Abstract
Active visualization, the use of dynamic representation of internal processes, is associated with increased knowledge and adherence to ART among people living with HIV. The current pilot intervention study tested the effectiveness of an online visualization for HIV prevention among 146 at-risk youth. Youth were randomized to a standard PrEP briefing or an online visualization. PrEP knowledge, attitudes, and uptake were self-reported at baseline and 3-months. Knowledge of PrEP increased, but there were no changes in preferences or uptake. Active visualization delivered online may be a useful educational tool for PrEP but not for shifting youth's uptake.
Similar content being viewed by others
Introduction
Pre-exposure prophylaxis (PrEP) implementation is a global priority to reduce HIV infection among high-risk populations [1]. PrEP has been found to dramatically reduce the rates of new HIV infections among those at-risk, with prevention rates as high as 90% [2, 3]. Although new HIV infection rates for most groups in the United States has leveled off, the number for those aged 13–24 remains high with over one fifth of new infections occurring in this group [4]. The highest number of new HIV infections occurred in men who have sex with other men (68%), transgender women (2%), and racial/ethnic minorities particularly Black (about 42%) and Latinx (27%) [5, 6]. With the growing rate of HIV infections among youth, there is a concurrent need to increase PrEP uptake and adherence.
Despite the promising potential of reducing HIV acquisition with PrEP, uptake and adherence to its strict routine is challenging, especially for youth [7]. Research in both the United States and globally has found several barriers to adherence such as low awareness and knowledge, concerns of side effects or safety (before and during use), low perceived risk around contracting HIV (or changing perceived risk), stigma (related to HIV, homophobia, and disclosing identity), lack of social support, ability to consent to treatment without parents, cost, and difficulty with the daily adherence regimen [8,9,10]. Around 50% of youth in studies that begin taking PrEP continued to have optimal adherence (daily use) by 6 months [3, 11]. Though many youth have reported being interested in PrEP and may start treatment, adherence dramatically decreased over time, especially as follow-up appointments begin to spread out to every 3 months [2].
Applying cognitive theories based on multisensory learning [12] and positive framing [13] through active visualizations offers an opportunity to address commonly cited barriers, such as a lack of knowledge about PrEP and how to maintain good adherence, which may, in turn, increase uptake and adherence to PrEP. Active visualizations are dynamic representations of internal processes of an illness or treatment [14], such as animations, computer models, or live demonstrations. They enable patients to “see” what is happening inside their body in terms of how their illness has occurred and the mode-of-action of a given treatment. By making these abstract concepts concrete and salient, visualizations may increase motivation and behaviors to try and reduce illness threat (e.g. adherence to treatment) [14]. Evidence suggests that visually presented information may increase memory for and understanding of health information [15], while also aligning with the cognitive models that patients have of their illness [16]. Active visualizations have been found to improve perceptions and health behaviors in several different illness groups, including kidney disease, HIV, cardiac disease, and cancer surgery (e.g., [17]).
An active visualization device was created to demonstrate how both ART and PrEP work inside the body to increase motivation to uptake and adhere to the medication [14]. This live demonstration using a 3-D visualization provides a simple, salient, and interactive demonstration of the utility of PrEP and ART, their potential benefits, and how to maintain medication adherence. In 2018, a randomized controlled trial in South Africa found that viewing the device resulted in clinically meaningful improvements in viral load at an 8-month follow-up in patients who were failing on regimen 1 or 2 ART [18]. This device was then adapted for use with youths to visualize how ART works in the body while simultaneously practicing medication adherence and interacting with their healthcare provider [19]. Youth who viewed the demonstration had lower viral loads, reported less difficulty in adhering to ART, and more motivation and control over their HIV than those not receiving the demonstration [19]. With the support that this active visualization may be an acceptable tool to address ART adherence among youth, the current study examined its effectiveness at improving preferences, knowledge, adherence, and uptake of PrEP among youth at high risk for HIV. To increase scalability of this intervention, we tested whether the active visualization could be effectively delivered online.
Methods
The Institutional Review Board of University of California Los Angeles approved this study (IRB#16-001858-AM-00007).
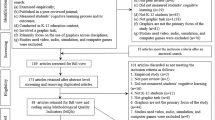
Participants
A random sample of youth at high risk for HIV were invited to participate between January and March 2020 from ATN 149, an ongoing randomized controlled trial for youth living at high risk for HIV (Adolescent Medicine Trials Network, Trial Registration #NCT03109431) [20]. ATN recruited youth aged 12–24 years old at homeless shelters, clinics, and community-based organizations working with sexual and gender minority diverse youth in high prevalence neighborhoods in Los Angeles, California, and New Orleans, Louisiana, from May 2017 to May 2020. At-risk for HIV was defined as reporting at least 3 of the following criteria: self-reporting as gay, bisexual, or transgender; African American or Latino race/ethnicity; having unprotected anal sex, sharing needles for injecting drugs, or an HIV-positive partner in the last 12 months; having been homeless (defined as not having a regular place to sleep for 3 or more months); illicit substance use (not including marijuana) in the last 12 months; having been hospitalized for a mental health disorder; having been in jail or on probation; having an STI in the last 12 months. Transgender and MSM youth were always eligible. These risk factors have also been associated with increased risk for HIV and SARS-CoV-2 infection [20]. If youth reported interest in other/future studies as part of the ATN 149, a research coordinator contacted youth by phone to describe the current study; coordinators contacted youth at random until the target sample size was obtained. Youth who expressed interest in participating were invited by research staff to provide voluntary and informed consent via zoom and using Qualtrics, survey analytic platform. Youth were randomized to: (1) verbal PrEP explanations delivered as part of standard care (SC) (n = 73) or (2) the demonstration model plus SC (n = 73). A similar proportion in the SC (n = 46) and intervention arms (n = 54) were assessed again 3 months later; the follow-up rate was 68%.
Standard Care and Medication Adherence Trainer Conditions
Standard Care (SC)
During the study, participants received a standard PrEP briefing as part of the ATN CARES study [20].
Intervention
In addition to SC, youth in the intervention received a 10-min one-on-one demonstration by a trained researcher. Following the stay-at-home orders in California in March 2020 amid the coronavirus outbreak, the demonstration [18, 19] was adapted to be used online via zoom. The demonstration used a human-body shaped container. At first, the container is filled with a ‘healthy body’ solution (water and sodium hydroxide) that is clear in color. The researcher then places a tablet representing PrEP ‘medication (soluble aspirin) into the body solution for each day of medication adherence, which results in a clear solution representing a “protected” body. A pink solution consisting of water, methanol, and phenolphthalein powder representing the HIV virus, is then added to the container. The body solution remains clear inside the container to demonstrate that HIV is unable to infect a “protected” body when adhering appropriately to daily PrEP. The research assistant also demonstrated a similar sequence to depict how PrEP 2-1-1 [21] works to protect the body (i.e., adding two tablets before and after the pink solution or exposure) and what happens in the case of non-adherence (the solution turns pink to depict the presence of a HIV infection).
Measures
All participants completed self-reported questionnaires at baseline and follow-up (3 months later) via a Qualtrics survey sent via text or email. Intervention youth also completed a post-demonstration questionnaire (details below).
Demographics
Age, gender identity, race, ethnicity, sex assigned at birth, sexual orientation, and current employment were assessed.
Knowledge of PrEP
Seven questions were included that assessed knowledge regarding adherence and effectiveness of PrEP, PrEP 2-1-1 [21], and PEP. The total number of correct items (out of seven possible items) was calculated.
Perceptions of HIV and PrEP
Items from the Brief Illness Perception Questionnaire [22] adapted for HIV infection were used to assess the participant’s perceptions about HIV (consequences, timeline, personal control, identity, concern, understanding, emotional response, and control). Additional Likert scale items [ranging from 0 (minimum) to 10 (maximum)] on the same response format asked participants about other related perceptions, including their motivation, concerns, difficulties taking PrEP, perceived risk of HIV severity, seriousness beliefs about HIV, and their relationship to their healthcare provider.
Preferences
Youth ranked their preferences for using PrEP daily, PrEP 2-1-1, and PEP as preventative treatment regimens at baseline and follow-up. An additional open-ended question asked participants to explain their preferences.
Medication Adherence
Youth reported if they were currently taking PrEP, their adherence in the last 7 days (number of days taken dose in the last 7 days), and if they had ever taken PrEP 2-1-1 (yes/no).
Acceptability of the Adapted Active Visualization (Post-demonstration Only)
Immediately after the demonstration, youth reported how interesting and helpful the demonstration was for understanding PrEP, how motivated they felt to take PrEP, and how much anxiety they felt on a 10-point-Likert-type scale [ranging from 0 (minimum) to 10 (maximum)] [18].
Analysis
Demographic characteristics were compared between study arms using t tests (for continuous variables) and chi-squares (for categorical). Knowledge and perceptions scores were compared across study arms and timepoints using 2 × 2 ANOVAs. Descriptive statistics were summarized for PrEP preferences and uptake as low frequencies limited the appropriateness of statistical tests.
Results
Youth were on average 23 years old (SD = 2.3) and the majority were male (90%), and Latinx (51%). Most participants self-identified as gay (60%) and the remaining self-identified as bisexual (12%), queer (10%), pansexual (6%), heterosexual (4%), asexual (1%), unsure (1%), same gender loving (1%), or other (5%). Similar numbers of youth were either unemployed (30%), employed full time (26%), employed part time (23%), or in school (22%). There were no differences in demographics between study arms.
Intervention
Youth reported that the demonstration was helpful in understanding PrEP (M = 9.39, SD = 1.25) and interesting (M = 8.55, SD = 1.77). They also reported that the active visualization was motivating (M = 7.49, SD = 2.83). Youth reported feeling low anxiety after the demonstration (M = 1.59, SD = 2.85).
Knowledge of PrEP
Knowledge scores were higher at follow-up for both the intervention groups (Baseline: Mean = 5.1, SD = 1.3; Follow-up: Mean = 6.2, SD = 1.1) and SC (Baseline: Mean = 5.2, SD = 1.6; Follow-up: Mean = 5.8, SD = 1.5), F(94,1) = 45.6, p < 0.001, partial eta squared = 0.327). The interaction between the intervention groups and time was not statistically significant, F(94,1) = 3.66, p = 0.059, partial eta squared = 0.037). When considering just the questions regarding PrEP 2-1-1, intervention participants answered more items correctly at follow-up (M = 1.65, SD = 0.48) from baseline (M = 1.10, SD = 0.45) when compared to SC (baseline: M = 1.16, SD = 0.53, follow-up: M = 1.34, SD = 0.53), F(94,1) = 10.09, p = 0.002, partial eta squared = 0.097).
Perceptions of HIV and PrEP
Youth had similar illness perceptions about HIV and PrEP across measures and time-points. However, intervention youth felt that it was less difficult to take PrEP at follow-up when compared to baseline than standard care, F(1,94) = 5.13, p = 0.026, partial η2 = 0.052.
Preferences
PrEP regimen preferences in the intervention group were descriptively similar at baseline and follow-up. Low frequencies (< 5) in at least one group per comparison (see Table 1) prevented testing this statistically. At baseline and follow-up, most participants (82.9%, n = 121/146; 69.4%, n = 59/85) endorsed daily PrEP as their preferred method of prophylaxis, citing familiarity with this regimen as the reason for their preference. Fewer participants selected PrEP 2-1-1 as their preferred method at baseline (12.3%, n = 18/146) and follow-up (9.4%, n = 8/68). The main reason for preferring PrEP 2-1-1 was not wanting to take a daily medication. PEP was the least preferred method at both baseline (4.8%, n = 7/146) and follow-up (2.4%, n = 2/85). Overall, fewer participants reported having little or no knowledge of PrEP at follow-up (6.7%, n = 4/59) when compared to baseline (14.9%, n = 18/121).
PrEP Uptake/Adherence
At baseline, 14% (20/145) of all participants reported taking PrEP and most reported taking PrEP at least five times in the past week (14/20; 70%). Six participants (4%) reported ever taking PrEP 2-1-1 but only two reported taking it as prescribed. At 3-month follow-up, 16% (16/100) of all participants reported taking PrEP. Of those, eight reported taking PrEP at least five times during the last week at both baseline and follow-up. Regarding uptake, three participants (3%) reported starting PrEP at follow-up and all three reported adhering to PrEP in the previous week. All three of these participants were in the intervention group. Rates of adherence and uptake were too low to understand differences between groups. No participants reported taking PrEP 2-1-1 at follow-up.
Discussion
The current study examined whether providing youth at high risk for HIV with a 10-min, one-on-one, active visualization delivered online would impact PrEP adherence, knowledge, and preferences. Participants found the demonstration interesting, motivating, and helpful in understanding how PrEP works. Participants who viewed the active visualization also reported that PrEP was less difficult to take and knowledge specifically about PrEP 2-1-1 also significantly increased at follow-up. The intervention, however, did not, increase adherence or uptake in comparison to standard care. This suggests the demonstration had limited effectiveness in changing behavior.
Overall, participants in both the intervention and standard care groups had higher knowledge scores at follow-up when compared to baseline. This increase in knowledge across groups could be due to a high standard of care. Knowledge about how PrEP works increased among participants in the intervention group but this was specifically in relation to PrEP 2-1-1. This is consistent with previous research suggesting that visualization can improve knowledge of illness and treatments, including knowledge of HIV medication [8]. There is also evidence that interest in using PrEP increases with better understanding of the medication, suggesting that providing information may facilitate motivation to adhere to PrEP [23].
Overall, there is limited evidence that the demonstration was associated with any changes in preferences. Across assessments and groups, most participants preferred taking PrEP daily, and generally reported feeling most familiar with the ease/security of this method. This is consistent with previous research where youth prefer daily PrEP and perceive this regimen as effective [25].
The intervention did not improve uptake or adherence to PrEP although the number of patients taking PrEP in the current sample was low (about 15% at baseline and follow-up). Most participants in the sample who were taking PrEP reported strong adherence at both baseline and follow-up. Notably, the three participants reporting uptake of PrEP at follow-up were all in the intervention condition. The limited numbers of participants taking PrEP within the current sample and the good adherence demonstrated at baseline in both groups may have limited the potential impact of the active visualization upon adherence and uptake. It may be that this type of active visualization is more effective for people who are identified as non-adherent to their medication as was demonstrated in the previous ART active visualization trial [18]. Further, the COVID-19 lockdown could also have created barriers to accessing PrEP or may have reduced social interactions therefore limiting the need for PrEP. Moreover, conducting the demonstration online removed the ability for the participant to interact with the active visualization demonstration. This may have reduced the efficacy of the intervention to change participants’ knowledge and adherence.
Previous studies have found that internet-delivered interventions can increase knowledge and adherence/uptake of HIV medication [24]. However, for many of these studies, changes in outcomes were not sustained at follow-up [24], suggesting the potency of such interventions to change behavior may be limited. Furthermore, many internet-based HIV interventions that have impacted participant outcomes, have utilized multimedia platforms (such as websites, text message reminders, and social media) specifically created for online-delivery, rather than needing to transition from in-person to online [24]. Thus, internet interventions may be a viable and effective way to reach and educate at-risk youth about HIV prevention however, these interventions may be more effective if specifically tailored for online-delivery to enhance interactive learning.
The current results suggest that there is some evidence that PrEP 2-1-1 may be preferred among youth who do not want or need to take PrEP daily. The current study suggests that active visualization may be particularly useful in educating at-risk youth about PrEP 2-1-1. Increasing knowledge about PrEP is important as evidence suggests that adolescents, while more likely to have more partners, are less likely to have knowledge around PrEP as compared to adults [25]. The rising HIV infections among youth [3], demonstrate the importance of increasing knowledge about PrEP to prevent new infections.
The current study demonstrates how active visualization can be used to educate at-risk youth about PrEP medication regimens. Although the current pilot did not find changes in adherence or uptake, this model may have utility as an educational tool to increase knowledge about PrEP, and in-particular the PrEP 2-1-1 regimen. Future research could investigate whether this intervention is more effective in youths who are struggling to adhere to PrEP. Future applications may also include specifically tailoring the active visualization for online delivery, such as utilizing a multi-media platform to enhance interactivity for the user.
Data Availability
Due the sensitive information collected from youth at-risk for HIV, data is available upon request from Scott Hines, Director of Academic Technology, Palo Alto University, shines@paloaltou.edu.
Code Availability
N/A.
References
Eakle R, Venter F, Rees H. Pre-exposure prophylaxis (PrEP) in an era of state prevention: can it change the game? Retrovirology. 2018;15(29):1–10.
Mullins KLT, Lehmann EC. Oral PRe-exposure prophylaxis (PrEP) for HIV prevention in adolescents and young adults. Curr Pediatr Rep. 2018;6(2):114–22.
Wood S, Gross R, Shea AJ, Bauermeister AJ, Franklin J, Petsis D, et al. Barriers and facilitators of PrEP adherence for young men and transgender women of color. AIDS Behav. 2019;23(10):2719–29.
Hightow-Weidman BL, Muessig K, Rosenberg E, Sanchez T, LeGrand S, Gravens L, et al. University of North Carolina/Emory Center for Innovative Technology (iTech) for addressing the HIV epidemic among adolescents and young adults in the United States: protocol and rationale for center development. KMIR Red PRotoc. 2018;7(8): e10365.
Allan-Blitz L, Mena AL, Mayer HK. The ongoing HIV epidemic in American youth: challenges and opportunities. mHealth. 2021;7:33.
CDC. HIV in the United States: at a glance [Internet]. Center for Disease Control: CDC; 2021 [cited 2022 July 7]. Available from: https://www.cdc.gov/hiv/statistics/overview/ataglance.html.
Pérez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP uptake among racially/ethnically diverse young men who have sex with men: the P18 study. AIDS Educ Prev. 2015;27(2):112.
Hart-Cooper DG, Allen I, Irwin EC, Scott H. Adolescent health providers’ willingness to prescribe pre-exposure prophylaxis (PrEP) to youth at risk for HIV infection in the United States. J Adolesc Health. 2018;63(2):242–4.
Pleuhs B, Wuinn GK, Walsh LJ, Petroll EA, John AS. Health care provider barriers to HIV pre-exposure prophylaxis in the United States: a systematic review. AIDS Patient Care STDs. 2020;34(3):111–23.
Fisher BC, Fried LA, Desmond M, Macapagal K, Mustanski B. Perceived barriers to HIV prevention services for transgender youth. LGBT Health. 2018;5(6):350–8.
Songtaweesin NW, Kawichai S, Phanuphak N, Cressey RT, Wongharn P, Saisaengjan C, et al. Youth-friendly services and a mobile phone application to promote adherence to pre-exposure prophylaxis among adolescent men who have sex with men and transgender women at-risk for HIV in Thailand: a randomized control trial. J Int AIDS Soc. 2020;23(5): e25564.
Shams L, Seitz AR. Benefits of multisensory learning. Trends Cogn Sci. 2008;12(11):411–7.
Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211(4481):453–8.
Jones AS, Petrie KJ. I can see clearly now: using active visualization to improve adherence to ART and PrEP. AIDS Behav. 2017;21(2):335–40.
Brotherstone H, Miles A, Robb KA, Atkin W, Wardle J. The impact of illustrations on public understanding of the aim of cancer screening. Patient Educ Couns. 2006;63(3):328–35.
Harrow A, Wells M, Humphris G, Taylor C, Williams B. “Seeing is believing, and believing is seeing”: an exploration of the meaning and impact of women’s mental images of their breast cancer and their potential origins. Patient Educ Couns. 2008;73(2):339–46.
Jones AS, Ellis CJ, Nash M, Stanfield B, Broadbent E. Using animation to improve recovery from acute coronary syndrome: a randomized trial. Ann Behav Med. 2016;50(1):108–18.
Jones ASK, Coetzee B, Kagee A, Fernandez J, Cleveland E, Thomas M, Petrie KJ. The use of a brief, active visualisation intervention to improve adherence to antiretroviral therapy in non-adherent patients in South Africa. AIDS Behav. 2019;23(8):2121–9.
Christodoulou J, Abdalian SE, Jones AS, Christodoulou G, Pentoney SL, Rotheram-Borus MJ. Crystal clear with active visualization: understanding medication adherence among youth living with HIV. AIDS Behav. 2020;24(4):1207–11.
Swendeman D, Arnold EM, Harris D, Fournier J, Comulada WS, Reback C, et al. Text-messaging, online peer support group, and coaching strategies to optimize the HIV prevention continuum for youth: protocol for a randomized controlled trial. JMIR Res Protoc. 2019;8(8): e11165.
Molina JM, Capitant C, Spire B, Pialoux G, Cotte L, Charreau I, Tremblay C, Le Gall JM, Cua E, Pasquet A, Raffi F, Group AIS. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373(23):2237–46.
Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7.
Koechlin MF, Fonner AV, Dalglish LA, O’Reilly RK, Baggaley R, Grant MR, Rodolph M, Hodges-Mameletzis I, Kennedy EC. Values and preferences in the use of oral pre-exposure prophylaxis (PrEP) for HIV prevention among multiple populations: a systematic review of the literature. AIDS Behav. 2017;21:1325–35.
Nguyen LH, Tran BX, Rocha LEC, Nguyen HLT, Yang C, Latkin CA, Thorson A, Stromdahl S. A systematic review of eHealth Intervention addressing HIV/STI prevention among men who have sex with men. AIDS Behav. 2019;23:2253–72.
Macapagal K, Kraus A, Korpak KA, Jozsa K, Moskowirz AD. PrEP awareness, uptake, barriers, and correlates among adolescents assigned male at birth who have sex with males in the U.S. Arch Sex Behav. 2020;49:113–24.
Funding
Funding was provided by UCLA Center for HIV Identification, Prevention and Treatment Services and National Institute of Mental Health (Grant No: T32MH109205).
Author information
Authors and Affiliations
Contributions
JC was involved in the conception of the study, securing funding, overseeing the intervention, data collection, and analyses, and drafted the first complete draft of the manuscript. EV and ES conducted the analyses and assisted in drafting the paper. AJ and MJRB were involved with the conception of the study and in editing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest or competing interests.
Consent to Participate
Youth provided voluntary and informed consent via zoom and using Qualtrics, survey analytic platform.
Consent for Publication
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Christodoulou, J., Vincent, E., Shaw, E. et al. Not as Clear Online? Active Visualization of How PrEP Works in the Body Improves Knowledge But Doesn’t Change Behavior. AIDS Behav 27, 1116–1122 (2023). https://doi.org/10.1007/s10461-022-03848-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03848-6