Abstract
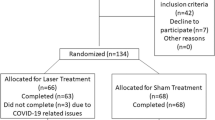
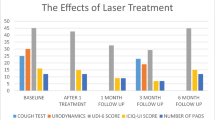
To evaluate the clinical efficacy of carbon dioxide laser in the treatment of female stress urinary incontinence and analyze the influencing factors. A total of 46 patients with stress urinary incontinence treated in the Affiliated Hospital of Nantong University from March 2021 to August 2022 were included through strict inclusion criteria and exclusion criteria. All patients were treated with transvaginal carbon dioxide laser therapy, and Patient Global Impression of Change (PGI-C) was used to evaluate patients’ subjective satisfaction after treatment. The efficacy was evaluated by patient’s subjective assessment of leakage, IngelmanSundberg scale, 1-h urine pad test, and international consultation on incontinence questionnaire short form (ICI-Q-SF) before and after treatment, and the adverse reactions after treatment were recorded. The treatment effect was divided into “significant effect group” and “no significant effect group” by subjective satisfaction and post-treatment-related scale evaluation. After laser treatment, patients’ subjective symptom improved, the volume of 1-h urine pad test was reduced, and the ICI-Q-SF score was decreased, and the differences were statistically significant (P < 0.05). There was no significant difference in IngelmanSundberg scale before and after treatment (P = 1.00). Multivariate logistic regression analysis showed that pad test volume was significantly correlated with treatment effect (P = 0.007). Transvaginal carbon dioxide laser is a safe and effective method for the treatment of mild to moderate stress urinary incontinence in females. The less severe the urinary leakage, the better the treatment effect.
Similar content being viewed by others
References
Imamura M, Abrams P, Bain C et al (2010) Systematic review and economic modelling of the effectiveness and cost-effectiveness of non-surgical treatments for women with stress urinary incontinence. Health Technol Assess 14(40):1–188, iii–iv. https://doi.org/10.3310/hta14400
Committee U (2018) Conservative management of urinary incontinence. J Obstet Gynaecol Can 40(2):e119–e125
Okeahialam NA, Dworzynski K, Jacklin P et al (2022) Prevention and non-surgical management of pelvic floor dysfunction: summary of NICE guidance. BMJ 376
Palos CC, Maturana AP, Ghersel FR et al (2018) Prospective and randomized clinical trial comparing transobturator versus retropubic sling in terms of efficacy and safety. Int Urogynecol J 29(1):29–35
deTayrac R, Deffieux X, Droupy S et al (2004) A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol 190(3):602–608
Wein AJ (2005) ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. J Urol 173(3):908–909
Gynecological Pelvic Floor Group of the Obstetrics and Gynecology Branch of the Chinese Medical Association. Guidelines for the diagnosis and treatment of female stress urinary incontinence (2017). Chinese J Obstet Gynecol, 52(05):289-293
Li FG, Maheux-Lacroix S, Deans R et al (2021) Effect of fractional carbon dioxide laser vs. sham treatment on symptom severity in women with postmenopausal vaginal symptoms: a randomized clinical trial. JAMA 326(14):1381–1389
Gao L, Wen W, Wang Y et al (2022) Fractional carbon dioxide laser improves vaginal laxity via remodeling of vaginal tissues in Asian women. J Clin Med 11(17):5201
Mothes AR, Runnebaum M, Runnebaum IB (2018) An innovative dual-phase protocol for pulsed ablative vaginal Erbium:YAG laser treatment of urogynecological symptoms. Eur J Obstet Gynecol Reprod Biol 229:167–171
Nalewczynska AA, Barwijuk M, Kolczewski P et al (2022) Pixel-CO2 laser for the treatment of stress urinary incontinence. Lasers Med Sci 37(2):1061–1067
Ruffolo AF, Casiraghi A, Marotta E et al (2021) Does the time of onset of urinary symptoms affect microablative fractional CO2 laser efficacy in postmenopausal women? Lasers Surg Med 53(7):953–959
Geisser ME, Clauw DJ, Strand V et al (2010) Contributions of change in clinical status parameters to Patient Global Impression of Change (PGIC) scores among persons with fibromyalgia treated with milnacipran. Pain 149(2):373–378
Schüssler B, Alloussi S (1983) Ingelman-Sundberg classification of stress incontinence. Gynakologische Rundschau 23(3):166
Palacios S, Ramirez M (2020) Efficacy of the use of fractional CO2RE intima laser treatment in stress and mixed urinary incontinence. Eur J Obstet Gynecol Reprod Biol 244:95–100
ElSheemy MS, Fathy H, Hussein HA et al (2015) Surgeon-tailored polypropylene mesh as a tension-free vaginal tape-obturator versus original TVT-O for the treatment of female stress urinary incontinence: a long-term comparative study. Int Urogynecol J 26(10):1533–1540
Abdel-Fattah M, Ramsay I, Pringle S et al (2011) Evaluation of transobturator tension-free vaginal tapes in management of women with recurrent stress urinary incontinence. Urology 77(5):1070–1075
Dietz HP, Hansell NK, Grace ME et al (2005) Bladder neck mobility is a heritable trait. BJOG 112(3):334–339
Ashton-Miller JA, Howard D, DeLancey JO (2001) The functional anatomy of the female pelvic floor and stress continence control system. Scand J Urol Nephrol Suppl 207:1–7
Turkoglu A, Coskun ADE, Arinkan SA et al (2022) The role of transperineal ultrasound in the evaluation of stress urinary incontinence cases. Int Braz J Urol 48(1):70–77
Chen HY, Huang YL, Hung YC et al (2006) Evaluation of stress urinary incontinence by computer-aided vector-based perineal ultrasound. Acta Obstet Gynecol Scand 85(10):1259–1264
Xiao T, Chen Y, Gan Y et al (2019) Can stress urinary incontinence be predicted by ultrasound? AJR Am J Roentgenol 213(5):1163–1169
González Isaza P, Jaguszewska K, Cardona JL et al (2018) Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J 29(2):211–215
Gaspar A, Brandi H, Gomez V et al (2017) Efficacy of Erbium:YAG laser treatment compared to topical estriol treatment for symptoms of genitourinary syndrome of menopause. Lasers Surg Med 49(2):160–168
Salvatore S, Leone Roberti Maggiore U et al (2015) Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause 22(8):845–849
Zhang L, Lai Y, Pan W et al (2021) Application of ultra pulse CO2 lattice laser in the treatment of female urinary incontinence. Transl Androl Urol 10(6):2471–2477
Dabaja H, Lauterbach R, Matanes E, Gruenwald I, Lowenstein L (2020) The safety and efficacy of CO2 laser in the treatment of stress urinary incontinence. Int Urogynecol J 31(8):1691–1696
Lauterbach R, Aharoni S, Justman N et al (2022) The efficacy and safety of a single maintenance laser treatment for stress urinary incontinence: a double-blinded randomized controlled trial. Int Urogynecol J 23:1–6
Mortensen OE, Christensen SE, Løkkegaard E (2022) The evidence behind the use of LASER for genitourinary syndrome of menopause, vulvovaginal atrophy, urinary incontinence and lichen sclerosus: a state-of-the-art review. Acta Obstet Gynecol Scand 101(6):657–692
Alexander JW, Karjalainen P, Ow LL et al (2022) CO2 surgical laser for treatment of stress urinary incontinence in women: a randomized controlled trial. Am J Obstet Gynecol 227(3):473.e1–473.e12
Fistonić I, Fistonić N (2018) Baseline ICIQ-UI score, body mass index, age, average birth weight, and perineometry duration as promising predictors of the short-term efficacy of Er:YAG laser treatment in stress urinary incontinent women: a prospective cohort study. Lasers Surg Med
Erel CT, Inan D, Mut A (2020) Predictive factors for the efficacy of Er:YAG laser treatment of urinary incontinence. Maturitas 132:1–6
Ogrinc UB, Sencar S, Lenasi H (2015) Novel minimally invasive laser treatment of urinary incontinence in women. Laser Surg Med 47:689–697
Ying T, Li Q, Xu L et al (2012) Three-dimensional ultrasound appearance of pelvic floor in nulliparous women and pelvic organ prolapse women. Int J Med Sci 9(10):894–900
Al-Saadi WI (2016) Transperineal ultrasonography in stress urinary incontinence: the significance of urethral rotation angles. Arab J Urol 14(1):66–71
Sendag F, Vidinli H, Kazandi M et al (2003) Role of perineal sonography in the evaluation of patients with stress urinary incontinence. Aust N Z J Obstet Gynaecol 43(1):54–57
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Approved by Ethics Committee of Affiliated Hospital of Nantong University
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Ye, Q. & Zhang, YQ. Effect evaluation and influencing factor analysis of vaginal carbon dioxide laser in the treatment of stress urinary incontinence. Lasers Med Sci 38, 153 (2023). https://doi.org/10.1007/s10103-023-03776-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03776-4