC Cardiovasc Interv 2(11):1035–1046
Kuku KO, Ekanem E, Azizi V, Melaku G, Bui A, Meirovich YF et al (2018) Optical coherence tomography-guided percutaneous coronary intervention compared with other imaging guidance: a meta-analysis. Int J Cardiovasc Imaging 34(4):503–513
Steinvil A, Zhang Y-J, Lee SY, Pang S, Waksman R, Chen S-L et al (2016) Intravascular ultrasound-guided drug-eluting stent implantation: an updated meta-analysis of randomized control trials and observational studies. Int J Cardiol 216:133–139
Kubo T, Akasaka T, Shite J, Suzuki T, Uemura S, Yu B et al (2013) OCT compared with IVUS in a coronary lesion assessment: the OPUS-CLASS study. JACC Cardiovasc Imaging 6(10):1095–1104
Fujii K, Carlier SG, Mintz GS, Yang Y, Moussa I, Weisz G et al (2005) Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: an intravascular ultrasound study. J Am Coll Cardiol 45(7):995–998
Hong M-K, Mintz GS, Lee CW, Park D-W, Choi B-R, Park K-H et al (2006) Intravascular ultrasound predictors of angiographic restenosis after sirolimus-eluting stent implantation. Eur Heart J 27(11):1305–1310
Morino Y, Honda Y, Okura H, Oshima A, Hayase M, Bonneau HN et al (2001) An optimal diagnostic threshold for minimal stent area to predict target lesion revascularization following stent implantation in native coronary lesions. Am J Cardiol 88(3):301–303
Doi H, Maehara A, Mintz GS, Yu A, Wang H, Mandinov L et al (2009) Impact of post-intervention minimal stent area on 9-month follow-up patency of paclitaxel-eluting stents: an integrated intravascular ultrasound analysis from the TAXUS IV, V, and VI and TAXUS ATLAS Workhorse, Long Lesion, and Direct Stent Trials. JACC Cardiovasc Interv 2(12):1269–1275
Meneveau N, Souteyrand G, Motreff P, Caussin C, Amabile N, Ohlmann P et al (2016) Optical coherence tomography to optimize results of percutaneous coronary intervention in patients with non-ST-elevation acute coronary syndrome: results of the multicenter, randomized DOCTORS study (Does Optical Coherence Tomography Optimize Results of Stenting). Circulation 134(13):906–917
Kubo T, Shinke T, Okamura T, Hibi K, Nakazawa G, Morino Y et al (2017) Optical frequency domain imaging vs. intravascular ultrasound in percutaneous coronary intervention (OPINION trial): one-year angiographic and clinical results. Eur Heart J 38(42):3139–3147
Prati F, VitoDi L, Biondi-Zoccai G, Occhipinti M, MannaLa A, Tamburino C et al (2012) Angiography alone versus angiography plus optical coherence tomography to guide decision-making during percutaneous coronary intervention: the Centro per la Lotta contro l’Infarto-Optimisation of Percutaneous Coronary Intervention (CLI-OPCI) study. EuroIntervention 8(7):823–829
Kim J-S, Shin D-H, Kim B-K, Ko Y-G, Choi D, Jang Y et al (2015) Randomized comparison of stent strut coverage following angiography- or optical coherence tomography-guided percutaneous coronary intervention. Rev Espanola Cardiol Engl Ed 68(3):190–197
Antonsen L, Thayssen P, Maehara A, Hansen HS, Junker A, Veien KT et al (2015) Optical coherence tomography guided percutaneous coronary intervention with nobori stent implantation in patients with Non-ST-Segment-Elevation Myocardial Infarction (OCTACS) trial: difference in strut coverage and dynamic malapposition patterns at 6 months. Circ Cardiovasc Interv 8(8):e002446
Kala P, Cervinka P, Jakl M, Kanovsky J, Kupec A, Spacek R et al (2018) OCT guidance during stent implantation in primary PCI: a randomized multicenter study with nine months of optical coherence tomography follow-up. Int J Cardiol 1(250):98–103
Acknowledgement
None
Funding
Dr. Varbella reports personal fees from chiesi, personal fees from bayer, personal fees from astrazeneca, personal fees from daichisankyo, personal fees from boeringher, personal fees from pfizer BMS, personal fees from menarini, personal fees from servier, personal fees from Alvimedica CID, personal fees from Stentys, personal fees from Abbott vascular, grants from Sanitex, grants from Biotronik, outside the submitted work. Dr. Ando’ reports non-financial support from Terumo, during the conduct of the study; personal fees from Daiichi-Sankyo, personal fees and non-financial support from Bayer, personal fees from Pfizer-BMS, non-financial support from Boeringer-Ingelheim, personal fees from AstraZeneca, personal fees and non-financial support from Menarini, non-financial support from Abbott, non-financial support from Philips Volcano, non-financial support from Boston Scientific, outside the submitted work. Dr. Valgimigli reports grants from Medtronic, personal fees from Abbott, personal fees from Chiesi, personal fees from Bayer, personal fees from Servier, personal fees from Boeringher, personal fees from Daiichi Sankyo, outside the submitted work;
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The other authors report nothing to disclose
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All the author takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation
Rights and permissions
About this article
Cite this article
Yacob, O., Garcia-Garcia, H.M., Dan, K. et al. Impact of optical coherence tomography findings on clinical outcomes in ST-segment elevation myocardial infarction patients: a MATRIX (Minimizing Adverse Hemorrhagic Events by Trans-radial Access Site and angioX) OCT sub-study. Int J Cardiovasc Imaging 37, 1143–1150 (2021). https://doi.org/10.1007/s10554-020-02098-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02098-8