Abstract
Purpose
This study used a network meta-analysis to evaluate the efficacy and safety of different surgical approaches in patients with hemorrhoids.
Methods
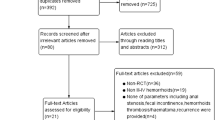
PubMed, Embase, Web of science, and Cochrane Library were searched for randomized controlled trials on patients with hemorrhoids treated by different surgical procedures. The search was conducted until January 15, 2023. Two investigators independently screened the resulting literature, extracted information, evaluated the risk of bias of the included studies, and performed a network meta-analysis.
Result
A total of 23 randomized controlled studies were included and involved 3573 patients and 10 interventions, namely L (Ligasure), M-M (Milligan-Morgan), F (Ferguson), H (Harmonic), OH (open Harmonic), CH (closed Harmonic), PPH (procedure for prolapse and hemorrhoids), TST (tissue selecting technique), T-S (TST STARE+; tissue selection therapy stapled transanal rectal resection plus), and STARR (stapled transanal rectal resection). Network meta-analysis results showed that L has the shortest mean operating time and STARR has the longest mean operating time, F and H have the longest length of hospitalization and T-S has the shortest length of hospitalization, PPH has the most intraoperative blood loss and L has the least intraoperative blood loss, TST has the shortest time to first defecation and M-M has the longest time to first defecation, STARR had the least recurrence and PPH had the most recurrence, PPH had the least anal stenosis and L had the most anal stenosis, and F had the least postoperative pain after 24 h and PPH had the most postoperative pain after 24 h.
Conclusion
Current evidence suggests that L is best at reducing mean operative time and intraoperative bleeding, T-S is best at reducing mean length of stay, TST has the shortest time to first defecation, STARR is best at reducing recurrence rates, PPH is best at reducing postoperative anal stricture, and F is best at reducing postoperative pain after 24 h.











Similar content being viewed by others
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary Information.
Abbreviations
- L:
-
Ligasure
- M-M:
-
Milligan-Morgan
- F:
-
Ferguson
- H:
-
Harmonic
- OH:
-
Open Harmonic
- CH:
-
Closed Harmonic
- PPH:
-
Procedure for prolapse and hemorrhoids
- TST:
-
Tissue Selecting Technique
- T-S:
-
TST STARE+ (tissue selection therapy stapler stapled transanal rectal resection plus)
- S:
-
STARR (stapled transanal rectal resection)
- MD:
-
Mean difference
- CI:
-
Confidence interval
- OR:
-
Odds ratio
References
Schubert MC, Sridhar S, Schade RR, Wexner SD (2009) What every gastroenterologist needs to know about common anorectal disorders. World J Gastroenterol 15(26):3201–3209. https://doi.org/10.3748/wjg.15.3201
Gardner IH, Siddharthan RV, Tsikitis VL (2020) Benign anorectal disease: hemorrhoids, fissures, and fistulas. Ann Gastroenterol 33(1):9–18. https://doi.org/10.20524/aog.2019.0438
Mott T, Latimer K, Edwards C (2018) Hemorrhoids: diagnosis and treatment options. Am Fam Phys 97(3):172–179
Trenti L, Biondo S, Kreisler ME et al (2019) Short-term outcomes of transanal hemorrhoidal dearterialization with mucopexy versus vessel-sealing device hemorrhoidectomy for grade III to IV hemorrhoids: a prospective randomized multicenter trial. Dis Colon Rectum 62(8):988–996. https://doi.org/10.1097/DCR.0000000000001362
Zagriadskiĭ EA, Bogomazov AM, Golovko EB (2018) Conservative treatment of hemorrhoids: results of an observational multicenter study. Adv Ther 35(11):1979–1992. https://doi.org/10.1007/s12325-018-0794-x
Orangio GR (2020) Expert commentary on the evaluation and management of hemorrhoids. Dis Colon Rectum 63(4):424–426. https://doi.org/10.1097/DCR.0000000000001643
Lohsiriwat V (2012) Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol 18(17):2009–2017. https://doi.org/10.3748/wjg.v18.i17.2009
Lohsiriwat V (2015) Treatment of hemorrhoids: a coloproctologist’s view. World J Gastroenterol 21(31):9245–9252. https://doi.org/10.3748/wjg.v21.i31.9245
Acheson AG, Scholefield JH (2008) Management of haemorrhoids. BMJ 336(7640):380–383. https://doi.org/10.1136/bmj.39465.674745.80
Cengiz TB, Gorgun E (2019) Hemorrhoids: a range of treatments. Cleve Clin J Med 86(9):612–620. https://doi.org/10.3949/ccjm.86a.18079
Matsukuma K, Gui D, Saadai P (2023) Hirschsprung disease for the practicing surgical pathologist. Am J Clin Pathol 159(3):228–241. https://doi.org/10.1093/ajcp/aqac141
Talaie R, Torkian P, Moghadam AD et al (2022) Hemorrhoid embolization: a review of current evidences. Diagn Interv Imaging 103(1):3–11. https://doi.org/10.1016/j.diii.2021.07.001
Hollingshead JR, Phillips R (2016) Haemorrhoids: modern diagnosis and treatment. Postgrad Med J 92(1083):4–8. https://doi.org/10.1136/postgradmedj-2015-133328
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Nikolakopoulou A, Higgins JPT, Papakonstantinou T et al (2020) CINeMA: an approach for assessing confidence in the results of a network meta-analysis. PLOS Med 17:e1003082
Chen S, Lai DM, Yang B, Zhang L, Zhou TC, Chen GX (2007) Therapeutic comparison between procedure for prolapse and hemorrhoids and Ligasure technique for hemorrhoids. Zhonghua Wei Chang Wai Ke Za Zhi 10(4):342–345
Chung YC, Wu HJ (2003) Clinical experience of sutureless closed hemorrhoidectomy with LigaSure. Dis Colon Rectum 46(1):87–92. https://doi.org/10.1007/s10350-004-6501-9
Ding JH, Zhao K, Jiang RX et al (2009) Comparison of long-term efficacy on severe hemorrhoids between procedure for prolapse and hemorrhoids and Milligan-Morgan hemorrhoidectomy. Zhonghua Wei Chang Wai Ke Za Zhi 12(4):382–855
Gao RZ, Liang XB, Xu CN, Zhang JY, Wang P, Niu HG (2008) Comparison of two-year efficacy between procedure for prolapse and hemorrhoids and Milligan-Morgan hemorrhoidectomy in treatment of III and IV degree internal hemorrhoids. Zhonghua Wei Chang Wai Ke Za Zhi 11(3):249–252
Haksal MC, Çiftci A, Tiryaki Ç, Yazıcıoğlu MB, Özyıldız M, Yıldız SY (2017) Comparison of the reliability and efficacy of LigaSure hemorrhoidectomy and a conventional Milligan-Morgan hemorrhoidectomy in the surgical treatment of grade 3 and 4 hemorrhoids. Turk J Surg 33(4):233–236. https://doi.org/10.5152/turkjsurg.2017.3493
He H, He P, Liu N (2014) Clinical study of tissue-selecting therapy in the treatment of mixed hemorrhoids: a single-blind randomized controlled trail. Zhonghua Wei Chang Wai Ke Za Zhi 17(6):586–588
Huang H, Tao L, Jiang J, Wei J, Ji L (2023) Tissue-selecting-technique mega-window stapler combined with anal canal epithelial preservation operation in prolapsed hemorrhoids. Asian J Surg 46(2):807–815. https://doi.org/10.1016/j.asjsur.2022.07.149
Khanna R, Khanna S, Bhadani S, Singh S, Khanna AK (2010) Comparison of Ligasure hemorrhoidectomy with conventional Ferguson’s hemorrhoidectomy. Indian J Surg 72(4):294–297. https://doi.org/10.1007/s12262-010-0192-3
Kwok SY, Chung CC, Tsui KK, Li MK (2005) A double-blind, randomized trial comparing Ligasure and Harmonic scalpel hemorrhoidectomy. Dis Colon Rectum 48(2):344–348. https://doi.org/10.1007/s10350-004-0845-z
Lin HC, Luo HX, Zbar AP et al (2014) The tissue selecting technique (TST) versus the Milligan-Morgan hemorrhoidectomy for prolapsing hemorrhoids: a retrospective case-control study. Tech Coloproctol 18(8):739–744. https://doi.org/10.1007/s10151-014-1187-z
Ozer MT, Yigit T, Uzar AI et al (2008) A comparison of different hemorrhoidectomy procedures. Saudi Med J 29(9):1264–1269
Peker K, Inal A, Güllü H et al (2013) Comparison of vessel sealing systems with conventional. Iran Red Crescent Med J 15(6):488–946. https://doi.org/10.5812/ircmj.10180
Ramadan E, Vishne T, Dreznik Z (2022) Harmonic scalpel hemorrhoidectomy: preliminary results of a new alternative method. Tech Coloproctol 6(2):89–92. https://doi.org/10.1007/s101510200019
Ruan N, Chen ZH, Lin XB (2013) Efficacy comparison of tissue selecting therapy stapler and procedure for prolapse and hemorrhoids in the treatment of severe hemorrhoids. Zhonghua Wei Chang Wai Ke Za Zhi 16(7):645–647
Shen K, Wang C, Gao ZD, Jiang KW, Wang YL, Ye YJ (2019) Procedure for prolapse and hemorrhoids versus stapled transanal rectal resection in the treatment of grade IV hemorrhoids. Zhonghua Wei Chang Wai Ke Za Zhi 22(12):1165–1169. https://doi.org/10.3760/cma.j.issn.1671-0274.2019.12.012
Talha A, Bessa S, Abdel WM (2017) Ligasure, Harmonic Scalpel versus conventional diathermy in excisional haemorrhoidectomy: a randomized controlled trial. ANZ J Surg 87(4):252–256. https://doi.org/10.1111/ans.12838
Teksöz S, Aytac E, Yavuz N et al (2011) Comparison of a vessel sealing system with a conventional technique in hemorrhoidectomy. Balkan Med J 28(2):189–192. https://doi.org/10.5174/tutfd.2010.03074.2
Van de Stadt J, D’Hoore A, Duinslaeger M, Chasse E, Penninckx F (2005) Belgian section of colorectal surgery royal belgian society for surgery. Long-term results after excision haemorrhoidectomy versus stapled haemorrhoidopexy for prolapsing haemorrhoids; a Belgian prospective randomized trial. Acta Chir Belg 105(1):44–52
Wang JY, Lu CY, Tsai HL et al (2006) Randomized controlled trial of LigaSure with submucosal dissection versus Ferguson hemorrhoidectomy for prolapsed hemorrhoids. World J Surg 30(3):462–466. https://doi.org/10.1007/s00268-005-0297-1
Wang ZG, Zhang Y, Zeng XD et al (2015) Clinical observations on the treatment of prolapsing hemorrhoids with tissue selecting therapy. World J Gastroenterol 21(8):2490–2496. https://doi.org/10.3748/wjg.v21.i8.2490
Wei J, Ding X, Jiang J, Ji L, Huang H (2022) Indications, feasibility, and safety of TST STARR plus stapler for degree III hemorrhoids: a retrospective study of 125 hemorrhoids patients. Front Surg 9:860150. https://doi.org/10.3389/fsurg.2022.860150
Xiang F, Feng JJ, Sun YQ, Gou YL (2014) Tissue-selecting therapy stapler vs procedure for prolapse and hemorrhoids for treatment of mixed hemorrhoids. World Chin J Digestol 22(25):3753–3758. https://doi.org/10.11569/wcjd.v22.i25.3753
Yan S, Liu X, Qian HH, Yang HJ, Zeng D, Liu DW (2015) Correlation between short-term anal control function and number of pacinian corpuscles in patients undergoing procedure for prolapse and hemorrhoids or Milligan-Morgan hemorrhoidectomy. World Chin J Digestol 23(24):3967–3972. https://doi.org/10.11569/wcjd.v23.i24.3967
Chen SW, Hsin LJ, Lin WN, Tsai YT, Tsai MS, Lee YC (2022) LigaSure versus conventional parotidectomy: a systematic review and meta-analysis. Healthcare (Basel) 10(4):706. https://doi.org/10.3390/healthcare10040706
Karande VC (2015) LigaSure™ 5 mm blunt tip laparoscopic instrument. J Obstet Gynaecol India 65(5):350–352. https://doi.org/10.1007/s13224-015-0745-2
Chen CW, Lai CW, Chang YJ, Hsiao KH (2014) Modified LigaSure hemorrhoidectomy for the treatment of hemorrhoidal crisis. Surg Today 44(6):1056–1062. https://doi.org/10.1007/s00595-013-0650-1
Prokopakis EP, Lachanas VA, Vardouniotis AS, Velegrakis GA (2010) The use of the Ligasure vessel sealing system in head and neck surgery: a report on six years of experience and a review of the literature. B-ENT 6(1):19–25
Xu L, Chen H, Lin G, Ge Q (2015) Ligasure versus Ferguson hemorrhoidectomy in the treatment of hemorrhoids: a meta-analysis of randomized control trials. Surg Laparosc Endosc Percutan Tech 25(2):106–110. https://doi.org/10.1097/SLE
Yuan SM (2020) Harmonic scalpel for internal mammary artery harvest. J Coll Phys Surg Pak 30(5):516–518. https://doi.org/10.29271/jcpsp.2020.05.516
Ziegler L, O’Brien RT (2002) Harmonic ultrasound: a review. Vet Radiol Ultrasound 43(6):501–509
Pereira C, Gururaj S, Varghese B (2022) Harmonic scalpel versus clips for ligation of cystic duct in laparoscopic cholecystectomy: a systematic review. Cureus 14(12):e32335. https://doi.org/10.7759/cureus.32335
Ju M, Wang X, Xia C, Ju Y (2022) Tissue selecting technique for adult women with low rectovaginal fistula. J Chin Med Assoc 85(1):120–123. https://doi.org/10.1097/JCMA.0000000000000663
Lin HC, Lian L, Xie SK, Peng H, Tai JD, Ren DL (2013) The tissue-selecting technique: segmental stapled hemorrhoidopexy. Dis Colon Rectum 56(11):1320–1324. https://doi.org/10.1097/DCR.0b013e3182a4aca5
Corman ML, Carriero A, Hager T et al (2006) Consensus conference on the stapled transanal rectal resection (STARR) for disordered defaecation. Colorectal Dis 8(2):98–101. https://doi.org/10.1111/j.1463-1318.2005.00941.x
Boccasanta P, Venturi M, Stuto A et al (2004) Stapled transanal rectal resection for outlet obstruction: a prospective, multicenter trial. Dis Colon Rectum 47(8):1285–1296. https://doi.org/10.1007/s10350-004-0582-3
Pescatori M, Gagliardi G (2008) Postoperative complications after procedure for prolapsed hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Tech Coloproctol 12(1):7–19. https://doi.org/10.1007/s10151-008-0391-0
Tjandra JJ, Chan MK (2007) Systematic review on the procedure for prolapse and hemorrhoids (stapled hemorrhoidopexy). Dis Colon Rectum 50(6):878–892. https://doi.org/10.1007/s10350-006-0852-3
Du T, Quan S, Dong T et al (2019) Comparison of surgical procedures implemented in recent years for patients with grade III and IV hemorrhoids: a network meta-analysis. Int J Colorectal Dis 34(6):1001–1012. https://doi.org/10.1007/s00384-019-03288-0
Acknowledgements
Acknowledge everyone who participated in this study.
Funding
There was no funding for the research.
Author information
Authors and Affiliations
Contributions
XY contributed to the conception, design, and implementation of the work and analysis, interpretation of data for the work, and drafting and revision of the manuscript. JW contributed to the conception, design, and implementation of the work, interpretation of data for the work, and revision of the manuscript. HY contributed to the design and implementation of the work, acquisition and interpretation of data for the work, and drafting and revision of the manuscript. CM contributed to analysis, interpretation of data for the work, and revision of the manuscript. SC contributed to the design and implementation of the work, and revision of the manuscript. All the authors approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Conflict of interest
There was no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuan, X.G., Wu, J., Yin, H.M. et al. Comparison of the efficacy and safety of different surgical procedures for patients with hemorrhoids: a network meta-analysis. Tech Coloproctol 27, 799–811 (2023). https://doi.org/10.1007/s10151-023-02855-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-023-02855-6