Abstract
Objective
To investigate ovarian function and therapeutic efficacy among estrogen receptor (ER)-positive, premenopausal breast cancer patients treated with gonadotropin-releasing hormone agonist (GnRHa) and chemotherapy simultaneously or sequentially.
Method
This study was a phase 3, open-label, parallel, randomized controlled trial (NCT01712893). Two hundred sixteen premenopausal patients (under 45 years) diagnosed with invasive ER-positive breast cancer were enrolled from July 2009 to May 2013 and randomized at a 1:1 ratio to receive (neo)adjuvant chemotherapy combined with sequential or simultaneous GnRHa treatment. All patients were advised to receive GnRHa for at least 2 years. The primary outcome was the incidence of early menopause, defined as amenorrhea lasting longer than 12 months after the last chemotherapy or GnRHa dose, with postmenopausal or unknown follicle-stimulating hormone and estradiol levels. The menstrual resumption period and survivals were the secondary endpoints.
Result
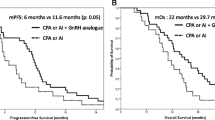
The median follow-up time was 56.9 months (IQR 49.5–72.4 months). One hundred and eight patients were enrolled in each group. Among them, 92 and 78 patients had complete primary endpoint data in the sequential and simultaneous groups, respectively. The rates of early menopause were 22.8% (21/92) in the sequential group and 23.1% (18/78) in the simultaneous group [simultaneous vs. sequential: OR 1.01 (95% CI 0.50–2.08); p = 0.969; age-adjusted OR 1.13; (95% CI 0.54–2.37); p = 0.737]. The median menstruation resumption period was 12.0 (95% CI 9.3–14.7) months and 10.3 (95% CI 8.2–12.4) months for the sequential and simultaneous groups, respectively [HR 0.83 (95% CI 0.59–1.16); p = 0.274; age-adjusted HR 0.90 (95%CI 0.64–1.27); p = 0.567]. No significant differences were evident for disease-free survival (p = 0.290) or overall survival (p = 0.514) between the two groups.
Conclusion
For ER-positive premenopausal patients, the sequential use of GnRHa and chemotherapy showed ovarian preservation and survival outcomes that were no worse than simultaneous use. The application of GnRHa can probably be delayed until menstruation resumption after chemotherapy.


Similar content being viewed by others
References
Anders CK, Johnson R, Litton J et al (2009) Breast cancer before age 40 years. Semin Oncol 36:237–249
Ewertz M, Jensen AB (2011) Late effects of breast cancer treatment and potentials for rehabilitation. Acta Oncol 50:187–193
Jain S, Santa-Maria CA, Gradishar WJ (2015) The role of ovarian suppression in premenopausal women with hormone receptor-positive early-stage breast cancer. Oncology (Williston Park) 29(473–478):481
Moore HC, Unger JM, Phillips KA et al (2015) Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. N Engl J Med 372:923–932
Del ML, Boni L, Michelotti A et al (2011) Effect of the gonadotropin-releasing hormone analogue triptorelin on the occurrence of chemotherapy-induced early menopause in premenopausal women with breast cancer: a randomized trial. JAMA 306:269–276
Lambertini M, Ceppi M, Poggio F et al (2015) Ovarian suppression using luteinizing hormone-releasing hormone agonists during chemotherapy to preserve ovarian function and fertility of breast cancer patients: a meta-analysis of randomized studies. Ann Oncol 26:2408–2419
Lambertini M, Del ML, Pescio MC et al (2016) Cancer and fertility preservation: international recommendations from an expert meeting. BMC Med 14:1
Francis PA, Regan MM, Fleming GF et al (2015) Adjuvant ovarian suppression in premenopausal breast cancer. N Engl J Med 372:436–446
Pagani O, Regan MM, Walley BA et al (2014) Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. N Engl J Med 371:107–118
Petrek JA, Naughton MJ, Case LD et al (2006) Incidence, time course, and determinants of menstrual bleeding after breast cancer treatment: a prospective study. J Clin Oncol 24:1045–1051
Iwase A, Nakamura T, Nakahara T et al (2015) Anti-Mullerian hormone and assessment of ovarian reserve after ovarian toxic treatment: a systematic narrative review. Reprod Sci 22:519–526
Qiu L, Fu F, Huang M et al (2016) Evaluating the survival benefit following ovarian function suppression in premenopausal patients with hormone receptor positive early breast cancer. Sci Rep 6:26627
Francis PA, Regan MM, Fleming GF et al (2015) Adjuvant ovarian suppression in premenopausal breast cancer. N Engl J Med 372:436–446
Song G, Gao H, Yuan Z (2013) Effect of leuprolide acetate on ovarian function after cyclophosphamide-doxorubicin-based chemotherapy in premenopausal patients with breast cancer: results from a phase II randomized trial. Med Oncol 30:667
Sverrisdottir A, Nystedt M, Johansson H, Fornander T (2009) Adjuvant goserelin and ovarian preservation in chemotherapy treated patients with early breast cancer: results from a randomized trial. Breast Cancer Res Treat 117:561–567
Leonard R, Adamson D, Anderson R et al (2010) Hormone levels in the option trial show no ovarian protection by goserelin in adjuvant chemotherapy for early breast cancer—an anglo-celtic collaborative group and NCRN trial. Cancer Res. https://doi.org/10.1158/0008-5472.SABCS10-P5-13-07
Munster PN, Moore AP, Ismail-Khan R et al (2012) Randomized trial using gonadotropin-releasing hormone agonist triptorelin for the preservation of ovarian function during (neo)adjuvant chemotherapy for breast cancer. J Clin Oncol 30:533–538
Gerber B, von Minckwitz G, Stehle H et al (2011) Effect of luteinizing hormone-releasing hormone agonist on ovarian function after modern adjuvant breast cancer chemotherapy: the GBG 37 ZORO study. J Clin Oncol 29:2334–2341
Li J, Liu G, Yu K et al (2015) Effect of using LHRH analog during chemotherapy (CT) on premature ovarian failure and prognosis in premenopausal patients with early-stage, hormone receptor-positive breast cancer: the primary analysis of a randomized controlled phase III trial. Cancer Res. https://doi.org/10.1158/1538-7445.SABCS14-P1-12-02
Swain SM, Jeong JH, Geyer CJ et al (2010) Longer therapy, iatrogenic amenorrhea, and survival in early breast cancer. N Engl J Med 362:2053–2065
Lambertini M, Boni L, Michelotti A et al (2015) Ovarian suppression with triptorelin during adjuvant breast cancer chemotherapy and long-term ovarian function, pregnancies, and disease-free survival: a randomized clinical trial. JAMA 314:2632–2640
Regan MM, Walley BA, Francis PA et al (2017) Concurrent and sequential initiation of ovarian function suppression with chemotherapy in premenopausal women with endocrine-responsive early breast cancer: an exploratory analysis of TEXT and SOFT. Ann Oncol 28:2225–2232
Lambertini M MHLR (2017) Pooled analysis of five randomized trials investigating temporary ovarian suppression with gonadotropin-releasing hormone analogs during chemotherapy as a strategy to preserve ovarian function and fertility in premenopausal early breast cancer patients. In: San Antonio breast cancer symposium 2017, San Anotonio, The United States
Acknowledgements
This work was supported by the Shanghai Committee of Science and Technology, China (grant 12DZ2260100), the Shanghai United Developing Technology Project of Municipal Hospitals (SHDC12010116), and the Key Clinical Program of the Ministry of Health (2010–2012). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have declared no conflicts of interest.
Ethical approval
This trial was approved by the review boards in Fudan University Shanghai Cancer Center (No. 090875-3). All patients provided written informed consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Y., Ji, Y., Li, J. et al. Sequential versus simultaneous use of chemotherapy and gonadotropin-releasing hormone agonist (GnRHa) among estrogen receptor (ER)-positive premenopausal breast cancer patients: effects on ovarian function, disease-free survival, and overall survival. Breast Cancer Res Treat 168, 679–686 (2018). https://doi.org/10.1007/s10549-018-4660-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4660-y