Abstract
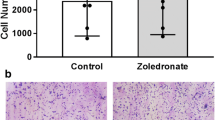
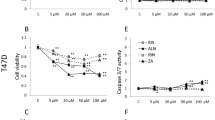
Bisphosphonates (BPs) are in clinical use for the treatment of breast cancer patients with bone metastases. Their anti-resorptive effect is mainly explained by inhibition of osteoclast activity, but recent evidence also points to a direct action of BPs on bone-forming osteoblasts. However, the mechanisms how BPs influence osteoblasts and their interactions with breast cancer cells are still poorly characterized. Human osteoblasts isolated from bone specimens were characterized in depth by their expression of osteogenic marker genes. The influence of the nitrogen-containing BPs zoledronate (Zol), ibandronate (Iban), and pamidronate (Pam) on molecular and cellular functions of osteoblasts was assessed focusing on cell proliferation and viability, apoptosis, cytokine secretion, and osteogenic-associated genes. Furthermore, effects of BPs on osteoblast–breast tumor cell interactions were examined in an established in vitro model system. The BPs Zol and Pam inhibited cell viability of osteoblasts. This effect was mediated by an induction of caspase-dependent apoptosis in osteoblasts. By interfering with the mevalonate pathway, Zol also reduces the proliferation of osteoblasts. The expression of phenotypic markers of osteogenic differentiation was altered by Zol and Pam. In addition, both BPs strongly influenced the secretion of the chemokine CCL2 by osteoblasts. Breast cancer cells also responded to Zol and Pam with a reduced cell adhesion to osteoblast-derived extracellular matrix molecules and with a decreased migration in response to osteoblast-secreted factors. BPs revealed prominent effects on human osteoblasts. Zol and Pam as the most potent BPs affected not only the expression of osteogenic markers, osteoblast viability, and proliferation but also important osteoblast–tumor cell interactions. Changing the osteoblast metabolism by BPs modulates migration and adhesion of breast cancer cells as well.








Similar content being viewed by others
Abbreviations
- BPs:
-
Bisphosphonates
- BrCa:
-
Breast cancer
- CCL2:
-
Chemokine, CC motif, ligand 2
- FPP:
-
Farnesyl pyrophosphate
- GGPP:
-
Geranylgeranyl pyrophosphate
- Iban:
-
Ibandronate
- MSCs:
-
Mesenchymal stem cells
- MTT:
-
3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide
- OB-CM:
-
Conditioned medium of the osteoblastic cell line CAL72
- Pam:
-
Pamidronate
- PARP1:
-
Poly (ADP-ribose) polymerase 1
- RCC:
-
Renal cell carcinoma
- Zol:
-
Zoledronate
References
Chiang AC, Massague J (2008) Molecular basis of metastasis. N Engl J Med 359(26):2814–2823
Guise TA, Brufsky A, Coleman RE (2010) Understanding and optimizing bone health in breast cancer. Curr Med Res Opin 26:3–20
Gnant M, Hadji P (2010) Prevention of bone metastases and management of bone health in early breast cancer. Breast Cancer Res 12(6):216
Kakonen SM, Mundy GR (2003) Mechanisms of osteolytic bone metastases in breast carcinoma. Cancer 97(3 Suppl):834–839
Lipton A, Theriault RL, Hortobagyi GN, Simeone J, Knight RD, Mellars K, Reitsma DJ, Heffernan M, Seaman JJ (2000) Pamidronate prevents skeletal complications and is effective palliative treatment in women with breast carcinoma and osteolytic bone metastases: long term follow-up of two randomized, placebo-controlled trials. Cancer 88(5):1082–1090
Body JJ, Bartl R, Burckhardt P, Delmas PD, Diel IJ, Fleisch H, Kanis JA, Kyle RA, Mundy GR, Paterson AH et al (1998) Current use of bisphosphonates in oncology. International Bone and Cancer Study Group. J Clin Oncol 16(12):3890–3899
Mundy GR, Yoneda T (1998) Bisphosphonates as anticancer drugs. N Engl J Med 339(6):398–400
Russell RG, Watts NB, Ebetino FH, Rogers MJ (2008) Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int 19(6):733–759
Luckman SP, Hughes DE, Coxon FP, Graham R, Russell G, Rogers MJ (1998) Nitrogen-containing bisphosphonates inhibit the mevalonate pathway and prevent post-translational prenylation of GTP-binding proteins, including Ras. J Bone Miner Res 13(4):581–589
Sahni M, Guenther HL, Fleisch H, Collin P, Martin TJ (1993) Bisphosphonates act on rat bone resorption through the mediation of osteoblasts. J Clin Invest 91(5):2004–2011
Vitte C, Fleisch H, Guenther HL (1996) Bisphosphonates induce osteoblasts to secrete an inhibitor of osteoclast-mediated resorption. Endocrinology 137(6):2324–2333
Fromigue O, Body JJ (2002) Bisphosphonates influence the proliferation and the maturation of normal human osteoblasts. J Endocrinol Invest 25(6):539–546
Xiong Y, Yang HJ, Feng J, Shi ZL, Wu LD (2009) Effects of alendronate on the proliferation and osteogenic differentiation of MG-63 cells. J Int Med Res 37(2):407–416
Corrado A, Neve A, Maruotti N, Gaudio A, Marucci A, Cantatore FP (2010) Dose-dependent metabolic effect of zoledronate on primary human osteoblastic cell cultures. Clin Exp Rheumatol 28(6):873–879
Viereck V, Emons G, Lauck V, Frosch KH, Blaschke S, Grundker C, Hofbauer LC (2002) Bisphosphonates pamidronate and zoledronic acid stimulate osteoprotegerin production by primary human osteoblasts. Biochem Biophys Res Commun 291(3):680–686
Frediani B, Spreafico A, Capperucci C, Chellini F, Gambera D, Ferrata P, Baldi F, Falsetti P, Santucci A, Bocchi L et al (2004) Long-term effects of neridronate on human osteoblastic cell cultures. Bone 35(4):859–869
Pan B, To LB, Farrugia AN, Findlay DM, Green J, Gronthos S, Evdokiou A, Lynch K, Atkins GJ, Zannettino AC (2004) The nitrogen-containing bisphosphonate, zoledronic acid, increases mineralisation of human bone-derived cells in vitro. Bone 34(1):112–123
Recker RR, Delmas PD, Halse J, Reid IR, Boonen S, Garcia-Hernandez PA, Supronik J, Lewiecki EM, Ochoa L, Miller P et al (2008) Effects of intravenous zoledronic acid once yearly on bone remodeling and bone structure. J Bone Miner Res 23(1):6–16
Garcia-Moreno C, Serrano S, Nacher M, Farre M, Diez A, Marinoso ML, Carbonell J, Mellibovsky L, Nogues X, Ballester J et al (1998) Effect of alendronate on cultured normal human osteoblasts. Bone 22(3):233–239
Greiner S, Kadow-Romacker A, Lubberstedt M, Schmidmaier G, Wildemann B (2007) The effect of zoledronic acid incorporated in a poly(D,L-lactide) implant coating on osteoblasts in vitro. J Biomed Mater Res A 80(4):769–775
Reinholz GG, Getz B, Pederson L, Sanders ES, Subramaniam M, Ingle JN, Spelsberg TC (2000) Bisphosphonates directly regulate cell proliferation, differentiation, and gene expression in human osteoblasts. Cancer Res 60(21):6001–6007
Senaratne SG, Colston KW (2002) Direct effects of bisphosphonates on breast cancer cells. Breast Cancer Res 4(1):18–23
Boissier S, Ferreras M, Peyruchaud O, Magnetto S, Ebetino FH, Colombel M, Delmas P, Delaisse JM, Clezardin P (2000) Bisphosphonates inhibit breast and prostate carcinoma cell invasion, an early event in the formation of bone metastases. Cancer Res 60(11):2949–2954
Senaratne SG, Pirianov G, Mansi JL, Arnett TR, Colston KW (2000) Bisphosphonates induce apoptosis in human breast cancer cell lines. Br J Cancer 82(8):1459–1468
Rachner TD, Singh SK, Schoppet M, Benad P, Bornhäuser M, Ellenrieder V, Ebert R, Jakob F, Hofbauer LC (2010) Zoledronic acid induces apoptosis and changes the TRAIL/OPG ratio in breast cancer cells. Cancer Lett 287(1):109–116
Dedes PG, Gialeli C, Tsonis AI, Kanakis I, Theocharis AD, Kletsas D, Tzanakakis GN, Karamanos NK (2012) Expression of matrix macromolecules and functional properties of breast cancer cells are modulated by the bisphosphonate zoledronic acid. Biochim Biophys Acta 1820(12):1926–1939
Coleman RE, Lipton A, Roodman GD, Guise TA, Boyce BF, Brufsky AM, Clezardin P, Croucher PI, Gralow JR, Hadji P et al (2010) Metastasis and bone loss: advancing treatment and prevention. Cancer Treat Rev 36(8):615–620
Burger JA, Kipps TJ (2006) CXCR4: a key receptor in the crosstalk between tumor cells and their microenvironment. Blood 107(5):1761–1767
Roodman DG (2003) Role of stromal-derived cytokines and growth factors in bone metastasis. Cancer 97(3 Suppl):733–738
Gillies RJ, Didier N, Denton M (1986) Determination of cell number in monolayer cultures. Anal Biochem 159(1):109–113
Dieterle A, Orth R, Daubrawa M, Grotemeier A, Alers S, Ullrich S, Lammers R, Wesselborg S, Stork B (2009) The Akt inhibitor triciribine sensitizes prostate carcinoma cells to TRAIL-induced apoptosis. Int J Cancer 125(4):932–941
Masuda T, Deng X, Tamai R (2009) Mouse macrophages primed with alendronate down-regulate monocyte chemoattractant protein-1 (MCP-1) and macrophage inflammatory protein-1alpha (MIP-1alpha) production in response to Toll-like receptor (TLR) 2 and TLR4 agonist via Smad3 activation. Int Immunopharmacol 9(9):1115–1121
Schüler Y, Lee-Thedieck C, Geiger K, Kaiser T, Ino Y, Aicher WK, Klein G (2012) Osteoblast-secreted factors enhance the expression of dysadherin and CCL2-dependent migration of renal carcinoma cells. Int J Cancer 130(2):288–299
Benford HL, McGowan NW, Helfrich MH, Nuttall ME, Rogers MJ (2001) Visualization of bisphosphonate-induced caspase-3 activity in apoptotic osteoclasts in vitro. Bone 28(5):465–473
Coleman ML, Olson MF (2002) Rho GTPase signalling pathways in the morphological changes associated with apoptosis. Cell Death Differ 9(5):493–504
Conti P, DiGioacchino M (2001) MCP-1 and RANTES are mediators of acute and chronic inflammation. Allergy Asthma Proc 22(3):133–137
Molloy AP, Martin FT, Dwyer RM, Griffin TP, Murphy M, Barry FP, O’Brien T, Kerin MJ (2009) Mesenchymal stem cell secretion of chemokines during differentiation into osteoblasts, and their potential role in mediating interactions with breast cancer cells. Int J Cancer 124(2):326–332
Li X, Qin L, Bergenstock M, Bevelock LM, Novack DV, Partridge NC (2007) Parathyroid hormone stimulates osteoblastic expression of MCP-1 to recruit and increase the fusion of pre/osteoclasts. J Biol Chem 282(45):33098–33106
Loberg RD, Day LL, Harwood J, Ying C, St John LN, Giles R, Neeley CK, Pienta KJ (2006) CCL2 is a potent regulator of prostate cancer cell migration and proliferation. Neoplasia 8(7):578–586
Lu Y, Cai Z, Galson DL, Xiao G, Liu Y, George DE, Melhem MF, Yao Z, Zhang J (2006) Monocyte chemotactic protein-1 (MCP-1) acts as a paracrine and autocrine factor for prostate cancer growth and invasion. Prostate 66(12):1311–1318
Loberg RD, Tantivejkul K, Craig M, Neeley CK, Pienta KJ (2007) PAR1-mediated RhoA activation facilitates CCL2-induced chemotaxis in PC-3 cells. J Cell Biochem 101(5):1292–1300
Kinder M, Chislock E, Bussard KM, Shuman L, Mastro AM (2008) Metastatic breast cancer induces an osteoblast inflammatory response. Exp Cell Res 314(1):173–183
Zhu J, Jia X, Xiao G, Kang Y, Partridge NC, Qin L (2007) EGF-like ligands stimulate osteoclastogenesis by regulating expression of osteoclast regulatory factors by osteoblasts: implications for osteolytic bone metastases. J Biol Chem 282(37):26656–26664
Qian BZ, Li J, Zhang H, Kitamura T, Zhang J, Campion LR, Kaiser EA, Snyder LA, Pollard JW (2011) CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature 475(7355):222–225
Festuccia C, Bologna M, Gravina GL, Guerra F, Angelucci A, Villanova I, Millimaggi D, Teti A (1999) Osteoblast conditioned media contain TGF-beta1 and modulate the migration of prostate tumor cells and their interactions with extracellular matrix components. Int J Cancer 81(3):395–403
Gallo M, De Luca A, Lamura L, Normanno N (2012) Zoledronic acid blocks the interaction between mesenchymal stem cells and breast cancer cells: implications for adjuvant therapy of breast cancer. Ann Oncol 23(3):597–604
Walter M, Liang S, Ghosh S, Hornsby PJ, Li R (2009) Interleukin 6 secreted from adipose stromal cells promotes migration and invasion of breast cancer cells. Oncogene 28(30):2745–2755
Knerr K, Ackermann K, Neidhart T, Pyerin W (2004) Bone metastasis: osteoblasts affect growth and adhesion regulons in prostate tumor cells and provoke osteomimicry. Int J Cancer 111(1):152–159
Nam JS, Kang MJ, Suchar AM, Shimamura T, Kohn EA, Michalowska AM, Jordan VC, Hirohashi S, Wakefield LM (2006) Chemokine (C–C motif) ligand 2 mediates the prometastatic effect of dysadherin in human breast cancer cells. Cancer Res 66(14):7176–7184
Acknowledgments
The authors thank Dr. Bernd Rolauffs (Center for Traumatology, BGU Hospital Tübingen) for his assistance in obtaining the bone specimens and Alice Mager for technical advice and help. This work was supported by a grant of the IZKF program of the Medical Faculty of the University of Tübingen (Grant No. 1686-0-0), by Novartis Pharma AG, Nürnberg, Germany, and by the DFG Graduate School 794. Part of this work was supported by Novartis Pharma AG (Nürnberg, Germany) to TK, GK, TF.
Author information
Authors and Affiliations
Corresponding authors
Additional information
* Gerd Klein and Tanja Fehm have contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kaiser, T., Teufel, I., Geiger, K. et al. Bisphosphonates modulate vital functions of human osteoblasts and affect their interactions with breast cancer cells. Breast Cancer Res Treat 140, 35–48 (2013). https://doi.org/10.1007/s10549-013-2613-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2613-z