Abstract
Background
Among the techniques investigated to reduce the risk of surgical wound infection or surgical space infection (SSI) in patients having colorectal surgery are topical application of antimicrobials (antibiotics and antiseptics) to the open wound or immediately after closure. The aim of the present study was to perform a systematic review of the literature on those treatments, with the exception of antibiotic ointments applied to closed skin, which are adequately assessed elsewhere, and a meta-analysis.
Methods
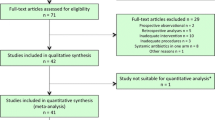
Only randomized trials of patients having only colorectal surgery were included in this review. Studies were sought in MEDLINE, EMBASE, the Cochrane Register of Controlled Trials, Clinical Trials.gov, and the World Health Organization Internet clinical trials register portal. In addition, reference lists of included studies and other published reviews were screened. Meta-analysis was performed for all included studies and subgroup analyses done for each individual intervention. Risk of bias was assessed for each included study, paying particular attention to the preoperative antibiotic prophylaxis used in each study. Sensitivity analyses were done to investigate heterogeneity of the analyses, excluding those studies with a significant risk of bias issues. Absolute risk reduction (RR) was calculated. The overall quality of the evidence for each individual intervention was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, and was classified as high, moderate, low or very low.
Results
A total of 30 studies are included in this review with 5511 patients, 665 of whom had SSI. The interventions included: 10 studies of gentamicin impregnated sponge or beads wound inlays, 4 studies of chlorhexidine impregnated suture, 11 studies of direct wound lavage or powder application or injection of antibiotics before closure, 4 studies of ionized silver dressing applied to the closed skin, and 1 study of vitamin E oil applied to the open wound. All but one study used preoperative antibiotic prophylaxis in addition to topical procedures, although, in some studies, the systemic antibiotic prophylaxis was not the same between groups or varied significantly from the recommended guidelines. Use of gentamycin sponge did not decrease SSI (RR 0.93, 95% CI 0.75–1.16; low-quality evidence) even after including only the studies of abdominal wounds (RR 1.02, 95% CI 0.80–1.30; low-quality evidence). However, sensitivity analysis excluding studies at high risk of bias decreased the heterogeneity and increased the effect of the prophylaxis for all wounds (RR 0.5, 95% CI 0.33–0.78; low-quality evidence) and for abdominal wounds only (RR 0.38, 95% CI 0.20–0.72; moderate-quality evidence). Chlorhexidine impregnated suture showed no effect on SSI (RR 0.79, 95% CI 0.56–1.10; low-quality evidence) and an increased efficacy after sensitivity analysis (RR 0.42, 95% CI 0.22–0.79; low-quality evidence). Antibiotic lavage showed a significant decrease in SSI (RR 0.45, 95% CI 0.26–0.79; low-quality evidence) which increased after sensitivity analysis (RR 0.33, 95% CI 0.15–0.72; moderate-quality evidence). Application of silver dressing to the closed wound resulted in a decrease of SSI (RR 0.55, 95% CI 0.35–0.85; moderate-quality evidence). The one study of topical vitamin E oil applied to the open wound showed a significant risk reduction (RR 0.22, 95% CI 0.05–0.98; low-quality evidence).
Conclusions
Each of these interventions appears to be effective in decreasing SSI, but the number of studies for each is small and the quality of evidence is very low to moderate. Within the various outcomes of GRADE assessment, even a moderate classification suggests that further studies may well have very different results.. No randomized trials exist of combinations of two or more of the above interventions to see if there is a combined effect. Future studies should make sure that the antibiotic used preoperatively is uniform within a study and is consistent with the current guidelines. Deviation from this leads to a significant heterogeneity and risk of bias.









Similar content being viewed by others
Change history
01 April 2019
Unfortunately, an author name (Nuzhat Iqbal) was missed out in the original publication. The complete updated author list is given below.
01 April 2019
Unfortunately, an author name (Nuzhat Iqbal) was missed out in the original publication. The complete updated author list is given below.
References
Baum ML, Anish DS, Chalmers TC, Sacks HS, Smith H Jr, Fagerstrom RM (1981) A survey of clinical trials of antibiotic prophylaxis in colon surgery: evidence against further use of no-treatment controls. N Engl J Med 305:795–799
Nelson RL, Gladman E, Barbateskovic M (2014) Antimicrobial prophylaxis for colorectal surgery. Cochrane Database Syst Rev 9(5):1
Bellows CF, Mills KT, Kelly TN, Gagliardi G (2011) Combination of oral non-absorbable and intravenous antibiotics versus intravenous antibiotics alone in the prevention of surgical site infections after colorectal surgery: a meta-analysis of randomized controlled trials. Tech Coloproctol 15(4):385–395
Anjum N, Ren J, Wang G, Li G, Wu X, Dong H, Wu Q, Li J (2017) A randomized control trial of preoperative oral antibiotics as adjunct therapy to systemic antibiotics for preventing surgical site infection in clean contaminated, contaminated, and dirty type of colorectal surgeries. Dis Colon Rectum 60(12):1291–1298
Intravenous versus Combined Oral and Intravenous Antimicrobial Prophylaxis for the Prevention of Surgical Site Infection in Elective Colorectal Surgery (COMBINE). https://Clinicaltrials.gov. NCT02618720. Accessed 3 July 2018
Greif R, Akça IO, Horn EP, Kurz A, Sessler DI (2000) Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med 342:161–167
Heal CF, Banks JL, Lepper P, Kontopantelis E, van Driel ML (2017) Meta-analysis of randomized and quasi-randomized clinical trials of topical antibiotics after primary closure for the prevention of surgical-site infection. Br J Surg 104(9):1123–1130. https://doi.org/10.1002/bjs.10588. Epub 28 Jun 2017
McHugh SM, Collins CJ, Corrigan MA, Hill ADK, Humphreys H (2011) The role of topical antibiotics used as prophylaxis in surgical site infection prevention. J Antimicrob Chemother 66:693–701
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332
Higgins JPT, Green S (eds) (2011) Cochrane Handbook for systematic reviews of interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. http://handbook.cochrane.org. Accessed 3 July 2018
Armijo-Olivo S, Warren (2009) Magee. Intention to Treat, compliance, drop outs and how to deal with missing data in clinical research: a review. Phys Ther Rev 14(1):36–49
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann HJ (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64(4):383–394
GRADE Handbook. http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html. Accessed 3 July 2018
Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA, Norris S, Vist G, Dahm P, Shukla VK, Higgins J, Falck-Ytter Y, Schünemann HJ, GRADE Working Group. (2011) GRADE guidelines: 7. Rating the quality of evidence–inconsistency. J Clin Epidemiol 64(12):1294–1302. https://doi.org/10.1016/j.jclinepi.2011.03.017
Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, Devereaux PJ, Montori VM, Freyschuss B, Vist G, Jaeschke R, Williams JW Jr, Murad MH, Sinclair D, Falck-Ytter Y, Meerpohl J, Whittington C, Thorlund K, Andrews J, Schünemann HJ (2011) GRADE guidelines 6. Rating the quality of evidence–imprecision. J Clin Epidemiol 64(12):1283–1293
Included studies
Bennett-Guerrero E, Pappas TN, Koltun WA, Fleshman JW, Lin M, Garg J et al (2010) Gentamicin-collagen sponge for infection prophylaxis in colorectal surgery. N Engl J Med 363:103–149
Collin A, Gustafsson UM, Smedh K, Pahlman L, Graf W, Folkesson J (2013) Effect of local gentamicin-collagen on perineal wound complications and cancer recurrence after abdominoperineal resection: a multi-centre randomized controlled trial. Colorectal Dis Off J Assoc of Coloproctol G B Irel 15(3):341–346
Gruessner U, Clemens M, Pahlplatz PV, Sperling P, Witte J, Rosen HR (2001) Improvement of perineal wound healing by local administration of gentamicin-impregnated collagen fleeces after abdominoperineal excision of rectal cancer. Am J Surg 182(5):502–509
Haase O, Raue W, Bohm B, Neuss H, Scharfenberg M, Schwenk W (2005) Subcutaneous gentamicin implant to reduce wound infections after loop-ileostomy closure: a randomized, double-blind, placebo-controlled trial. Dis Colon Rectum 48(11):2025–2031
Nowacki MP, Rutkowski A, Oledzki J, Chwalinski M (2005) Prospective, randomized trial examining the role of gentamycin-containing collagen sponge in the reduction of postoperative morbidity in rectal cancer patients: early results and surprising outcome at 3-year follow-up. Int J Colorectal Dis 20(2):114–120
Pochhammer J, Zacheja S, Schaffer M (2015) Subcutaneous application of gentamicin collagen implants as prophylaxis of surgical site infections in laparoscopic colorectal surgery: a randomized, double-blinded, three-arm trial. Langenbeck’s Archives of Surgery 400(1):1–8
Reith HB, Mittelkotter U, Niedmann M, Debus S, Kozuschek W (1996) Modification of laparotomy wound healing in colon surgery by local antibiotic administration [Beeinflussung der Laparotomiewundheilung in der Kolonchirurgie durch lokale Antibiotikaapplikation]. Zentralblatt fur Chirurgie 121 Suppl:84–85
Rosen HR, Marczell AP, Czerwenka E, Stierer MO, Spoula H, Wasl H (1991) Local gentamicin application for perineal wound healing following abdominoperineal rectum excision. Am J Surg 162(5):438–441
Rutkowski A, Zajac L, Pietrzak L, Bednarczyk M, Byszek A, Oledzki J et al (2014) Surgical site infections following short-term radiotherapy and total mesorectal excision: results of a randomized study examining the role of gentamicin collagen implant in rectal cancer surgery. Tech Coloproctol 18(10):921–928
Rutten HJ, Nijhuis PH (1997) Prevention of wound infection in elective colorectal surgery by local application of a gentamicin-containing collagen sponge. Eur J Surg 578:31–5
Baracs J, Huszar O, Sajjadi SG, Peter Horvath O (2011) Surgical site infections after abdominal closure in colorectal surgery using Triclosan-coated absorbable suture (PDS Plus) vs. uncoated sutures (PDS II): a randomized multicenter study. Surg Infect 12(6):483–489
Mattavelli I, Rebora P, Doglietto G, Dionigi P, Dominioni L, Luperto M et al (2015) Multi-center randomized controlled trial on the effect of triclosan-coated sutures on surgical site infection after colorectal surgery. Surg Infect 16(3):226–235
Nakamura T, Kashimura N, Noji T, Suzuki O, Ambo Y, Nakamura F et al (2013) Triclosan-coated sutures reduce the incidence of wound infections and the costs after colorectal surgery: a randomized controlled trial. Surgery 153(4):576–583
Rasic Z, Schwarz D, Adam VN, Sever M, Lojo N, Rasic D et al (2011) Efficacy of antimicrobial Triclosan-coated polyglactin 910 (Vicryl* Plus) suture for closure of the abdominal wall after colorectal surgery. Coll Antropol 35(2):439–443
Andersen B, Ostergaard AH (1972) Topical Ampicillin against wound infection in colorectal surgery. Ann Surg 172(2):129–132
Greig J, Morran C, Gunn R, Mason B, Sleigh D, McArdle C (1987) Wound sepsis after colorectal surgery: the effect of cefotetan lavage. Chemioterapia 6(2):595–596
Juul P, Merrild U, Kronborg O (1985) Topical ampicillin in addition to a systematic antibiotic prophylaxis in elective colorectal surgery: a prospective randomised study. Dis Colon Rectum 28(11):804–806
Moesgaard F, Nielsen ML, Hjortrup A, Kjersgaard P, Sorensen C, Larsen PN et al (1989) Intraincisional antibiotic in addition to systemic antibiotic treatment fails to reduce wound infection rates in contaminated abdominal surgery. A controlled clinical trial. Dis Colon Rectum 32(1):36–38
Nash AG, Hugh TB (1967) Topical ampicillin and wound infection in colon surgery. BMJ 1(5538):471–472
Ostergaard AH, Wamberg P (1981) Topical or oral antibiotics against wound infection in colorectal surgery. Aktuelle Probleme in Chirurgie Orthopadie 19:105–107
Quendt J, Blank I, Seidel W (1996) Perioperative antibiotic prophylaxis by transperitoneal and subcutaneous application during elective colorectal surgery. A prospective randomized comparative study [Peritoneale und subkutane Applikation von Cefazolin als perioperative Antibiotikaprophylaxe bei kolorektalen Operationen. Prospektive randomisierte Vergleichsstudie bei 200 Patienten]. Langenbecks Arch Chir 381(6):318–322
Raahave D (1981) High-dose penicillin to prevent postoperative wound sepsis after ileocolorectal operations. Scand J Gastroenterol 16(6):789–793
Raahave D, Hesselfeldt P, Pedersen T, Zachariassen A, Kann D, Hansen OH (1989) No effect of topical ampicillin prophylaxis in elective operations of the colon or rectum. Surg Gynecol Obstet 168(2):112–114
Ruiz-Tovar J, Santos J, Arroyo A, Llavero C, Armaanzas L, Lopez-Delgado A et al (2012) Effect of peritoneal lavage with clindamycin-gentamicin solution on infections after elective colorectal cancer surgery. J Am Coll Surg 214(2):202–207
Ruiz-Tovar J, Llavero C, Morales V, Gamallo C (2015) Total occlusive ionic silver-containing dressing vs mupirocin ointment application vs conventional dressing in elective colorectal surgery: effect on incisional surgical site infection. J Am Coll Surg 221(2):424–429
Biffi R, Fattori L, Bertani E, Radice D, Rotmensz N, Misitano P et al (2012) Surgical site infections following colorectal cancer surgery: a randomized prospective trial comparing common and advanced antimicrobial dressing containing ionic silver. World J Surg Oncol 10:94
Krieger BR, Davis DM, Sanchez JE, Mateka JJ, Nfonsam VN, Frattini JC et al (2011) The use of silver nylon in preventing surgical site infections following colon and rectal surgery. Dis Colon Rect 54(8):1014–1019
Siah CJ, Yatim J (2011 Dec) Efficacy of a total occlusive ionic silver-containing dressing combination in decreasing risk of surgical site infection: an RCT. J Wound Care 20(12):561–568
Alias D, Ruiz-Tovar J, Moreno A, Manso B, Diaz G, Duran M et al (2017) Effect of subcutaneous sterile vitamin E ointment on incisional surgical site infection after elective laparoscopic colorectal cancer surgery. Surg Infect 18(3):287–292
Discussion references
Sedgwick P (2014) Randomized controlled trials and subgroup analysis. Br Med J 349:g7513. https://doi.org/10.1136/bmj.g7513
Sterne AC, Egger M, Smith DG (2001) Investigating and dealing with publication bias and other biases in meta-analysis. Br Med J 323:101–105
Charalambous CP, Tryfonidis M, Swindell R, Lipsett AP (2003) When should old therapies be abandoned? A modern look at old studies on topical ampicillin. J Infect 47(3):203–209 (Erratum in: J Infect. 2008 Apr;56(4):297. Charalambous, Charalambos [corrected to Charalambous, Charalambos P] )
Atiyeh BS, Costagliola M, Hayek SN, Dibo SA (2007) Effect of silver on burn wound infection control and healing: review of the literature. Burns 33(2):139–148. (Epub 29 Nov 2006)
Li HZ, Zhang L, Chen JX, Zheng Y, Zhu XN (2017) Silver-containing dressing for surgical site infection in clean and clean-contaminated operations: a systematic review and meta-analysis of randomized controlled trials. J Surg Res 215:98–107. https://doi.org/10.1016/j.jss.2017.03.040. (Epub 2 Apr 2017)
Politano AD, Campbell KT, Rosenberger LH, Sawyer RG (2013) Use of silver in the prevention and treatment of infections: silver review. Surg Infect (Larchmt) 14(1):8–20. https://doi.org/10.1089/sur.2011.097. (Epub 28 Feb 2013)
de Bruin AF, Gosselink MP, van der Harst E, Rutten HJ (2010) Local application of gentamicin collagen implants in the prophylaxis of surgical site infections following gastrointestinal surgery: a review of clinical experience. Tech Coloproctol 14(4):301–310. https://doi.org/10.1007/s10151-010-0593-0. (Epub 29 Jun 2010)
Daoud FC, Edmiston CE Jr, Leaper D (2014) Meta-analysis of prevention of surgical site infections following incision closure with Triclosan-coated sutures: robustness to new evidence. Surg Infect (Larchmt) 15(3):165–181. https://doi.org/10.1089/sur.2013.177. (Epub 16 Apr 2014)
Elsolh B, Zhang L, Patel SV (2017 May) The Effect of Antibiotic-coated sutures on the incidence of surgical site infections in abdominal closures: a meta-analysis. J Gastrointest Surg 21(5):896–903. https://doi.org/10.1007/s11605-017-3357-6. (Epub 18 Jan 2017)
Heal CF, Banks JL, Lepper PD, Kontopantelis E, van Driel ML (2016) Topical antibiotics for preventing surgical site infection in wounds healing by primary intention. Cochrane Database Syst Rev 7;11:CD011426
de Jonge SW, Atema JJ, Solomkin JS, Boermeester MA (2017) Meta-analysis and trial sequential analysis of triclosan-coated sutures for the prevention of surgical-site infection. Br J Surg 104(2):e118–e133. https://doi.org/10.1002/bjs.10445. (Epub 17 Jan 2017)
Lv YF, Wang J, Dong F, Yang DH (2016) Meta-analysis of local gentamicin for prophylaxis of surgical site infections in colorectal surgery. Int J Colorectal Dis 31(2):393–402. https://doi.org/10.1007/s00384-015-2454-9. (Epub 27 Nov 2015)
Mueller TC, Loos M, Haller B, Mihaljevic AL, Nitsche U, Wilhelm D, Friess H, Kleeff J, Bader FG (2015) Intra-operative wound irrigation to reduce surgical site infections after abdominal surgery: a systematic review and meta-analysis. Langenbecks Arch Surg 400(2):167–181. https://doi.org/10.1007/s00423-015-1279-x. (Epub 14 Feb 2015)
Musters GD, Burger JW, Buskens CJ, Bemelman WA, Tanis PJ (2015) Local application of gentamicin in the prophylaxis of perineal wound infection after abdominoperineal resection: a systematic review. World J Surg 39(11):2786–2794. https://doi.org/10.1007/s00268-015-3159-5.
Sandini M, Mattavelli I, Nespoli L, Uggeri F, Gianotti L (2016) Systematic review and meta-analysis of sutures coated with Triclosan for the prevention of surgical site infection after elective colorectal surgery according to the PRISMA statement. Medicine (Baltimore). 95(35):e4057. https://doi.org/10.1097/MD.0000000000004057
Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, Abbas M, Atema JJ, Gans S, van Rijen M, Boermeester MA, Egger M, Kluytmans J, Pittet D, Solomkin JS, WHO Guidelines Development Group (2016) New WHO recommendations on reoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 16(12):e276–e287. https://doi.org/10.1016/S1473-3099(16)30398-X. (Epub 2 Nov 2016)
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, Reinke CE, Morgan S, Solomkin JS, Mazuski JE, Dellinger EP, Itani KMF, Berbari EF, Segreti J, Parvizi J, Blanchard J, Allen G, Kluytmans JAJW, Donlan R, Schecter WP (2017) Healthcare infection control practices advisory committee. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152(8):784–791. https://doi.org/10.1001/jamasurg.2017.0904
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Appendix 1: search strategy
Appendix 1: search strategy
Cochrane central (latest issue)
-
1.
MeSH descriptor: [Surgical Wound Infection] explode all trees
-
2.
MeSH descriptor: [Postoperative Complications] explode all trees
-
3.
MeSH descriptor: [Bacterial Infections] explode all trees
-
4.
MeSH descriptor: [Infection] explode all trees
-
5.
MeSH descriptor: [Sepsis] explode all trees
-
6.
(postoperative complication* or infection* or sepsis):ti,ab,kw
-
7.
(#1 or #2 or #3 or #4 or #5 or #6)
-
8.
MeSH descriptor: [Antiinfective Agents] explode all trees
-
9.
MeSH descriptor: [Antibacterial Agents] explode all trees
-
10.
MeSH descriptor: [Antibiotic Prophylaxis] explode all trees
-
11.
MeSH descriptor: [Triclosan] explode all trees
-
12.
(antiinfective or antibiotic* or antimicrobial* or antibacterial* or triclosan* or prophylaxis or premedication or disinfect* or antiseptic*):ti,ab,kw
-
13.
(#8 or #9 or #10 or #11 or #12)
-
14.
MeSH descriptor: [Colorectal Surgery] explode all trees
-
15.
MeSH descriptor: [Colon] explode all trees and with qualifier(s): [Surgery - SU]
-
16.
MeSH descriptor: [Rectum] explode all trees and with qualifier(s): [Surgery - SU]
-
17.
MeSH descriptor: [Colectomy] explode all trees
-
18.
((colon* or rect* or colorect*) and (surgery or operation or resection)):ti,ab,kw
-
19.
(colectom* or colostom*):ti,ab,kw
-
20.
(#14 or #15 or #16 or #17 or #18 or #19)
-
21.
(#7 and #13 and #20)
MEDLINE search strategy
Ovid MEDLINE (1950 to 08/24/2017)
-
1.
exp Surgical Wound Infection/
-
2.
exp Postoperative Complications/
-
3.
exp Bacterial Infections/
-
4.
exp Infection/
-
5.
exp Sepsis/
-
6.
(postoperative complication* or infection* or sepsis).mp.
-
7.
1 or 2 or 3 or 4 or 5 or 6
-
8.
exp Antiinfective Agents/
-
9.
exp Antibacterial Agents/
-
10.
exp Antibiotic Prophylaxis/
-
11.
exp Triclosan/
-
12.
(antiinfective or antibiotic* or antimicrobial* or antibacterial* or triclosan* or prophylaxis or premedication or disinfect* or antiseptic*).mp.
-
13.
8 or 9 or 10 or 11 or 12
-
14.
exp Colorectal Surgery/
-
15.
exp Colon/su [Surgery]
-
16.
exp Rectum/su [Surgery]
-
17.
exp Colectomy/
-
18.
((colon* or rect* or colorect*) and (surgery or operation or resection)).mp.
-
19.
(colectom* or colostom*).mp.
-
20.
14 or 15 or 16 or 17 or 18 or 19
-
21.
7 and 13 and 20
-
22.
randomized-controlled trial.pt.
-
23.
controlled clinical trial.pt.
-
24.
randomized.ab.
-
25.
placebo.ab.
-
26.
clinical trial.sh.
-
27.
randomly.ab.
-
28.
trial.ti.
-
29.
22 or 23 or 24 or 25 or 26 or 27 or 28
-
30.
humans.sh.
-
31.
29 and 30
-
32.
21 and 31
EMBASE search strategy
Ovid EMBASE (1974–08/24/2017)
-
1.
exp surgical infection/
-
2.
exp postoperative complication/pc [Prevention]
-
3.
exp bacterial infection/
-
4.
exp sepsis/
-
5.
(postoperative complication* or infection* or sepsis).mp.
-
6.
1 or 2 or 3 or 4 or 5
-
7.
exp antiinfective agent/
-
8.
exp antibiotic prophylaxis/
-
9.
exp disinfectant agent/
-
10.
(antiinfective or antibiotic* or antimicrobial* or antibacterial* or triclosan* or prophylaxis or premedication or disinfect* or antiseptic*).mp.
-
11.
7 or 8 or 9 or 10
-
12.
exp colorectal surgery/
-
13.
exp colon surgery/
-
14.
exp rectum surgery/
-
15.
exp colon/su [Surgery]
-
16.
exp rectum/su [Surgery]
-
17.
((colon* or rect* or colorect*) and (surgery or operation or resection)).mp.
-
18.
(colectom* or colostom*).mp.
-
19.
12 or 13 or 14 or 15 or 16 or 17 or 18
-
20.
6 and 11 and 19
-
21.
CROSSOVER PROCEDURE.sh.
-
22.
DOUBLE-BLIND PROCEDURE.sh.
-
23.
SINGLE-BLIND PROCEDURE.sh.
-
24.
(crossover* or cross over*).ti,ab.
-
25.
placebo*.ti,ab.
-
26.
(doubl* adj blind*).ti,ab.
-
27.
allocat*.ti,ab.
-
28.
trial.ti.
-
29.
RANDOMIZED-CONTROLLED TRIAL.sh.
-
30.
random*.ti,ab.
-
31.
21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30
-
32.
(exp animal/ or exp invertebrate/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans or man or men or wom?n).ti.)
-
33.
31 not 32
-
34.
20 and 33
Rights and permissions
About this article
Cite this article
Nelson, R.L., Kravets, A., Khateeb, R. et al. Topical antimicrobial prophylaxis in colorectal surgery for the prevention of surgical wound infection: a systematic review and meta-analysis. Tech Coloproctol 22, 573–587 (2018). https://doi.org/10.1007/s10151-018-1814-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-018-1814-1