Abstract
Background
To evaluate whether serum N-glycan profile can be used as a diagnostic marker of graft rejection after living-donor kidney transplants (KT).
Methods
We retrospectively examined 174 KT recipients at five medical centers. N-Glycan levels were analyzed in postoperative serum samples using glycoblotting combined with mass spectrometry. We developed an integrated score to predict graft rejection based on a combination of age, gender, immunological risk factors, and serum N-glycan levels at post-KT day D1 and D7. Rejection-free survival rates stratified by the sum of integrated scores (D1 + D7) were evaluated using Kaplan–Meier curves.
Results
Of 174, 52 showed graft rejection (Rejection-pos. group) and 122 recipients did not show graft rejection (Rejection-neg. group). The integrated scores were significantly higher in the Rejection-pos. group than those of the Rejection-neg. group. Area-under-curve (AUC) value of integrated scores at post-KT D1, and D7 were 0.84 and 0.84, respectively. The sum of integrated scores (D1 + D7) ≥ 0.50 identified graft rejection with 81% sensitivity and 80% specificity; with an AUC value of 0.87. Recipients with higher sum of integrated scores (D1 + D7 ≥ 0.5) had significantly shorter rejection-free survival than those with lower scores.
Conclusion
Evaluation of serum N-glycosylation profiles can identify recipients who are prone to rejection.





Similar content being viewed by others
References
Okumi M, Unagami K, Kakuta Y, Ochi A, Takagi T, Ishida H, et al. Elderly living donor kidney transplantation allows worthwhile outcomes: the Japan Academic Consortium of Kidney Transplantation study. Int J Urol. 2017;24(12):833–40. https://doi.org/10.1111/iju.13443.
Kubota Y, Hatakeyama S, Narita I, Shimada M, Hashimoto Y, Ohyama C. Clinical impact of glomerular basement membrane thickness on post-donation renal function in living donors. Int J Urol. 2019;26(2):309–11. https://doi.org/10.1111/iju.13850.
Kusaka M, Kubota Y, Takahashi H, Sasaki H, Kawai A, Takenaka M, et al. Warm ischemic time as a critical risk factor of graft failure from donors after cardiac death: a single-center experience over three decades in the Kidney Donor Profile Index/Kidney Donor Risk Index era in Japan. Int J Urol. 2019;26(2):247–52. https://doi.org/10.1111/iju.13851.
Nishioka T, Yoshimura N, Ushigome H, Watarai Y, Nishimura K, Akioka K, et al. High-dose mizoribine combined with calcineurin inhibitor (cyclosporine or tacrolimus), basiliximab and corticosteroids for renal transplantation: a Japanese multicenter study. Int J Urol. 2018;25(2):141–5. https://doi.org/10.1111/iju.13476.
Hamano I, Hatakeyama S, Yamamoto H, Fujita T, Murakami R, Shimada M, et al. Impact of distance between donor and recipient hospitals on cadaveric kidney transplantation outcomes. Clin Exp Nephrol. 2019;23(6):807–13. https://doi.org/10.1007/s10157-019-01710-z.
Ma MK, Law HK, Tse KS, Chan KW, Chan GC, Yap DY, et al. Non-invasive assessment of kidney allograft fibrosis with shear wave elastography: a radiological-pathological correlation analysis. Int J Urol. 2018;25(5):450–5. https://doi.org/10.1111/iju.13536.
Takeuchi A, Kato K, Akashi K, Eto M. Cyclophosphamide-induced tolerance in kidney transplantation avoids long-term immunosuppressive therapy. Int J Urol. 2018;25(2):112–20. https://doi.org/10.1111/iju.13474.
Kakuta Y, Imamura R, Okumi M, Horio M, Isaka Y, Ichimaru N, et al. Assessment of renal function in living kidney donors before and after nephrectomy: a Japanese prospective, observational cohort study. Int J Urol. 2019;26(4):499–505. https://doi.org/10.1111/iju.13923.
Hatakeyama S, Fujita T, Murakami R, Suzuki Y, Sugiyama N, Yamamoto H, et al. Outcome comparison of ABO-incompatible kidney transplantation with low-dose rituximab and ABO-compatible kidney transplantation: a single-center experience. Transplant Proc. 2014;46(2):445–8. https://doi.org/10.1016/j.transproceed.2013.09.036.
Maenosono R, Unagami K, Kakuta Y, Furusawa M, Okumi M, Azuma H, et al. Association between response to rituximab and antibody-mediated rejection in ABO-incompatible living kidney transplantation. Int J Urol. 2019. https://doi.org/10.1111/iju.14108.
Tasaki M, Saito K, Nakagawa Y, Imai N, Ito Y, Yoshida Y, et al. Analysis of the prevalence of systemic de novo thrombotic microangiopathy after ABO-incompatible kidney transplantation and the associated risk factors. Int J Urol. 2019. https://doi.org/10.1111/iju.14118.
Erpicum P, Hanssen O, Weekers L, Lovinfosse P, Meunier P, Tshibanda L, et al. Non-invasive approaches in the diagnosis of acute rejection in kidney transplant recipients, part II: omics analyses of urine and blood samples. Clin Kidney J. 2017;10(1):106–15. https://doi.org/10.1093/ckj/sfw077.
Malard-Castagnet S, Dugast E, Degauque N, Pallier A, Soulillou JP, Cesbron A, et al. Sialylation of antibodies in kidney recipients with de novo donor specific antibody, with or without antibody mediated rejection. Hum Immunol. 2016;77(11):1076–83. https://doi.org/10.1016/j.humimm.2015.10.021.
Noro D, Yoneyama T, Hatakeyama S, Tobisawa Y, Mori K, Hashimoto Y, et al. Serum aberrant N-glycan profile as a marker associated with early antibody-mediated rejection in patients receiving a living donor kidney transplant. Int J Mol Sci. 2017;18(8):1731. https://doi.org/10.3390/ijms18081731.
Ohyama C, Tsuboi S, Fukuda M. Dual roles of sialyl Lewis X oligosaccharides in tumor metastasis and rejection by natural killer cells. EMBO J. 1999;18(6):1516–25. https://doi.org/10.1093/emboj/18.6.1516.
Tsuboi S, Sutoh M, Hatakeyama S, Hiraoka N, Habuchi T, Horikawa Y, et al. A novel strategy for evasion of NK cell immunity by tumours expressing core2 O-glycans. EMBO J. 2011;30(15):3173–85. https://doi.org/10.1038/emboj.2011.215.
Tsuboi S, Hatakeyama S, Ohyama C, Fukuda M. Two opposing roles of O-glycans in tumor metastasis. Trends Mol Med. 2012;18(4):224–32. https://doi.org/10.1016/j.molmed.2012.02.001.
Hatakeyama S, Amano M, Tobisawa Y, Yoneyama T, Tsuchiya N, Habuchi T, et al. Serum N-glycan alteration associated with renal cell carcinoma detected by high throughput glycan analysis. J Urol. 2014;191(3):805–13. https://doi.org/10.1016/j.juro.2013.10.052.
Ishibashi Y, Tobisawa Y, Hatakeyama S, Ohashi T, Tanaka M, Narita S, et al. Serum tri- and tetra-antennary N-glycan is a potential predictive biomarker for castration-resistant prostate cancer. Prostate. 2014;74(15):1521–9. https://doi.org/10.1002/pros.22869.
Oikawa M, Hatakeyama S, Yoneyma T, Tobisawa Y, Narita T, Yamamoto H, et al. Significance of serum N-glycan profiling as a diagnostic biomarker in urothelial carcinoma. Eur Urol Focus. 2018;4(3):405–11. https://doi.org/10.1016/j.euf.2016.11.004.
Narita T, Hatakeyama S, Yoneyama T, Narita S, Yamashita S, Mitsuzuka K, et al. Clinical implications of serum N-glycan profiling as a diagnostic and prognostic biomarker in germ-cell tumors. Cancer Med. 2017;6(4):739–48. https://doi.org/10.1002/cam4.1035.
Yoneyama T, Ohyama C, Hatakeyama S, Narita S, Habuchi T, Koie T, et al. Measurement of aberrant glycosylation of prostate specific antigen can improve specificity in early detection of prostate cancer. Biochem Biophys Res Commun. 2014;448(4):390–6. https://doi.org/10.1016/j.bbrc.2014.04.107.
Ishikawa T, Yoneyama T, Tobisawa Y, Hatakeyama S, Kurosawa T, Nakamura K, et al. An automated micro-total immunoassay system for measuring cancer-associated α2,3-linked sialyl N-glycan-carrying prostate-specific antigen may improve the accuracy of prostate cancer diagnosis. Int J Mol Sci. 2017;18(2):470. https://doi.org/10.3390/ijms18020470.
Tanaka T, Yoneyama T, Noro D, Imanishi K, Kojima Y, Hatakeyama S, et al. Aberrant N-glycosylation profile of serum immunoglobulins is a diagnostic biomarker of urothelial carcinomas. Int J Mol Sci. 2017;18(12):2632. https://doi.org/10.3390/ijms18122632.
Hatakeyama S, Amano M, Tobisawa Y, Yoneyama T, Tsushima M, Hirose K, et al. Serum N-glycan profiling predicts prognosis in patients undergoing hemodialysis. Sci World J. 2013;2013:268407. https://doi.org/10.1155/2013/268407.
Haas M. The revised (2013) banff classification for antibody-mediated rejection of renal allografts: update, difficulties, and future considerations. Am J Transplant. 2016;16(5):1352–7. https://doi.org/10.1111/ajt.13661.
Nara M, Komatsuda A, Numakura K, Saito M, Inoue T, Niioka T, et al. Quantification of interstitial fibrosis in renal allografts and clinical correlates of long-term graft function. Am J Nephrol. 2017;46(3):187–94. https://doi.org/10.1159/000479983.
Takeuchi M, Amano M, Kitamura H, Tsukamoto T, Masumori N, Hirose K, et al. N- and O-glycome analysis of serum and urine from bladder cancer patients using a high-throughput glycoblotting method. J Glycom Lipidom. 2013;3(108):1–8. https://doi.org/10.4172/2153-0637.1000108.
Uchida J, Kosoku A, Naganuma T, Tanaka T, Nakatani T. Latest insights on ABO-incompatible living-donor renal transplantation. Int J Urol. 2019. https://doi.org/10.1111/iju.14109.
Quast I, Keller CW, Maurer MA, Giddens JP, Tackenberg B, Wang LX, et al. Sialylation of IgG Fc domain impairs complement-dependent cytotoxicity. J Clin Invest. 2015;125(11):4160–70. https://doi.org/10.1172/jci82695.
Hess C, Winkler A, Lorenz AK, Holecska V, Blanchard V, Eiglmeier S, et al. T cell-independent B cell activation induces immunosuppressive sialylated IgG antibodies. J Clin Invest. 2013;123(9):3788–96. https://doi.org/10.1172/jci65938.
Amano M, Yamaguchi M, Takegawa Y, Yamashita T, Terashima M, Furukawa J, et al. Threshold in stage-specific embryonic glycotypes uncovered by a full portrait of dynamic N-glycan expression during cell differentiation. Mol Cell Proteom. 2010;9(3):523–37. https://doi.org/10.1074/mcp.M900559-MCP200.
Dijk van W, Havenaar EC, Brinkman-van der Linden EC. Alpha 1-acid glycoprotein (orosomucoid): pathophysiological changes in glycosylation in relation to its function. Glycoconj J. 1995;12(3):227–33.
Acknowledgements
The authors are grateful to Takahiro Yoneyama, Satomi Sakamoto, Yukie Nishizawa, Itsuto Hamano, Naoki Fujita, Takuma Narita, and Yuki Fujita for their invaluable help with sample collection and patient data management.
Funding
This work was supported by a Grant-in-Aid for Scientific Research (Nos. 15H02563, 17K11119, and 19H05556) from the Japan Society for the Promotion of Science, and Japanese Society for Clinical Renal Transplant grant-in-aid for multicenter clinical research Grant 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Human and animal rights
This study was performed in accordance with the ethical standards of the Declaration of Helsinki and was approved by the Ethics Committee of the Hirosaki University Graduate School of Medicine (approval number: 2014–195).
Informed consent
Written informed consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10157_2019_1820_MOESM1_ESM.pdf
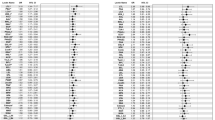
Supplementary file1 (PDF 1808 kb) Figure S1. Schematic representation of the 35 types of N-glycans identified by N-glycomics. Putative structures of the N-glycans are represented using monosaccharide symbols. Yellow circles, galactose (Gal); green circles, mannose (Man); blue squares, N-acetylglucosamine (GlcNAc); red triangles, fucose (Fuc); and purple diamonds, N-acetylneuraminic acid (sialic acid).Figure S2. Representative MALDI-TOF mass spectra. Representative MALDI-TOF mass spectra (m/z range of 1250 to 4000) of benzyloxyamine (BOA)-labeled N-glycans derived from the serum of patients in kidney transplantation at day 1 and 7 were shown. A mass spectrum of serum N-glycans from a patient who did not develop any adverse events (A). A mass spectrum of serum N-glycans from a patient who developed ABMR (B). A mass spectrum of serum N-glycans from a patient who developed TCMR (C), A mass spectrum of serum N-glycans from a patient who developed ABMR and TCMR (D). Figure S3. The AUC for immunological risks and pure N-glycan score.The AUC for ABOi-KT, preformed DSA status, rituximab use, and the sum of immunological risks (ABOi-KT, preformed DSA positive, plus rituximab use) were 0.59 (A; P = 0.055), 0.54 (B; P = 0.373), 0.59 (C; P = 0.078), and 0.62 (D; P = 0.012), respectively. When we compared the pure N-glycan score (without age, sex, ABO compatibility, rituximab administration, and presence of DSA) and integrated score using ROC curve, there was no significant difference in the AUC value between the pure N-glycan score and integrated score in D1 (E; AUC 0.84 vs. 0.84, respectively, P = 0.609), D7 (F; AUC 0.83 vs 0.84, respectively, P = 0.564), and D1+D7 (G; AUC 0.87 vs 0.87, respectively, P = 0.551).
About this article
Cite this article
Soma, O., Hatakeyama, S., Yoneyama, T. et al. Serum N-glycan profiling can predict biopsy-proven graft rejection after living kidney transplantation. Clin Exp Nephrol 24, 174–184 (2020). https://doi.org/10.1007/s10157-019-01820-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01820-8