Abstract
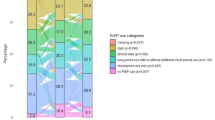
We assessed the coverage of sex acts by event-driven pre-exposure prophylaxis (ED-PrEP) over a 2-month period in 54 participants in the open label phase of the ANRS Ipergay trial. Participants received an electronic monitoring system device to record bottle openings. Self-questionnaires collected daily information on PrEP intake and sexual behavior. Intake was also estimated through returned pill counts. Full coverage of sex acts was defined as at least one pill taken both within 24 h before and within 48 h following sex. There was a strong correlation (r = − 0.92) between the number of bottle openings and returned pill counts. During the study, 42 participants (78%) practiced ED-PrEP and 12 (22%) daily PrEP with bottle openings at least 5 days/week whatever their sexual activity. Out of the 154 reported receptive anal sex acts, 81% were condomless: among them, PrEP coverage was hight: 97% among those practicing daily PrEP and 82% among those using ED-PrEP.



Similar content being viewed by others
References
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Thigpen M, Kebaabetswe P, Smith D, Segolodi T, Soud F, Chillag K, et al. Daily oral antiretroviral use for the prevention of HIV infection in heterosexually active young adults in Botswana: results from the TDF2 study. In. 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention; 2011.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387(10013):53–60.
Molina JM, Capitant C, Spire B, Pialoux G, Cotte L, Charreau I, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373(23):2237–46.
Lundgren JD, Battegay M, Behren G, De Wit S, Guaraldi G, Katlama C, et al. European AIDS Clinical Society (EACS) guidelines on the prevention and management of metabolic diseases in HIV. Hiv Medicine. 2008;9(2):72–81.
WHO. What’s the 2+1+1? Event-driven oral pre-exposure prophylaxis to prevent HIV for men who have sex with men: Update to WHO’s recommendation on oral PrEP. In; July 2019.
Garcia-Lerma JG, Otten RA, Qari SH, Jackson E, Cong ME, Masciotra S, et al. Prevention of rectal SHIV transmission in macaques by daily or intermittent prophylaxis with emtricitabine and tenofovir. PLoS Med. 2008;5(2):291–9.
Cottrell ML, Yang KH, Prince HMA, Sykes C, White N, Malone S, et al. Predicting effective truvada (R) PrEP dosing strategies with a novel PK-PD model incorporating tissue active metabolites and endogenous nucleotides (EN). AIDS Res Hum Retroviruses. 2014;30:A60–A6060.
Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Inf Dis. 2014;14(9):820–9.
Bekker LG, Roux S, Sebastien E, Yola N, Amico KR, Hughes JP, et al. Daily and non-daily pre-exposure prophylaxis in African women (HPTN 067/ADAPT Cape Town Trial): a randomised, open-label, phase 2 trial. Lancet HIV. 2018;5(2):E68–E78.
Mugo PM, Sanders EJ, Mutua G, van der Elst E, Anzala O, Barin B, et al. Understanding adherence to daily and intermittent regimens of oral HIV pre-exposure prophylaxis among men who have sex with men in Kenya. AIDS Behav. 2015;19(5):794–801.
Grant RM, Mannheimer S, Hughes JP, Hirsch-Moverman Y, Loquere A, Chitwarakorn A, et al. Daily and nondaily oral preexposure prophylaxis in men and transgender women who have sex with men: the human immunodeficiency virus prevention trials network 067/ADAPT study. Clin Infect Dis. 2018;66(11):1712–21.
Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. Obstet Gynecol Surv. 2015;70(7):444–6.
Garcia-Lerma JG, Cong ME, Mitchell J, Youngpairoj AS, Zheng Q, Masciotra S, et al. Intermittent prophylaxis with oral truvada protects macaques from rectal SHIV infection. Sci Transl Med. 2010;2(14):14ra14.
Fonsart J, Saragosti S, Taouk M, Peytavin G, Bushman L, Charreau I, et al. Single-dose pharmacokinetics and pharmacodynamics of oral tenofovir and emtricitabine in blood, saliva and rectal tissue: a sub-study of the ANRS IPERGAY trial. J Antimicrob Chemother. 2017;72(2):478–85.
AARDEX Group, Ltd, Sion, Switzerland. MEMs software: https://www.aardexgroup.com. In.
Hendrix CW, Andrade A, Bumpus NN, Kashuba AD, Marzinke MA, Moore A, et al. Dose frequency ranging pharmacokinetic study of tenofovir-emtricitabine after directly observed dosing in healthy volunteers to establish adherence benchmarks (HPTN 066). AIDS Res Hum Retroviruses. 2016;32(1):32–433.
Donnell D, Baeten JM, Bumpus NN, Brantley J, Bangsberg DR, Haberer JE, et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. JAIDS J Acquir Immun Def Syndr. 2014;66(3):340–8.
Blum MR, Chittick GE, Begley JA, Zong J. Steady-state pharmacokinetics of emtricitabine and tenofovir disoproxil fumarate administered alone and in combination in healthy volunteers. J Clin Pharmacol. 2007;47(6):751–9.
Team RC. R: A language and environment for statistical computing. In. 3.2.3 ed; 2015.
Di Ciaccio M, Fressard L, Sagaon-Teyssier L, Protiere C, Gatey C, Chas J, Cotte L, Castro DR, Meyer L, Molina JM, Préau M, Spire B. What are the situational and behavioral factors associated with condomless anal sex without PrEP in men who have sex with men? Results from the ANRS-IPERGAY trial. AIDS. 2020. https://doi.org/10.1097/QAD.0000000000002542.
Molina J, Prevenir ANRS Study G. Incidence of HIV-infection with daily or on-demand PrEP with TDF/FTC in Paris area. Update from the ANRS Prevenir Study. In; 2019 (IAS Mexico).
Mutua G, Sanders E, Mugo P, Anzala O, Haberer JE, Bangsberg D, et al. Safety and adherence to intermittent pre-exposure prophylaxis (PrEP) for HIV-1 in African men who have sex with men and female sex workers. PLoS One. 2012;7(4):e33103.
Vuylsteke B, Reyniers T, De Baetselier I, Nostlinger C, Crucitti T, Buyze J, et al. Daily and event-driven pre-exposure prophylaxis for men who have sex with men in Belgium: results of a prospective cohort measuring adherence, sexual behaviour and STI incidence. J Int AIDS Soc. 2019;22(10):e25407.
Noret M, Balavoine S, Pintado C, Siguier M, Brun A, Bauer R, et al. Daily or on-demand oral tenofovir disoproxil fumarate/emtricitabine for HIV pre-exposure prophylaxis: experience from a hospital-based clinic in France. AIDS. 2018;32(15):2161–9.
Acknowledgments
We thanks the study participants for their time and dedication to this study, the National Agency for Research on AIDS and Hepatitis (ANRS; France Recherche Nord & Sud Sida-HIV Hépatites) and its Director François Dabis, the Canadian HIV Trials Network, Fondation Pierre Bergé pour la prevention/Sidaction, and the Bill & Melinda Gates Foundation for their grant support, Gilead Sciences for donation of tenofovir disoproxil fumarate and emtricitabine, and Jean-François Delfraissy for his support from the beginning of the trial. We thank the gay communities in France and Canada (AIDES, COQSIDA, REZO) who supported this work.
Funding
The funding was provided by Institut National de la Santé et de la Recherche Médicale [Grant No. N14036LR].
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bauer, R., Netzer, E., Pintado, C. et al. Coverage of Sex Acts by Event-Driven Pre-exposure Prophylaxis: A Sub-Study of the ANRS IPERGAY Trial. AIDS Behav 24, 3244–3251 (2020). https://doi.org/10.1007/s10461-020-02890-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-02890-6