Abstract
Purpose
This study utilized translabial three-dimensional ultrasound to investigate the morphological characteristics of the levator hiatus and provide sonographic evidence for assessing pelvic floor dysfunction in postpartum women.
Methods
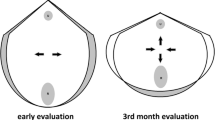
Two-hundred and one singleton primiparae without any complications underwent translabial three-dimensional ultrasound at 6 and 18 weeks after delivery, with 12 participants lost to follow-up at 18 weeks. Fifty nulliparae were enrolled as the control group. Levator hiatal morphology at rest and on Valsalva maneuver was assessed by experienced sonographers, specifically evaluating the anteroposterior diameter, left-to-right diameter, and area.
Results
In postpartum women at 6 weeks after delivery, all the levator hiatal parameters were significantly higher compared with those of the control group. At 18 weeks, the hiatal parameters were better than at 6 weeks but still higher than in the nulliparous controls. In all three groups, the hiatal parameters were significantly higher during the Valsalva maneuver than at rest.
Conclusions
Postpartum women are prone to develop pelvic floor dysfunction as shown by an enlarged levator hiatus. Translabial three-dimensional ultrasound can be used to effectively assess the morphology and structural alterations of the levator hiatus in postpartum women, providing reliable pelvic floor imaging for early screening, diagnosis, and prevention of pelvic floor dysfunction.




Similar content being viewed by others
References
Sung VW, Hampton BS. Epidemiology of pelvic floor dysfunction. Obstet Gynecol Clin N Am. 2009;36:421–43.
Glazener C, Elders A, Macarthur C, et al. Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG. 2013;120:161–8.
Schwertner-Tiepelmann N, Thakar R, Sultan AH, et al. Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol. 2012;39:372–83.
Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106:707–12.
Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. BJOG. 2010;117:1485–92.
Pelsang RE, Bonney WW. Voiding cystourethrography in female stress incontinence. AJR Am J Roentgenol. 1996;166:561–5.
Tunn R, Schaer G, Peschers U, et al. Updated recommendations on ultrasonography in urogynecology. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:236–41.
Dietz HP. Female pelvic floor dysfunction—an imaging perspective. Nat Rev Gastroenterol Hepatol. 2012;9:113–21.
De Almeida FG, Rodriguez LV, Raz S. Magnetic resonance imaging in the diagnosis of pelvic floor disorders. Int Braz J Urol. 2002;28:553–9.
Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25:580–5.
Dietz HP. Pelvic floor ultrasound: a review. Am J Obstet Gynecol. 2010;202:321–34.
Falkert A, Willmann A, Endress E, et al. Three-dimensional ultrasound of pelvic floor: is there a correlation with delivery mode and persisting pelvic floor disorders 18–24 months after first delivery? Ultrasound Obstet Gynecol. 2013;41:204–9.
Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116:1281–7.
Svabik K, Shek K, Dietz H. How much does the levator hiatus have to stretch during childbirth? BJOG. 2009;116:1657–62.
DeLancey JO, Kearney R, Chou Q, et al. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101:46–53.
Fonti Y, Giordano R, Cacciatore A, et al. Post partum pelvic floor changes. J Prenat Med. 2009;3:57–9.
Wei JT, De Lancey JO. Functional anatomy of the pelvic floor and lower urinary tract. Clin Obstet Gynecol. 2004;47:3–17.
Dietz HP, Shek C, De Leon J, et al. Ballooning of the levator hiatus. Ultrasound Obstet Gynecol. 2008;31:676–80.
Dietz HP, Steensma AB. The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG. 2006;113:225–30.
Wieczorek AP, Wozniak MM, Stankiewicz A, et al. 3-D high-frequency endovaginal ultrasound of female urethral complex and assessment of inter-observer reliability. Eur J Radiol. 2012;81:e7–12.
Majida M, Brækken IH, Bø K, et al. Validation of three-dimensional perineal ultrasound and magnetic resonance imaging measurements of the pubovisceral muscle at rest. Ultrasound Obstet Gynecol. 2010;35:715–22.
Falkert A, Endress E, Weigl M, et al. Three-dimensional ultrasound of the pelvic floor 2 days after first delivery: influence of constitutional and obstetric factors. Ultrasound Obstet Gynecol. 2010;35:583–8.
Dietz HP, Moegni F, Shek KL. Diagnosis of levator avulsion injury: a comparison of three methods. Ultrasound Obstet Gynecol. 2012;40:693–8.
Rostaminia G, Manonai J, Leclaire E, et al. Interrater reliability of assessing levator ani deficiency with 360° 3D endovaginal ultrasound. Int Urogynecol J. 2014;25:761–6.
Acknowledgments
This study was supported by the Joint Key Project of New Frontier Technology in Shanghai Municipal Hospitals (No. SHDC12013120) and the Project of the Science and Technology Commission of Shanghai Municipality (No. 124119a5501).
Conflict of interest
All authors declare no conflict of interest.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
X.-M. Wang and X. Chang contributed equally to the work.
About this article
Cite this article
Wang, XM., Chang, X., Ding, Y. et al. Translabial three-dimensional ultrasound investigation of the levator hiatus in postpartum women. J Med Ultrasonics 42, 373–378 (2015). https://doi.org/10.1007/s10396-014-0609-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-014-0609-x