Summary
Background
Anastomotic leakage represents a devastating post-surgical event with surgeon- and patient-related causes. The early lag phase of healing (day 0–4) is a time of increased vulnerability. The current role of tissue sealants as anastomotic adjuncts remains unclear, with controversial results reported. Platelet-rich plasma provides a reliable source of growth factors supporting wound healing. We aimed to assess the impact of a novel autologous platelet-rich fibrin (PRF) agent (Obsidian-ASG® matrix; GergMed Medizintechnik, Baiern, Germany) on colonic anastomotic healing in a porcine model.
Methods
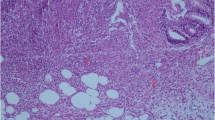
Left-sided colonic anastomoses were constructed in 16 pigs with reinforcement using the Obsidian-ASG® matrix in 12 animals. Animals were sacrificed on days 0, 4, 10 and 30, with histologic assessment of the anastomotic line along with evaluation of fibrotic tissue maturation, foreign body reactivity and mucin production. Collagen maturity and immunohistochemical changes of angiogenesis and infiltrating macrophage profiles were determined as well.
Results
There was no observable effect in matrix-treated animals on epithelial line thickness, granulation tissue formation, foreign body reactivity or mucosal restitution. Matrix-treated animals showed higher mucin production on day 4 accompanied by a more mature collagen and a greater degree of early angiogenic response with a higher infiltration density of M2 macrophages. Additionally, anastomotic burst pressure in matrix-treated animals was higher on day 0, 4, 10 and 30 (100, 100, 210, 160 vs. 40, 30, 60, 20 mm Hg, respectively).
Conclusion
Obsidian-ASG® matrix may have beneficial effects on anastomotic healing by shifting the inflammatory response towards a mature and more stable collagen phenotype in the early phase.





Similar content being viewed by others
References
Buchs NC, Gervaz P, Secic M, Mugnier-Konrad B, Morel P. Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis. 2008;23:265–70.
McDermott FD, Heeney A, Kelly ME, et al. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg. 2015;102:462–79.
Berho M, Wexner SD, Botero-Anug A‑M, Pelled D, Fleshman JW. Histopathologic advantages of compression ring anastomosis healing as compared with stapled anastomosis in a porcine model: a blinded comparative study. Dis Colon Rectum. 2014;57:506–13.
Pommergaard H‑C, Achiam MP, Rosenberg J. External coating of colonic anastomoses: a systematic review. Int J Colorectal Dis. 2012;27:1247–58.
Vakalopoulos KA, Daams F, Wu Z, et al. Tissue adhesives in gastrointestinal anastomosis: a systematic review. J Surg Res. 2013;180:290–300.
Stergios K, Kontzoglou K, Pergialiotis V, Korou LM, Frountzas M, Lalude O, Nikiteas N. The potential effect of biological sealants on colorectal anastomosis: healing in experimental research involving severe diabetes. Ann R Coll Surg Engl. 2017;99:189–92.
Vakalopulos KA, Wu Z, Kroese LF, Jeekel J, Kleinrinsenk G‑J, Dodou D, Lam KH, Lange JF. Sutureless closure of colonic defects with tissue adhesives: an in vivo study. Am J Surg. 2017;213:151–8.
Akgün A, Kuru S, Uraldi C, Tekin O, Karip B, Tug T, Ongoren AU. Early effects of fibrin sealant on colonic anastomosis in rats: an experimental and case-control study. Tech Coloproctol. 2006;10:208–14.
Giuratrabocchetta S, Rinaldi M, Cuccia F, Lemma M, Piscitelli D, Polidoro P, Altomare DF. Protection of intestinal anastomosis with biological glues: an experimental method. Tech Coloproctol. 2011;15:153–8.
Vakalopoulos KA, Wu Z, Kroese LF, van der Horst PH, Lam KH, Dodou D, Jeekel JJ, Lange JF. Clinical, mechanical, and immunohistopathological effects of tissue adhesives on the colon: an in‐vivo study. J Biomed Mater Res Part B Appl Biomater. 2017;105(4):846–54.
Nordentoft T. Sealing of gastrointestinal anastomoses with fibrin glue coated collagen patch. Dan Med J. 2015;62(5):B5081.
Huh JW, Kim HR, Kim YJ. Anastomotic leakage after laparoscopic resection of rectal cancer: the impact of fibrin glue. Am J Surg. 2010;199:435–41.
Spotnitz WD. Fibrin sealant: Past, present and future: a brief review. World J Surg. 2010;34:632–4.
Nanditha S, Chandrasekaran B, Muthusamy S, Muthu K. Apprising the diverse facets of platelet rich fibrin in surgery through a systematic review. Int J Surg. 2017;46:186–94.
Rughetti A, Giusti I, D’Ascenzo S, Leocata P, Carta G, Pavan A, Dell’Orso L, Dolo V. Platelet gel-released supernatant modulates the angiogenic capability of human endothelial cells. Blood Transfus. 2008;6:12–7.
Dohan Ehrenfest DM, de Peppo GM, Doglioli P, Sammartino G. Slow release of growth factors and thrombospondin-1 in Choukroun’s platelet-rich fibrin (PRF): a gold standard to achieve for all surgical platelet concentrates technologies. Growth Factors. 2009;27:63–9.
Bai MY, Wang CW, Wang JY, Lin MF, Chan WP. Three-dimensional structure and cytokine distribution of platelet-rich fibrin. Clinics (Sao Paulo). 2017;72:116–24.
Kjaergard HK, Fairbrother JE, Cederholm-Williams SA, Edwardson PAD, Hollingsbee DA, Holm NE. The Vivostat system for the automated preparation of autologous fibrin sealant. Cardiovasc Eng. 1997;2:204–6.
Velada JL, Hollingsbee DA, Menzies AR, Cornwell R, Dodd RA. Reproducibility of the mechanical properties of Vivostat patient-derived fibrin sealant. Biomaterials. 2002;23:2249–54.
Kilkenny C, Browne W, Cuthill IC, et al. Animal research: Reporting in vivo experiments: the ARRIVE guidelines. Br J Pharmacol. 2010;160:1577–9.
Dodd RA, Cornwell R, Holm NE, Garbasch A, Hollingsbee DA. The Vivostat application system: a comparison with conventional fibrin sealant systems. Technol Health Care. 2002;10(5):401–11.
Kjaergard HK, Velada JL, Pedesen JH, Fleron H, Hollingsbee DA. Comparative kinetics of polymerization of three sealants and influence on timing of tissue adhesion. Thromb Res. 2000;98:221–8.
Zuhlke HV, Lorenz EM, Straub EM, et al. Pathophysiology and classification of adhesions. Langenbecks Arch Chir Suppl Ii Verh Dtsch Ges Chir. 1990;345:1009–16.
Kopelman Y, Siersema PD, Nir Y, et al. Endoluminal compression clip: full-thickness resection of the mesenteric bowel wall in a porcine model. Gastrointest Endosc. 2009;70:1146–57.
Barros MH, Hauck F, Dreyer JH, Kempkes B, Niedobitek G. Macrophage polarization: an immunohistochemical approach for identifying M1 and M2 macrophages. PLoS ONE. 2013;8(11):e80908.
Lundquist R, Dziegel MH, Agren MS. Bioactivity and stability of endogenous fibrogenic factors in platelet-rich fibrin. Wound Repair Regen. 2008;16:356–63.
Isobe K, Suzuki M, Watanabe T, Kitamura Y, Suzuki T, Kawabata H, Nakamura M, Okudera T, Okudera H, Uematsu K, et al. Platelet-rich fibrin prepared from stored whole-blood samples. Int J Implant Dent. 2017;3(1):6.
O’Connell SM, Impeduglia T, Hessler K, Wang XJ, Carroll RJ, Dardik H. Autologous platelet rich fibrin matrix as cell therapy in the healing of chronic lower-extremity ulcers. Wound Repair Regen. 2017;16:749–56.
Yu P, Zhai Z, Jin X, Yang X, Qi Z. Clinical application of platelet-rich fibrin in plastic and reconstructive surgery: a systematic review. Aesthetic Plast Surg. 2018;42:511–9.
Yamaguchi R, Terashima H, Yoneyama S, Tadano S, Ohkohchi N. Effects of platelet-rich plasma on intestinal anastomotic healing in rats: PRP concentration is a key factor. J Surg Res. 2012;173:258–66.
Byrne DJ, Hardy J, Wood RA, McIntosh R, Hopwood D, Cuschieri A. Adverse influence of fibrin sealant on the healing of high-risk sutured colonic anastomoses. J R Coll Surg Edinb. 1992;37:394–8.
Fresno L, Fondevila D, Banmbo O, Chacaltana A, Garcia F, Andaluz A. Effects of platelet-rich plasma on intestinal wound healing in pigs. Vet J. 2010;185:322–7.
Fajardo AD, Chun J, Stewart D, Safar B, Fleshman JW. 1.5:1 meshed AlloDerm bolsters for stapled rectal anastomoses does not provide any advantage in anastomotic strength in a porcine model. Surg Innov. 2011;18(1):21–8.
Yol S, Tekin A, Yilmaz H, Kucukkartallar T, Esen H, Caglayan O, Tatkan Y. Effects of platelet rich plasma on colonic anastomosis. J Surg Res. 2008;146:190–4.
Krarup P‑M, Eld M, Heiemeier K, Jorgensen LN, Hansen MB, Ågren MS. Expression and inhibition of matrix metalloproteinase (MMP)-8, MMP-9 and MMP-12 in early colonic anastomotic repair. Int J Colorectal Dis. 2013;28:1151–519.
Shogan BD, Smith DP, Christley S, Gilbert JA, Zaborina O, Alverdy JC. Intestinal anastomotic injury alters spatially defined microbiome composition and function. Microbiome. 2014;2:35.
Shogan BD, Belogortseva N, Luong PM, Zaborin A, Lax S, Bethel C, Ward M, Muldoon JP, Singer M, An G, Umanskiy K, Konda V, Shakhsheer B, Luo J, Klabbers R, Hancock LE, Gilbert J, Zaborina O, Alverdy JC. Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci Transl Med. 2015;7:286ra68. https://doi.org/10.1126/scitranslmed.3010658.
Skowron KB, Shogan BD, Rubin DT, Hyman NH. The new frontier: the intestinal microbiome and surgery. J Gastrointest Surg. 2018;22:1277–85.
Funding
The study presented was sponsored by GergMed Medizintechnik, Baiern, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Dauser, W. Heitland, F.G. Bader, W. Brunner and A.P. Zbar have no personal financial ties to Vivostat®, Allerød, Denmark or GergMed Medizintechnik, Baiern, Germany, or patent holdings etc. to declare. Y. Nir works as a consultant for GergMed Medizintechnik, Baiern, Germany.
Ethical standards
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Bernhard Dauser, Wolf Heitland, Franz Bader, Walter Brunner and Yael Nir contributed equally to conception and design of the study, analysis and interpretation of data, and drafting of the manuscript. Andrew P. Zbar assisted with manuscript draft preparation and critical review of manuscript.
Rights and permissions
About this article
Cite this article
Dauser, B., Heitland, W., Bader, F.G. et al. Histologic changes in early colonic anastomotic healing using autologous platelet-rich fibrin matrix. Eur Surg 52, 155–164 (2020). https://doi.org/10.1007/s10353-019-0578-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-019-0578-9