Abstract
Purpose
The association between smoking and the risk of skin cancers has been studied without reaching consistent findings. This study aims to assess this association through an updated meta-analysis of cohort studies.
Methods
We retrieved cohort studies that investigated the temporal association between smoking and the risk of basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and malignant melanoma (MM). Pooled relative risks (RRs) and confidence intervals (CIs) of the included articles were calculated for current, former, and heavy smoking compared with never smoking. Publication bias was detected using the Egger’s regression.
Results
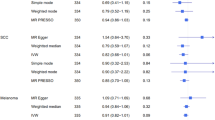
A total of 15 studies, published between 1990 and 2018, were included. Current smoking was associated with a higher risk of SCC (pooled RR = 1.32, 95% CI 1.15, 1.52) but with a lower risk of BCC (pooled RR = 0.85, 95% CI 0.75, 0.96) and MM (pooled RR = 0.72, 95% CI 0.64, 0.82). No publication bias was detected, and no single study had a substantial impact on the pooled results. Similar results were detected for heavy smoking, while former smoking was not associated with the risk of skin cancer.
Conclusion
Current smoking and heavy smoking were associated with a higher risk of SCC but a decreased risk of BCC and MM, while former smoking was not associated with skin cancer risk.




Similar content being viewed by others
References
Perera E, Gnaneswaran N, Staines C et al (2015) Incidence and prevalence of non-melanoma skin cancer in Australia: a systematic review. Aust J Dermatol 56:258–267
Whiteman DC, Green AC, Olsen CM (2016) The growing burden of invasive melanoma: projections of incidence rates and numbers of new cases in six susceptible populations through 2031. J Invest Dermatol 136:1161–1171
Apalla Z, Nashan D, Weller R et al (2017) Skin cancer: epidemiology, disease burden, pathophysiology, diagnosis, and therapeutic approaches. Dermatol Ther 7:5–19
Etzkorn JR, Parikh RP, Marzban SS et al (2013) Identifying risk factors using a skin cancer screening program. Cancer Control 20:248–254
Jacob L, Freyn M, Kalder M et al (2018) Impact of tobacco smoking on the risk of developing 25 different cancers in the UK: a retrospective study of 422,010 patients followed for up to 30 years. Oncotarget 9:17420–17429
Song F, Qureshi AA, Gao X et al (2012) Smoking and risk of skin cancer: a prospective analysis and a meta-analysis. Int J Epidemiol 41:1694–1705
Pirie K, Beral V, Heath AK et al (2018) Heterogeneous relationships of squamous and basal cell carcinomas of the skin with smoking: the UK Million Women Study and meta-analysis of prospective studies. Br J Cancer 119:114–120
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ Clin Res Ed 339:b2535
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ Clin Res Ed 327:557–560
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ Clin Res Ed 315:629–634
Hunter DJ, Colditz GA, Stampfer MJ et al (1990) Risk factors for basal cell carcinoma in a prospective cohort of women. Ann Epidemiol 1:13–23
Karagas MR, Stukel TA, Greenberg ER et al (1992) Risk of subsequent basal cell carcinoma and squamous cell carcinoma of the skin among patients with prior skin cancer. Skin Cancer Prev Study Group JAMA 267:3305–3310
Veierod MB, Thelle DS, Laake P (1997) Diet and risk of cutaneous malignant melanoma: a prospective study of 50,757 Norwegian men and women. Int J Cancer 71:600–604
Freedman DM, Sigurdson A, Doody MM et al (2003) Risk of melanoma in relation to smoking, alcohol intake, and other factors in a large occupational cohort. Cancer Causes Control 4:847–857
Odenbro A, Bellocco R, Boffetta P et al (2005) Tobacco smoking, snuff dipping and the risk of cutaneous squamous cell carcinoma: a nationwide cohort study in Sweden. Br J Cancer 92:1326–1328
Odenbro A, Gillgren P, Bellocco R et al (2007) The risk for cutaneous malignant melanoma, melanoma in situ and intraocular malignant melanoma in relation to tobacco use and body mass index. Br J Dermatol 156:99–105
DeLancey JO, Hannan LM, Gapstur SM et al (2011) Cigarette smoking and the risk of incident and fatal melanoma in a large prospective cohort study. Cancer Causes Control 22:937–942
McBride P, Olsen CM, Green AC (2011) Tobacco smoking and cutaneous squamous cell carcinoma: a 16-year longitudinal population-based study. Cancer Epidemiol Biomark Prev 20:1778–1783
Blakely T, Barendregt JJ, Foster RH et al (2013) The association of active smoking with multiple cancers: national census-cancer registry cohorts with quantitative bias analysis. Cancer Causes Control 24:1243–1255
Hughes MC, Olsen CM, Williams GM et al (2014) A prospective study of cigarette smoking and basal cell carcinoma. Arch Dermatol Res 306:851–856
Henderson MT, Kubo JT, Desai M et al (2015) Smoking behavior and association of melanoma and nonmelanoma skin cancer in the Women's Health Initiative. J Am Acad Dermatol 72:190–191
Dusingize JC, Olsen CM, Pandeya NP et al (2017) Cigarette smoking and the risks of basal cell carcinoma and squamous cell carcinoma. J Invest Dermatol 137:1700–1708
Dusingize JC, Olsen CM, Pandeya N et al (2018) Smoking and cutaneous melanoma: findings from the QSkin Sun and Health Cohort Study. Cancer Epidemiol Biomark Prev 27:874–881
De Hertog SA, Wensveen CA, Bastiaens MT et al (2001) Relation between smoking and skin cancer. J Clin Oncol 19:231–238
D'Errico M, Calcagnile A, Iavarone I et al (1999) Factors that influence the DNA repair capacity of normal and skin cancer-affected individuals. Cancer Epidemiol Biomark Prev 8:553–559
Rees JR, Stukel TA, Perry AE et al (2007) Tea consumption and basal cell and squamous cell skin cancer: results of a case-control study. J Am Acad Dermatol 56:781–785
Kessides MC, Wheless L, Hoffman-Bolton J et al (2011) Cigarette smoking and malignant melanoma: a case-control study. J Am Acad Dermatol 64:84–90
Shors AR, Solomon C, McTiernan A et al (2001) Melanoma risk in relation to height, weight, and exercise (United States). Cancer Causes Control 12:599–606
Nan H, Xu M, Kraft P et al (2011) Genome-wide association study identifies novel alleles associated with risk of cutaneous basal cell carcinoma and squamous cell carcinoma. Hum Mol Genet 20:3718–3724
Stacey SN, Gudbjartsson DF, Sulem P et al (2008) Common variants on 1p36 and 1q42 are associated with cutaneous basal cell carcinoma but not with melanoma or pigmentation traits. Nat Genet 40:1313–1318
Sopori M (2002) Effects of cigarette smoke on the immune system. Nat Rev Immunol 2:372–377
Yerger VB, Malone RE (2006) Melanin and nicotine: a review of the literature. Nicotine Tob Res 8:487–498
Grant WB (2008) Skin aging from ultraviolet irradiance and smoking reduces risk of melanoma: epidemiological evidence. Anticancer Res 28:4003–4008
Thompson CA, Zhang ZF, Arah OA (2013) Competing risk bias to explain the inverse relationship between smoking and malignant melanoma. Eur J Epidemiol 28:557–567
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arafa, A., Mostafa, A., Navarini, A.A. et al. The association between smoking and risk of skin cancer: a meta-analysis of cohort studies. Cancer Causes Control 31, 787–794 (2020). https://doi.org/10.1007/s10552-020-01319-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-020-01319-8