Abstract
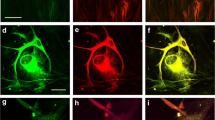
Glioblastoma is the most malignant and prevalent brain tumor in adults. It can grow and spread quickly causing harm to the brain health. One of the major challenges in treatment of glioblastoma is drug resistance. Use of synergistic combination of two drugs with different anti-tumor effects is nowadays highly considered in the development of effective therapeutic strategies for many malignancies. In the present study, we showed synergistic therapeutic efficacies of two chemical compounds, N-(4-hydroxyphenyl) retinamide (4HPR) and suberoylanilide hydroxamic acid (SAHA), for significant reduction in cell viability of rat C6 and human T98G glioblastoma cells. These compounds (4HPR and SAHA) were used alone or in synergistic combination for evaluating their various anti-tumor effects. The results showed that combination of 4HPR and SAHA significantly induced morphological and molecular features of astrocytic differentiation in C6 and T98G glioblastoma cells. Combination of 4HPR and SAHA proved to be an important therapeutic strategy for inhibiting cell growth and inducing differentiation in glioblastoma cells. Furthermore, combination of the two drugs showed more efficacies than either dug alone in reducing in vitro cell invasion (transwell assay), cell migration (wound healing assay), and angiogenesis (tube formation assay) due to down regulation of the molecules involved in these processes. The ultimate of goal of using this combination of drugs was induction of apoptosis. The results showed that these drugs in synergistic combination contributed highly to increases in morphological and molecular features of apoptotic death in the tumor cells. The results from molecular studies indicated that cell death occurred via activation of the extrinsic and intrinsic pathways of apoptosis in both C6 and T98G cells. The drugs in combination also contributed to dramatic inhibition of histone deacetylase 1, an important epigenetic player in promoting growth in glioblastoma cells. This novel combination of drugs should also be considered as a promising therapeutic strategy for the treatment of glioblastoma in vivo.







Similar content being viewed by others
References
Delgado-López PD, Corrales-García EM (2016) Survival in glioblastoma: a review on the impact of treatment modalities. Clin Transl Oncol 18(11):1062–1071. https://doi.org/10.1007/s12094-016-1497-x
Hottinger AF, Stupp R, Homicsko K (2014) Standards of care and novel approaches in the management of glioblastoma multiforme. Chin J Cancer 33(1):32–39. https://doi.org/10.5732/cjc.013.10207
Taylor MA, Das BC, Ray SK (2018) Targeting autophagy for combating chemoresistance and radioresistance in glioblastoma. Apoptosis 23(11–12):563–575. https://doi.org/10.1007/s10495-018-1480-9
van Tellingen O, Yetkin-Arik B, de Gooijer MC, Wesseling P, Wurdinger T, de Vries HE (2015) Overcoming the blood–brain tumor barrier for effective glioblastoma treatment. Drug Resist Updat 19:1–12. https://doi.org/10.1016/j.drup.2015.02.002
Stupp R, Brada M, van den Bent MJ, Tonn J-C, Pentheroudakis G (2014) High-grade glioma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25(suppl 3):iii93–iii101. https://doi.org/10.1093/annonc/mdu050
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups, National Cancer Institute of Canada Clinical Trials Group (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996. https://doi.org/10.1056/NEJMoa043330
Das A, Banik NL, Ray SK (2008) N-(4-Hydroxyphenyl) retinamide induced both differentiation and apoptosis in human glioblastoma T98G and U87MG cells. Brain Res 1227:207–215. https://doi.org/10.1016/j.brainres.2008.06.045
Holpuch AS, Phelps MP, Desai KG, Chen W, Koutras GM, Han BB, Warner BM, Pei P, Seghi GA, Tong M, Border MB, Fields HW, Stoner GD, Larsen PE, Liu Z, Schwendeman SP, Mallery SR (2012) Evaluation of a mucoadhesive fenretinide patch for local intraoral delivery: a strategy to reintroduce fenretinide for oral cancer chemoprevention. Carcinogenesis 33(5):1098–1105. https://doi.org/10.1093/carcin/bgs122
Zhang H, Mi JQ, Fang H, Wang Z, Wang C, Wu L, Zhang B, Minden M, Yang WT, Wang HW, Li JM, Xi XD, Chen SJ, Zhang J, Chen Z, Wang KK (2013) Preferential eradication of acute myelogenous leukemia stem cells by fenretinide. Proc Natl Acad Sci USA 110(14):5606–5611. https://doi.org/10.1073/pnas.1302352110
DiPietrantonio AM, Hsieh TC, Olson SC, Wu JM (1998) Regulation of G1/S transition and induction of apoptosis in HL-60 leukemia cells by fenretinide (4HPR). Int J cancer 78(1):53–61. https://doi.org/10.1002/(sici)1097-0215(19980925)78:1<53::aid-ijc10>3.0.co;2-6
Puduvalli VK, Saito Y, Xu R, Kouraklis GP, Levin VA, Kyritsis AP (1999) Fenretinide activates caspases and induces apoptosis in gliomas. Clin Cancer Res 5(8):2230–2235
Shibina A, Seidel D, Somanchi SS, Lee DA, Stermann A, Maurer BJ, Lode HN, Reynolds CP, Huebener N (2013) Fenretinide sensitizes multidrug-resistant human neuroblastoma cells to antibody-independent and ch14.18-mediated NK cell cytotoxicity. J Mol Med (Berl) 91(4):459–472. https://doi.org/10.1007/s00109-012-0958-0
George J, Banik NL, Ray SK (2010) Survivin knockdown and concurrent 4-HPR treatment controlled human glioblastoma in vitro and in vivo. Neuro Oncol 12(11):1088–1101. https://doi.org/10.1093/neuonc/noq079
Janardhanan R, Butler JT, Banik NL, Ray SK (2009) N-(4-Hydroxyphenyl) retinamide potentiated paclitaxel for cell cycle arrest and apoptosis in glioblastoma C6 and RG2 cells. Brain Res 1268(0 1):142–153. https://doi.org/10.1016/j.brainres.2009.02.064
Janardhanan R, Banik NL, Ray SK (2008) N-(4-Hydroxyphenyl) retinamide induced differentiation with repression of telomerase and cell cycle to increase interferon-γ sensitivity for apoptosis in human glioblastoma cells. Cancer Lett 261(1):26–36. https://doi.org/10.1016/j.canlet.2007.11.016
Mann BS, Johnson JR, Cohen MH, Justice R, Pazdur R (2007) FDA approval summary: vorinostat for treatment of advanced primary cutaneous T-cell lymphoma. Oncologist 12(10):1247–1252. https://doi.org/10.1634/theoncologist.12-10-1247
Lakshmaiah KC, Jacob LA, Aparna S, Lokanatha D, Saldanha SC (2014) Epigenetic therapy of cancer with histone deacetylase inhibitors. J Cancer Res Ther 10(3):469–478. https://doi.org/10.4103/0973-1482.137937
Diss E, Nalabothula N, Nguyen D, Chang E, Kwok Y, Carrier F (2014) Vorinostat (SAHA) promotes hyper-radiosensitivity in wild type p53 human glioblastoma cells. J Clin Oncol Res 2(1):1–16
Chiao MT, Cheng WY, Yang YC, Shen CC, Ko JL (2013) Suberoylanilide hydroxamic acid (SAHA) causes tumor growth slowdown and triggers autophagy in glioblastoma stem cells. Autophagy 9(10):1509–1526. https://doi.org/10.4161/auto.25664
Galanis E, Jaeckle KA, Maurer MJ, Reid JM, Ames MM, Hardwick JS, Reilly JF, Loboda A, Nebozhyn M, Fantin VR, Richon VM, Scheithauer B, Giannini C, Flynn PJ, Moore DF, Zwiebel J, Buckner JC (2009) Phase II trial of vorinostat in recurrent glioblastoma multiforme: a north central cancer treatment group study. J Clin Oncol 27(12):2052–2058. https://doi.org/10.1200/JCO.2008.19.0694
Galanis E, Anderson SK, Miller CR, Sarkaria JN, Jaeckle K, Buckner JC, Ligon KL, Ballman KV, Moore DF, Nebozhyn M, Loboda A, Schiff D, Ahluwalia MS, Lee EQ, Gerstner ER, Lesser GJ, Prados M, Grossman SA, Cerhan J, Giannini C, Wen PY, Alliance for Clinical Trials in Oncology and ABTC (2018) Phase I/II trial of vorinostat combined with temozolomide and radiation therapy for newly diagnosed glioblastoma: results of Alliance N0874/ABTC 02. Neuro Oncol 20(4):546–556. https://doi.org/10.1093/neuonc/nox161
Chou TC (2010) Drug combination studies and their synergy quantification using the Chou-Talalay method. Cancer Res 70(2):440–446. https://doi.org/10.1158/0008-5472.CAN-09-1947
Oberhammer FA, Hochegger K, Fröschl G, Tiefenbacher R, Pavelka M (1994) Chromatin condensation during apoptosis is accompanied by degradation of lamin A + B, without enhanced activation of cdc2 kinase. J Cell Biol 126(4):827–837. https://doi.org/10.1083/jcb.126.4.827
Ostrom QT, Gittleman H, Xu J, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS (2016) CBTRUS Statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2009–2013. Neuro Oncol 18(suppl_5):v1–v75. https://doi.org/10.1093/neuonc/now207
Lathia JD, Mack SC, Mulkearns-Hubert EE, Valentim CLL, Rich JN (2015) Cancer stem cells in glioblastoma. Genes Dev 29(12):1203–1217. https://doi.org/10.1101/gad.261982.115
Dror N, Mandel M, Lavie G (2013) Unique anti-glioblastoma activities of hypericin are at the crossroad of biochemical and epigenetic events and culminate in tumor cell differentiation. PLoS ONE 8(9):e73625. https://doi.org/10.1371/journal.pone.0073625
Ivanov VN, Hei TK (2014) Radiation-induced glioblastoma signaling cascade regulates viability, apoptosis and differentiation of neural stem cells (NSC). Apoptosis 19(12):1736–1754. https://doi.org/10.1007/s10495-014-1040-x
Aldaz B, Sagardoy A, Nogueira L, Guruceaga E, Grande L, Huse JT, Aznar MA, Díez-Valle R, Tejada-Solís S, Alonso MM, Fernandez-Luna JL, Martinez-Climent JA, Malumbres R (2013) Involvement of miRNAs in the differentiation of human glioblastoma multiforme stem-like cells. PLoS ONE 8(10):e77098. https://doi.org/10.1371/journal.pone.0077098
Yun K, Knittle P, Mantani A, Israel MA (2005) Id2 and Id4 expression and function in glioblastoma multiforme and neural stem cells. Cancer Res 65(9 Supplement):248
Zhao Z, He H, Wang C, Tao B, Zhou H, Dong Y, Xiang J, Wang L, Luo C, Lu Y, Yu X (2015) Downregulation of Id2 increases chemosensitivity of glioma. Tumour Biol 36(6):4189–4196. https://doi.org/10.1007/s13277-015-3055-5
Folkman J (2002) Role of angiogenesis in tumor growth and metastasis. Semin Oncol 29(6 Suppl 16):15–18. https://doi.org/10.1053/sonc.2002.37263
Chinot OL, Wick W, Mason W, Henriksson R, Saran F, Nishikawa R, Carpentier AF, Hoang-Xuan K, Kavan P, Cernea D, Brandes AA, Hilton M, Abrey L, Cloughesy T (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370(8):709–722. https://doi.org/10.1056/NEJMoa1308345
Ulukaya E, Wood EJ (1999) Fenretinide and its relation to cancer. Cancer Treat Rev 25(4):229–235. https://doi.org/10.1053/ctrv.1999.0127
Mourad PD, Farrell L, Stamps LD, Chicoine MR, Silbergeld DL (2005) Why are systemic glioblastoma metastases rare? Systemic and cerebral growth of mouse glioblastoma. Surg Neurol 63(6):511–519. https://doi.org/10.1016/j.surneu.2004.08.062 ( discussion 519)
Chaichana KL, Jusue-Torres I, Lemos AM, Gokaslan A, Cabrera-Aldana EE, Ashary A, Olivi A, Quinones-Hinojosa A (2014) The butterfly effect on glioblastoma: is volumetric extent of resection more effective than biopsy for these tumors? J Neurooncol 120(3):625–634. https://doi.org/10.1007/s11060-014-1597-9
Mattos JP, Marenco HA, Campos JM, Faria AV, Queiroz LS, Borges G, Oliveira (2006) Cerebellar glioblastoma multiforme in an adult. Arq Neuropsiquiatr 64(1):132–135. https://doi.org/10.1590/s0004-282x2006000100028
Timmons JJ, Zhang K, Fong J, Lok E, Swanson KD, Gautam S, Wong ET (2018) Literature review of spinal cord glioblastoma. Am J Clin Oncol 41(12):1281–1287. https://doi.org/10.1097/COC.0000000000000434
Paw I, Carpenter RC, Watabe K, Debinski W, Lo H-W (2015) Mechanisms regulating glioma invasion. Cancer Lett 362(1):1–7. https://doi.org/10.1016/j.canlet.2015.03.015
Malhotra V, Perry MC (2003) Classical chemotherapy: mechanisms, toxicities and the therapeutc window. Cancer Biol Ther 2(sup1):1–3. https://doi.org/10.4161/cbt.199
Taylor MA, Khathayer F, Ray SK (2019) Quercetin and sodium butyrate synergistically increase apoptosis in rat C6 and human T98G glioblastoma cells through inhibition of autophagy. Neurochem Res 44(7):1715–1725. https://doi.org/10.1007/s11064-019-02802-8
Saitoh Y, Goto T, Puduvalli VK, Murakami M, Kochi M, Levin VA, Kyritsis AP, Ushio Y (1999) Induction of apoptosis by N-(4-hydroxyphenyl)retinamide in glioma cells. Int J Oncol 15(3):499–504. https://doi.org/10.3892/ijo.15.3.499
Hsu CC, Chang WC, Hsu TI, Liu JJ, Yeh SH, Wang JY, Liou JP, Ko CY, Chang KY, Chuang JY (2016) Suberoylanilide hydroxamic acid represses glioma stem-like cells. J Biomed Sci 23(1):81. https://doi.org/10.1186/s12929-016-0296-6
Lohitesh K, Saini H, Srivastava A, Mukherjee S, Roy A, Chowdhury R (2018) Autophagy inhibition potentiates SAHA–mediated apoptosis in glioblastoma cells by accumulation of damaged mitochondria. Oncol Rep 39(6):2787–2796. https://doi.org/10.3892/or.2018.6373
Duvic M, Talpur R, Ni X, Zhang C, Hazarika P, Kelly C, Chiao JH, Reilly JF, Ricker JL, Richon VM, Frankel SR (2007) Phase 2 trial of oral vorinostat (suberoylanilide hydroxamic acid, SAHA) for refractory cutaneous T-cell lymphoma (CTCL). Blood 109(1):31–39. https://doi.org/10.1182/blood-2006-06-025999
Acknowledgements
This work was supported in part by an incentive award from the Soy Health Research Program (SHRP, United Soybean Board, Chesterfield, MO, USA), an Investigator Initiated Research grant (SCIRF-2015-I-0) from the South Carolina Spinal Cord Injury Research Fund (SCIRF, Columbia, SC, USA), and also the earlier R01 grants (CA91460 and NS057811) from the National Institutes of Health (Bethesda, MD, USA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khathayer, F., Taylor, M.A. & Ray, S.K. Synergism of 4HPR and SAHA increases anti-tumor actions in glioblastoma cells. Apoptosis 25, 217–232 (2020). https://doi.org/10.1007/s10495-020-01590-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-020-01590-9