Abstract
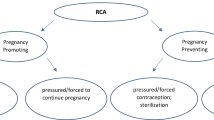
To better understand the structural drivers of women living with HIV’s (WLWH’s) reproductive rights and choices, this study examined the structural correlates, including non-consensual HIV disclosure, on WLWH’s pregnancy decisions and describes access to preconception care. Analyses drew on data (2014-present) from SHAWNA, a longitudinal community-based cohort with WLWH across Metro-Vancouver, Canada. Multivariable logistic regression was used to model the effect of non-consensual HIV disclosure on WLWH’s pregnancy decisions. Of the 218 WLWH included in our analysis, 24.8% had ever felt discouraged from becoming pregnant and 11.5% reported accessing preconception counseling. In multivariable analyses, non-consensual HIV disclosure was positively associated with feeling discouraged from wanting to become pregnant (AOR 3.76; 95% CI 1.82–7.80). Non-consensual HIV disclosure adversely affects WLWH’s pregnancy decisions. Supporting the reproductive rights of WLWH will require further training among general practitioners on the reproductive health of WLWH and improved access to women-centred, trauma-informed care, including non-judgmental preconception counseling.

Similar content being viewed by others
References
Antiretroviral Therapy Cohort C. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372(9635):293–9.
Hogg RS, Heath KV, Yip B, Craib KJ, O’Shaughnessy MV, Schechter MT, et al. Improved survival among HIV-infected individuals following initiation of antiretroviral therapy. JAMA. 1998;279(6):450–4.
Jin Y, Liu Z, Wang X, Liu H, Ding G, Su Y, et al. A systematic review of cohort studies of the quality of life in HIV/AIDS patients after antiretroviral therapy. Int J STD AIDS. 2014;25(11):771–7.
Nosyk B, Zang X, Min JE, Krebs E, Lima VD, Milloy MJ, et al. Relative effects of antiretroviral therapy and harm reduction initiatives on HIV incidence in British Columbia, Canada, 1996-2013: a modelling study. Lancet HIV. 2017;4(7):e303–10.
Chi BH, Stringer JS, Moodley D. Antiretroviral drug regimens to prevent mother-to-child transmission of HIV: a review of scientific, program, and policy advances for sub-Saharan Africa. Curr HIV/AIDS Rep. 2013;10(2):124–33.
Nattabi B, Li J, Thompson SC, Orach CG, Earnest J. A systematic review of factors influencing fertility desires and intentions among people living with HIV/AIDS: implications for policy and service delivery. AIDS Behav. 2009;13(5):949–68.
Sharma A, Feldman JG, Golub ET, Schmidt J, Silver S, Robison E, et al. Live birth patterns among human immunodeficiency virus-infected women before and after the availability of highly active antiretroviral therapy. Am J Obstet Gynecol. 2007;196(6):541.e1-6.
Haddad LB, Machen LK, Cordes S, Huylebroeck B, Delaney A, Ofotokun I, et al. Future desire for children among women living with HIV in Atlanta, Georgia. AIDS Care. 2016;28(4):455–9.
Jones DL, Cook R, Potter JE, Miron-Shatz T, Chakhtoura N, Spence A, et al. Fertility desires among women living with HIV. PLoS ONE. 2016;11(9):e0160190.
Jose H, Madi D, Chowta N, Ramapuram J, Bhaskaran U, Achappa B, et al. Fertility desires and intentions among people living with HIV/AIDS (PLWHA) in Southern India. J Clin Diagn Res. 2016;10(6):Oc19–22.
Loutfy MR, Hart TA, Mohammed SS, Su D, Ralph ED, Walmsley SL, et al. Fertility desires and intentions of HIV-positive women of reproductive age in Ontario, Canada: a cross-sectional study. PLoS ONE. 2009;4(12):e7925.
Finocchario-kessler S, Sweat MD, Keller JM, Anderson JR, Finocchario-Kessler S, Sweat MD, et al. Understanding high fertility desires and intentions among a sample of urban women living with HIV in the United States. AIDS Behav. 2010;14(5):1106–14.
Health Canada. HIV and AIDS in Canada: surveillance report to June 30, 2002. Ottawa: Division of HIV/AIDS Epidemiology and Surveillance, Centre for Infectious Disease Prevention and Control (CIDPC), Health Canada; 2002.
Ogilvie GS, Palepu A, Remple VP, Maan E, Heath K, MacDonald G, et al. Fertility intentions of women of reproductive age living with HIV in British Columbia, Canada. AIDS. 2007;21(Suppl 1):S83–8.
Fabiani M, Nattabi B, Ayella EO, Ogwang M, Declich S. Differences in fertility by HIV serostatus and adjusted HIV prevalence data from an antenatal clinic in northern Uganda. Trop Med Int Health. 2006;11(2):182–7.
Burgess A, Purssell E. What is the relationship between increased access to HAART, relationship status and fertility decisions amongst HIV positive women? A literature review and meta-analysis. J Clin Nurs. 2017.
Demissie DB, Tebeje B, Tesfaye T. Fertility desire and associated factors among people living with HIV attending antiretroviral therapy clinic in Ethiopia. BMC Pregnancy Childbirth. 2014;14:382.
Public Health Agency of Canada. HIV and AIDS in Canada: surveillance report to December 31, 2013. Ottawa: Public Health Agency of Canada; 2014.
Donnelly LR, Bailey L, Jessani A, Postnikoff J, Kerston P, Brondani M. Stigma experiences in marginalized people living with HIV seeking health services and resources in Canada. J Assoc Nurses AIDS Care. 2016;27(6):768–83.
Benoit C, Carroll D, Chaudhry M. In search of a healing place: aboriginal women in Vancouver’s downtown eastside. Soc Sci Med. 2003;56:821–33.
Oosterhoff P, Anh NT, Hanh NT, Yen PN, Wright P, Hardon A. Holding the line: family responses to pregnancy and the desire for a child in the context of HIV in Vietnam. Cult Health Sex. 2008;10(4):403–16.
Cooper D, Harries J, Myer L, Orner P, Bracken H, Zweigenthal V. “Life is still going on”: reproductive intentions among HIV-positive women and men in South Africa. Soc Sci Med. 2007;65(2):274–83.
Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. AIDS Behav. 2013;17(7):2528–39.
Duff P, Kipp W, Wild TCC, Rubaale T, Okech-Ojony J. Barriers to accessing highly active antiretroviral therapy by HIV-positive women attending an antenatal clinic in a regional hospital in western Uganda. J Int AIDS Soc. 2010;13(1):37.
Greene S, Ion A, Kwaramba G, Smith S, Loutfy MR. “Why are you pregnant? What were you thinking?”: how women navigate experiences of HIV-related stigma in medical settings during pregnancy and birth. Soc Work Health Care. 2016;55(2):161–79.
Ion A, Elston D. Examining the health care experiences of women living with human immunodeficiency virus (HIV) and perceived HIV-related stigma. Womens Health Issues. 2015;25(4):410–9.
Craft SM, Delaney RO, Bautista DT, Serovich JM. Pregnancy decisions among women with HIV. AIDS Behav. 2007;11(6):927–35.
Darlington CK, Hutson SP. Understanding HIV-related stigma among women in the Southern United States: a literature review. AIDS Behav. 2017;21(1):12–26.
Bernard E, Bennet-Carlson R. Criminalization of HIV non-disclosure, exposure and transmission: background and current landscape. Geneva: UNAIDS; 2012.
Patterson SE, Milloy MJ, Ogilvie G, Greene S, Nicholson V, Vonn M, et al. The impact of criminalization of HIV non-disclosure on the healthcare engagement of women living with HIV in Canada: a comprehensive review of the evidence. J Int AIDS Soc. 2015;18:20572.
Brezing C, Ferrara M, Freudenreich O. The syndemic illness of HIV and trauma: implications for a trauma-informed model of care. Psychosomatics. 2015;56(2):107–18.
Duff PK, Money DM, Ogilvie GS, Ranville F, Kestler M, Braschel MC, et al. Severe menopausal symptoms associated with reduced adherence to antiretroviral therapy among perimenopausal and menopausal women living with HIV in metro Vancouver. Menopause (New York, NY); 2017.
Ratzlaff A, Deering K, Pick N, Kestler M, Ranville F, Braschel M, et al., editors. Women living with HIV identify critical need for trauma-informed HIV Care models to support ART use in Metro Vancouver, Canada. Canadian Association for HIV Research; 2017; Vancouver.
Gelaye B, Zhong QY, Basu A, Levey EJ, Rondon MB, Sanchez S, et al. Trauma and traumatic stress in a sample of pregnant women. Psychiatry Res. 2017;257:506–13.
Torchalla I, Linden IA, Strehlau V, Neilson EK, Krausz M. “Like a lots happened with my whole childhood”: violence, trauma, and addiction in pregnant and postpartum women from Vancouver’s Downtown Eastside. Harm Reduct J. 2015;11:34.
SAMHSA’s Traumatic and Justice Strategic Initiative. SAMHSA’s concept of trauma and guidance for a trauma-informed approach; 2014.
Canada PHAo. HIV and AIDS in Canada: Surveillance Report to December 31, 2013.. Ottawa, Canada: Minister of Public Works and Government Services Canada.; 2014.
Barreto D, Krusi A, Ranville F, Safford H, Pooyak S, Braschel M, et al. HIV disclosure without consent linked to increased risk of violence against women living with HIV in Metro Vancouver, British Columbia. Women and HIV workshop, February 2017, Seattle, USA; 2017.
Ross L. What is Reproductive Justice?: Sistersong Women on Color Reproductive Health Collective and Pro-Choice Public Education Project; 2007.
Wood E, Tyndall MW, Spittal PM, Li K, Anis AH, Hogg RS, et al. Impact of supply-side policies for control of illicit drugs in the face of the AIDS and overdose epidemics: investigation of a massive heroin seizure. CMAJ. 2003;168(2):165–9.
Stockman JK, Morris MD, Martinez G, Lozada R, Patterson TL, Ulibarri MD, et al. Prevalence and correlates of female condom use and interest among injection drug-using female sex workers in two mexico-us border cities. AIDS Behav. 2012;16(7):1877–86.
Lima VD, Harrigan R, Fau-Murray M, Murray M, Fau-Moore DM, Moore DM, Fau-Wood E, Wood E, Fau-Hogg RS, Hogg RS, Fau-Montaner JS, et al. Differential impact of adherence on long-term treatment response among naive HIV-infected individuals, p. 1473–5571. (Electronic).
Prudden H, Dzialowy N, Foss A, Black V, Wallace C, Nyblade L. Modelling the impact of stigma on the Prevention of Mother to Child HIV Transmission for a setting in South Africa. Technical Report: London School of Hygiene and Tropical Medicine; 2011.
Rujumba J, Neema S, Byamugisha R, Tylleskar T, Tumwine JK, Heggenhougen HK. “Telling my husband I have HIV is too heavy to come out of my mouth”: pregnant women’s disclosure experiences and support needs following antenatal HIV testing in eastern Uganda. J Int AIDS Soc. 2012;15(2):17429.
Kendall T. Reproductive rights violations reported by Mexican women with HIV. Health Hum Rights. 2009;11(2):77–87.
Ion A, Wagner AC, Greene S, Loutfy MR. HIV-related stigma in pregnancy and early postpartum of mothers living with HIV in Ontario, Canada. AIDS Care. 2017;29(2):137–44.
Logie C, James L, Tharao W, Loutfy M. Associations between HIV-related stigma, racial discrimination, gender discrimination, and depression among HIV-positive African, Caribbean, and Black Women in Ontario, Canada. AIDS Patient Care STDs. 2013;27(2):114–22.
Loutfy MR, Blitz S, Zhang Y, Hart TA, Walmsley SL, Smaill FM, et al. Self-reported preconception care of HIV-positive women of reproductive potential: a retrospective study. J Int Assoc Provid AIDS Care. 2014;13(5):424–33.
Finocchario-Kessler S, Dariotis JK, Sweat MD, Trent ME, Keller JM, Hafeez Q, et al. Do HIV-infected women want to discuss reproductive plans with providers, and are those conversations occurring? AIDS Patient Care STDS. 2010;24(5):317–23.
Hoyt MJ, Storm DS, Aaron E, Anderson J. Preconception and contraceptive care for women living with HIV. Infect Dis Obstet Gynecol. 2012;2012:604183.
Coll AS, Potter JE, Chakhtoura N, Alcaide ML, Cook R, Jones DL. Providers’ perspectives on preconception counseling and safer conception for HIV-infected women. AIDS Care. 2016;28(4):513–8.
World Health Organization. Consolidated guidelines on sexual and reproductive health and rights of women living with HIV; 2017.
Of BWsHHCaBCC, Excellence for Women’s Health. A women’s health strategy for British Columbia: advancing the health of girls and women. Vancouver: BC Women’s Hospital & Health Centre and British Columbia Centre of Excellence for Women’s Health; 2004.
Loutfy MR, Margolese S, Money DM, Gysler M, Hamilton S, Yudin MH. Canadian HIV pregnancy planning guidelines: no. 278, June 2012. Int J Gynaecol Obstet. 2012;119(1):89–99.
Acknowledgments
We thank all those who contributed their time and expertise to this project, particularly participants, community partners, the SHAWNA Positive Women’s Advisory Board and Community Advisory Board, and the SHAWNA Project team: Sarah Moreheart, Brittany Udall, Jennifer Morris, Flo Ranville, Heidi Safford, Lauren Martin, Ray Croy, Bridgette Simpson, Anita Dhanoa, Monique Desroches, Lydia Hamel, Lulu Gurney, and Patience Chamboko. We also acknowledge Melissa Braschel, Abby Rolston, Sylvia Machat, Peter Vann, Erin Seatter, and Patricia McDonald for their research and administrative support. KS is supported by a Canada Research Chair in Global Sexual Health and HIV/AIDS and Michael Smith Foundation for Health Research. KS is supported by a Canada Research Chair in Global Sexual Health and HIV/AIDS and Michael Smith Foundation for Health Research. PD is supported by the Canadian Institutes for Health Research and Michael Smith Foundations for Health Research Postdoctoral Fellowship Award. JM received research support, paid to the institution, from the Public Health Agency of Canada, the BC-Ministry of Health, the US NIH (NIDA R01DA036307 and CTN 248), the Canadian Institutes of Health Research, Janssen & Janssen, and Merk.
Funding
This research was supported by the Canadian Institutes of Health Research (MOP-133617) and MacAIDS.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Research Involving Human Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study holds ethical approval through Providence Health Care/University of British Columbia Research Ethics Board and BC Women’s Hospital.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Duff, P., Kestler, M., Chamboko, P. et al. Realizing Women Living with HIV’s Reproductive Rights in the Era of ART: The Negative Impact of Non-consensual HIV Disclosure on Pregnancy Decisions Amongst Women Living with HIV in a Canadian Setting. AIDS Behav 22, 2906–2915 (2018). https://doi.org/10.1007/s10461-018-2111-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2111-8