Abstract
Background
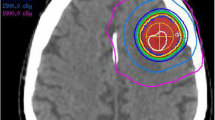
Stereotactic radiosurgery (SRS) effectively treats brain metastases. It can provide local control, symptom relief, and improved survival rates, but it poses challenges in selecting optimal candidates, determining dose and fractionation, monitoring for toxicity, and integrating with other modalities. Practical tools to predict patient outcomes are also needed. Machine learning (ML) is currently used to predict treatment outcomes. We aim to investigate the accuracy of ML in predicting treatment response and local failure of brain metastasis treated with SRS.
Methods
PubMed, Scopus, Web of Science (WoS), and Embase were searched until April 16th, which was repeated on October 17th, 2023 to find possible relevant papers. The study preparation adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline. The statistical analysis was performed by the MIDAS package of STATA v.17.
Results
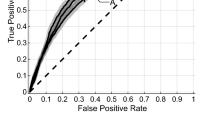
A total of 17 articles were reviewed, of which seven and eleven were related to the clinical use of ML in predicting local failure and treatment response. The ML algorithms showed sensitivity and specificity of 0.89 (95% CI: 0.84–0.93) and 0.87 (95% CI: 0.81–0.92) for predicting treatment response. The positive likelihood ratio was 7.1 (95% CI: 4.5–11.1), the negative likelihood ratio was 0.13 (95% CI: 0.08–0.19), and the diagnostic odds ratio was 56 (95% CI: 25–125). Moreover, the pooled estimates for sensitivity and specificity of ML algorithms for predicting local failure were 0.93 (95% CI: 0.76–0.98) and 0.80 (95% CI: 0.53–0.94). The positive likelihood ratio was 4.7 (95% CI: 1.6–14.0), the negative likelihood ratio was 0.09 (95% CI: 0.02–0.39), and the diagnostic odds ratio was 53 (95% CI: 5-606).
Conclusion
ML holds promise in predicting treatment response and local failure in brain metastasis patients receiving SRS. However, further studies and improvements in the treatment process can refine the models and effectively integrate them into clinical practice.






Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, M.A Habibi, upon reasonable request.
References
Achrol AS et al (2019) Brain metastases. Nat Rev Dis Primers 5(1):5
Sperduto PW et al (2020) Survival in patients with brain metastases: Summary Report on the updated diagnosis-specific graded Prognostic Assessment and Definition of the eligibility quotient. J Clin Oncol 38(32):3773–3784
Steindl A et al (2020) Neurological symptom burden impacts survival prognosis in patients with newly diagnosed non-small cell lung cancer brain metastases. Cancer 126(19):4341–4352
Wu A, Colón GR, Lim M (2022) Quality of life and role of Palliative and supportive care for patients with brain metastases and caregivers: a review. Front Neurol 13:806344
Badiyan SN, Regine WF, Mehta M (2016) Stereotactic radiosurgery for treatment of Brain metastases. J Oncol Pract 12(8):703–712
Yan M et al (2023) Hypofractionated stereotactic radiosurgery (HSRS) as a salvage treatment for brain metastases failing prior stereotactic radiosurgery (SRS). J Neurooncol 162(1):119–128
Gupta S et al (2022) Analysis of prognostic factors in patients with brain metastases affecting survival. J Egypt Natl Canc Inst 34(1):45
Park K et al (2021) Radiotherapy for brain metastasis and long-term survival. Sci Rep 11(1):8046
Mantovani C et al (2021) Modern Radiation Therapy for the management of Brain metastases from Non-small Cell Lung Cancer: current approaches and future directions. Front Oncol 11:772789
Habibi MA et al (2024) The safety and efficacy of dabrafenib and trametinib in patients with glioma: a systematic review and meta-analysis. European Journal of Clinical Pharmacology
Stankiewicz M, Tomasik B, Blamek S (2021) A new prognostic score for predicting survival in patients treated with robotic stereotactic radiotherapy for brain metastases. Sci Rep 11(1):20347
Copeland B Artificial Intelligence. https://www.britannica.com/technology/artificial-intelligence
Habibi MA et al (2023) The performance of machine learning for prediction of H3K27 M mutation in midline gliomas: a systematic review and Meta-analysis. World Neurosurgery
Habibi MA et al (2024) Predicting the radiological outcome of cerebral aneurysm treatment with machine learning algorithms; a systematic review and diagnostic meta-analysis. Interdisciplinary Neurosurg 36:101929
Habibi MA et al (2024) Prediction of cerebral aneurysm rupture risk by machine learning algorithms: a systematic review and meta-analysis of 18,670 participants. Neurosurg Rev 47(1):34
Shahidi R et al (2023) Diagnostic performance of MRI radiomics for classification of Alzheimer’s disease, mild cognitive impairment, and normal subjects: a systematic review and meta-analysis. Aging Clin Exp Res 35(11):2333–2348
Lin YY et al (2023) Application of artificial intelligence to stereotactic radiosurgery for intracranial lesions: detection, segmentation, and outcome prediction. J Neurooncol 161(3):441–450
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Whiting PF et al (2011) QUADAS-2: a revised Tool for the Quality Assessment of Diagnostic Accuracy studies. Ann Intern Med 155(8):529–536
Jaberipour M et al (2021) A priori prediction of local failure in brain metastasis after hypo-fractionated stereotactic radiotherapy using quantitative MRI and machine learning. Sci Rep, 11(1)
Jaberipour M et al (2020) Predicting Local failure after Stereotactic Radiation Therapy in Brain Metastasis using quantitative CT and machine learning(). Annu Int Conf IEEE Eng Med Biol Soc 2020:1323–1326
Wang H et al (2021) Predicting local failure of brain metastases after stereotactic radiosurgery with radiomics on planning MR images and dose maps. Med Phys 48(9):5522–5530
Azimi P, Shahzadi S, Sadeghi S (2020) Use of artificial neural networks to predict the probability of developing new cerebral metastases after radiosurgery alone, vol 64. JOURNAL OF NEUROSURGICAL SCIENCES, pp 52–57. 1
Buzea CG et al (2023) AI evaluation of imaging factors in the evolution of stage-treated metastases using Gamma Knife. Diagnostics (Basel), 13(17).
Moon HC, Park YS (2022) Volume prediction for large brain metastases after hypofractionated gamma knife radiosurgery through artificial neural network. Med (United States) 101(40):E30964
Rodrigues G et al (2014) A clinical nomogram and recursive partitioning analysis to determine the risk of regional failure after radiosurgery alone for brain metastases. Radiother Oncol 111(1):52–58
Cha YJ et al (2018) Prediction of response to stereotactic radiosurgery for brain metastases using convolutional neural networks. Anticancer Res 38(9):5437–5445
Hsu DG et al (2023) Automatically tracking brain metastases after stereotactic radiosurgery. Phys Imaging Radiat Oncol 27:100452
Kawahara D et al (2021) Predicting the local response of metastatic brain tumor to Gamma Knife Radiosurgery by Radiomics with a machine learning method. Front Oncol, 10
Du P et al (2023) Prediction of treatment response in patients with brain metastasis receiving stereotactic radiosurgery based on pre-treatment multimodal MRI radiomics and clinical risk factors: a machine learning model. Front Oncol 13:1114194
Mouraviev A et al (2020) Use of radiomics for the prediction of local control of brain metastases after stereotactic radiosurgery. Neurooncology 22(6):797–805
Gutsche R et al (2022) Radiomics outperforms semantic features for prediction of response to stereotactic radiosurgery in brain metastases: Radiomics for response prediction to stereotactic radiosurgery. Radiother Oncol 166:37–43
Jiang Z et al (2022) Multimodality MRI-based radiomics approach to predict the posttreatment response of lung cancer brain metastases to gamma knife radiosurgery. Eur Radiol 32(4):2266–2276
Du P et al (2023) Development and validation of a radiomics-based prediction pipeline for the response to stereotactic radiosurgery therapy in brain metastases. Eur Radiol 33(12):8925–8935
DeVries DA et al (2023) Dual-center validation of using magnetic resonance imaging radiomics to predict stereotactic radiosurgery outcomes. Neurooncol Adv 5(1):vdad064
Mulford K et al (2021) A radiomics-based model for predicting local control of resected brain metastases receiving adjuvant SRS. Clin Translational Radiation Oncol 29:27–32
Chao ST et al (2018) Stereotactic radiosurgery in the management of limited (1–4) brain metasteses: systematic review and international stereotactic radiosurgery society practice guideline. Neurosurgery 83(3):345–353
Minniti G et al (2016) Single-fraction versus multifraction (3× 9 Gy) stereotactic radiosurgery for large (> 2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiation Oncology* Biology* Phys 95(4):1142–1148
Tsao M, Xu W, Sahgal A (2012) A meta-analysis evaluating stereotactic radiosurgery, whole‐brain radiotherapy, or both for patients presenting with a limited number of brain metastases. Cancer 118(9):2486–2493
Galldiks N et al (2020) Imaging challenges of immunotherapy and targeted therapy in patients with brain metastases: response, progression, and pseudoprogression. Neurooncology 22(1):17–30
Abouei Mehrizi MA et al (2023) The safety and efficacy of eCLIPs for treatment of wide-necked bifurcation aneurysms: a systematic review and Meta-analysis. World Neurosurg 180:213–223e7
Habibi MA et al (2022) The efficacy and safety of Rituximab in ANCA-Associated Vasculitis: a systematic review. Biology 11(12):1767
Paybast S, Habibi MA, Naser Moghadasi A (2023) Characteristics and management of multiple sclerosis patients during the Omicron era: is there a concern about the MS course in the face of the new variant of COVID-19? Neurol Sci 44(2):659–665
Karalis VD (2024) The Integration of Artificial Intelligence into Clinical Practice. Appl Biosci 3(1):14–44
Hofer IS et al (2020) Realistically integrating machine learning into clinical practice: a Road Map of opportunities, challenges, and a potential future. Anesth Analg 130(5):1115–1118
Ed-Driouch C et al (2022) Addressing the challenges and barriers to the Integration of Machine Learning into clinical practice: an innovative method to Hybrid Human–Machine Intelligence. Sensors 22(21):8313
Funding
There is no funding source with authors to declare.
Author information
Authors and Affiliations
Contributions
MA. H, F.R, and MS.M contributed to the study conception and design, and edited the manuscript. MA.H and A.H analyzed the data and wrote the first draft of the manuscript. E.M and MR.A collected data. MA.H and F.R made a critical revision of the manuscript. All authors commented on previous versions of the manuscript and revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study is deemed to exempt to received ethical approval.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Habibi, M.A., Rashidi, F., Habibzadeh, A. et al. Prediction of the treatment response and local failure of patients with brain metastasis treated with stereotactic radiosurgery using machine learning: A systematic review and meta-analysis. Neurosurg Rev 47, 199 (2024). https://doi.org/10.1007/s10143-024-02391-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-024-02391-3