Abstract
Purpose
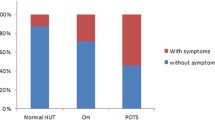
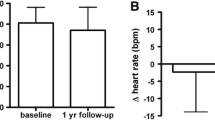
Postural orthostatic tachycardia syndrome (POTS) in adults is defined as symptoms of chronic orthostatic intolerance (COI) and autonomic dysfunction (AD) with heart rate (HR) increase of 30 beats per minute (bpm), or HR > 120 bpm, during prolonged upright position. However, in adolescents, POTS is defined as symptoms of OI and AD with HR increase of ≥ 40 bpm, based on tilt table data. We assessed frequency of COI symptoms in pediatric patients versus HR criteria on prolonged standing to evaluate using criteria of increased HR of 30–39 bpm versus ≥ 40 bpm in our POTS Program.
Methods
Patients with COI with symptoms for > 3 months plus HR increase of ≥ 30 bpm on 10 min stand aged ≤ 18 years at diagnosis were included. Patients were divided into two groups: those with HR increase of 30–39 bpm, and those with HR increase of ≥ 40 bpm or upright HR of > 120 bpm. A total of 28 symptoms described prior to diagnosis were evaluated using chi-square testing to assess for significant differences.
Results
Only insomnia was found to be significantly different between the two groups. The other 27 symptoms showed no significant difference as a function of HR.
Conclusion
There are minimal statistically significant differences and no clinical differences between patients as a function of HR increase during standing. Thus, a 40-bpm threshold for adolescents on standing test may be too high, or a specific HR criteria threshold is neither predictive nor definitive in diagnosing POTS.





Similar content being viewed by others
References
Raj SR, Black BK, Biaggioni I, Harris PA, Robertson D (2005) Acetylcholinesterase inhibition improves tachycardia in postural tachycardia syndrome. Circulation 111:2734–2740
Hoeldtke RD, Bryner KD, Hoeldtke ME, Hobbs G (2006) Treatment of postural tachycardia syndrome: a comparison of octreotide and midodrine. Clin Auton Res 16:390–395
Singer W, Sletten DM, Opfer-Gehrking TL, Brands CK, Fischer PR, Low PA (2012) Postural tachycardia in children and adolescents: what is abnormal? J Pediatr 160:222–226
Sheldon RS, Grubb BP 2nd, Olshansky B et al (2015) 2015 Heart Rhythm Society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm 12:e41–e63
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-drive methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Stewart JM, Boris JR, Chelimsky G et al (2018) Pediatric disorders of orthostatic intolerance. Pediatrics 141(1):e20171673. https://doi.org/10.1542/peds.2017-1673
Mathias CJ, Low DA, Iodice V, Owens AP, Kirbis M, Grahame R (2011) Postural tachycardia syndrome—current experience and concepts. Nat Rev Neurol 8:22–34
Jiawei L, Qingyou Z, Hongjun H, Hongfang J, Junbao D (2014) Clinical features and management of postural tachycardia syndrome in children: a single-center experience. Chin Med J127:3684–3689
Boris JR, Bernadzikowski T (2018) Demographics of a large paediatric postural orthostatic tachycardia syndrome program. Cardiol Young 28:668–674
Silverman BW (1986) Density estimation for statistics and data analysis. Chapman and Hall, London
Landgraf AJ, Lee Y (2015) Dimensionality reduction for binary data through the projection of natural parameters. arXiv:1510.06112
Stewart JM, Clarke D (2011) “He’s dizzy when he stands up”. An introduction to initial orthostatic hypotension. J Pediatr 158:499–504
Langhagen T, Albers L, Heinen F et al (2015) Period prevalence of dizziness and vertigo in adolescents. PLoS One 10:e0136512
Ganzeboom KS, Colman N, Reitsma JB, Shen WK, Wieling W (2003) Prevalence and triggers of syncope in medical students. Am J Cardiol 91:1006–1008
De Jong-deVos van Steenwijk CCE, Wieling W, Harms MPM, Wesseling KH (1997) Variability of near-fainting responses in healthy 6–16-year-old subjects. Clin Sci (Lond) 93:205–211
Freeman R (2003) Treatment of orthostatic hypotension. Semin Neurol 23:435–442
Frishman WH, Azer V, Sica D (2003) Drug treatment of orthostatic hypotension and vasovagal syncope. Heart Dis 5:49–64
Ruzieh M, Batizy L, Dasa O, Oostra C, Grubb B (2017) The role of autoantibodies in the syndromes of orthostatic intolerance: a systematic review. Scan Cardiovasc J 51:243–247
Watari M, Nakane S, Mukaino A et al (2018) Autoimmune postural orthostatic tachycardia syndrome. Ann Clin Transl Neurol 5:486–492
Yu X, Li H, Murphy TA et al (2018) Angiotensin II type 1 receptor autoantibodies in postural tachycardia syndrome. J Am Heart Assoc. https://doi.org/10.1161/JAHA.117.008351
Skinner JE, Driscoll SW, Porter CJ et al (2010) Orthostatic heart rate and blood pressure in adolescents: reference ranges. J Child Neurol 25:1210–1215
Chelimsky G, Kovacic K, Nugent M, Mueller A, Simpson P, Chelimsky TC (2015) Comorbid conditions do not differ in children and young adults with functional disorders with or without postural tachycardia syndrome. J Pediatr 167:120–124
Ives CT, Kimpinski K (2014) Higher heart rate increments on head-up tilt in control subjects are not associated with autonomic dysfunction. Clin Neurophysiol 125:2109–2114
Parsaik AJ, Singer W, Allison TG et al (2013) Orthostatic intolerance without postural tachycardia: how much dysautonomia? Clin Auton Res 23:181–188
Plash WB, Diedrich A, Biaggioni I et al (2013) Diagnosing postural tachycardia syndrome: comparison of tilt testing compared with standing haemodynamics. Clin Sci (Lond) 124:109–114
Berkowitz JB, Auld D, Hulse JE, Campbell RM (1995) Tilt table evaluation for control pediatric patients: comparison with symptomatic patients. Clin Cardiol 18:521–525
Brignole M, Sutton R, Menozzi C et al (2006) Lack of correlation between the responses to tilt testing and adenosine triphosphate test and the mechanism of spontaneous neurally mediated syncope. Eur Heart J 27:2232–2239
Acknowledgements
The authors would like to acknowledge the excellent assistance and review work of Andrew Glatz, MD, MSCE. As well, we would like to thank Andrea Kennedy, Arya Boris, Robert Rennie, and Elizabeth Schoenberg for the creation of and the updating within the CHOP POTS Database. Finally, we acknowledge the excellent support of the Cardiac Center Research Core at the Children’s Hospital of Philadelphia.
Funding
The creation of the CHOP POTS database was supported by the Cardiac Center of the Children’s Hospital of Philadelphia. Partial funding for personnel working on the database was provided by Dysautonomia International.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Boris, J.R., Huang, J. & Bernadzikowski, T. Orthostatic heart rate does not predict symptomatic burden in pediatric patients with chronic orthostatic intolerance. Clin Auton Res 30, 19–28 (2020). https://doi.org/10.1007/s10286-019-00622-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-019-00622-y