Abstract
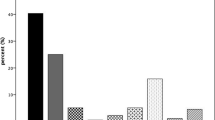
The study aims to determine whether 8 weeks of antibiotics is non-inferior to 12 weeks in patients with acute deep spinal implant infection (SII). In the retrospective study of all SII cases (2009–2016), patients aged ≥ 15 years with microbiologically confirmed SII treated with debridement and implant retention were included. Whenever possible, tailored antibiotic treatment was used: rifampin/linezolid in gram-positive and quinolones in gram-negative infection. Patients were divided into short treatment course (8 weeks, ST group) and extended treatment (12 weeks, ET group). Primary outcome measure was percentage of cures at 1-year follow-up. One-hundred-twenty-four patients considered, 48 excluded based on the above criteria, leaving 76 patients, 28 ST and 48 ET. There were no differences in patient age, comorbidities, underlying pathologies, infection location, or surgery characteristics between groups. Surgery-to-debridement time was similar (18.5-day ST vs. 19-day ET; P = 0.96). Sixteen SII cases (21.1%) occurred with bloodstream infection. Pathogens found were Enterobacteriaceae (35, 46.1%), Staphylococcus aureus (29, 38.2%), coagulase-negative staphylococci (12, 15.8%), Pseudomonas aeruginosa (12, 15.8%), and Enterococcus faecalis (7, 9.2%). Twenty seven (35.5%) had polymicrobial infection. E. faecalis was more frequent in the ST group (7, 25% vs. 0; P < 0.001), and P. aeruginosa in ET (1, 3.6% vs. 11, 22.9%; P = 0.05). Five patients died of causes unrelated to SII. At 1-year follow-up, cure rates (21/26 ST, 80.8% vs. 39/45 ET, 86.7%; P = 0.52) and recurrences (2/26, 7.7% vs. 2/45, 4.4%; P = 0.62) were similar. Eight-week antimicrobial courses were not inferior to 12 weeks in patients with acute deep SII treated with prompt debridement, proper wound healing, and optimized antibiotics.
Similar content being viewed by others
References
Pull Ter Gunne AF, Cohen DB (2009) Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976) 34(13):1422–1428
Kanafani ZA, Dakdouki GK, El-Dbouni O, Bawwab T, Kanj SS (2006) Surgical site infections following spinal surgery at a tertiary care center in Lebanon: incidence, microbiology, and risk factors. Scand J Infect Dis 38(8):589–592
Yeramaneni S, Robinson C, Hostin R (2016) Impact of spine surgery complications on costs associated with management of adult spinal deformity. Curr Rev Musculoskelet Med 9(3):327–332
Veeravagu A, Patil CG, Lad SP, Boakye M (2009) Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine (Phila Pa 1976) 34(17):1869–1872
Lazennec JY, Fourniols E, Lenoir T, Aubry A, Pissonnier ML, Issartel B et al (2011) Infections in the operated spine: update on risk management and therapeutic strategies. Orthop Traumatol Surg Res 97(6 SUPPL):S107–16
Núñez-Pereira S, Pellisé F, Rodríguez-Pardo D, Pigrau C, Bagó J, Villanueva C et al (2013) Implant survival after deep infection of an instrumented spinal fusion. Bone Joint J 95-B(8):1121–1126
Lall RR, Wong AP, Lall RR, Lawton CD, Smith ZA, Dahdaleh NS (2015) Evidence-based management of deep wound infection after spinal instrumentation. J Clin Neurosci 22(2):238–242
Bachy M, Bouyer B, Vialle R (2012) Infections after spinal correction and fusion for spinal deformities in childhood and adolescence. Int Orthop 36(2):465–469
Kowalski TJ, Berbari EF, Huddleston PM, Steckelberg JM, Mandrekar JN, Osmon DR (2007) The management and outcome of spinal implant infections: contemporary retrospective cohort study. Clin Infect Dis 44(7):913–920
Dubée V, Lenoir T, Leflon-Guibout V, Briere-Bellier C, Guigui P, Fantin B (2012) Three-month antibiotic therapy for early-onset postoperative spinal implant infections. Clin Infect Dis 55(11):1481–1487
Wille H, Dauchy FA, Desclaux A, Dutronc H, Vareil MO, Dubois V et al (2017) Efficacy of debridement, antibiotic therapy and implant retention within three months during postoperative instrumented spine infections. Infect Dis (Auckl) 49(4):261–267
Fernandez-Gerlinger M, Arvieu R, Lebeaux D, Rouis K, Guigui P, Mainardi J et al (2018) Successful six-week antibiotic treatment for early surgical-site infections in spinal surgery. Clin Infect Dis. https://doi.org/10.1093/cid/ciy805
Puhto AP, Puhto T, Syrjala H (2012) Short-course antibiotics for prosthetic joint infections treated with prosthesis retention. Clin Microbiol Infect 18(11):1143–1148
Lora-Tamayo J, Euba G, Cobo J, Horcajada JP, Soriano A, Sandoval E et al (2016) Short- versus long-duration levofloxacin plus rifampicin for acute staphylococcal prosthetic joint infection managed with implant retention: a randomised clinical trial. Int J Antimicrob Agents 48(3):310–316
Rodríguez-Pardo D, Pigrau C, Lora-Tamayo J, Soriano A, del Toro MD, Cobo J et al (2014) Gram-negative prosthetic joint infection: outcome of a debridement, antibiotics and implant retention approach. A large multicentre study. Clin Clin Microbiol Infect 20(11):O911–O919
Chen S-H, Lee C-H, Huang K-C, Hsieh P-H, Tsai S-Y (2015) Postoperative wound infection after posterior spinal instrumentation: analysis of long-term treatment outcomes. Eur Spine J 24(3):561–570
Ho C, Sucato DJ, Richards BS (2007) Risk factors for the development of delayed infections following posterior spinal fusion and instrumentation in adolescent idiopathic scoliosis patients. Spine (Phila Pa 1976) 32(20):2272–2277
Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J et al (2008) Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Jt Surg Am Vol [Internet] 90(1):62–69
Schuster JM, Rechtine G, Norvell DC, Dettori JR (2010) The influence of perioperative risk factors and therapeutic interventions on infection rates after spine surgery: a systematic review. Spine (Phila Pa 1976) 35(9 Suppl):S125–S137
Mikhael MM, Huddleston PM, Nassr A (2009) Postoperative culture positive surgical site infections after the use of irradiated allograft, nonirradiated allograft, or autograft for spinal fusion. Spine (Phila Pa 1976) 34(22):2466–2468
Donlan RM, Costerton JW (2002) Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 15(2):167–193
Haddad S, Núñez-Pereira S, Pigrau C, Rodríguez-Pardo D, Vila-Casademunt A, Alanay A et al (2018) The impact of deep surgical site infection on surgical outcomes after posterior adult spinal deformity surgery: a matched control study. Eur Spine J 27(10):2518–2528
Núñez-Pereira S, Pellisé F, Rodríguez-Pardo D, Pigrau C, Sánchez JM, Bagó J et al (2011) Individualized antibiotic prophylaxis reduces surgical site infections by gram-negative bacteria in instrumented spinal surgery. Eur Spine J 20(S3):397–402
Senneville E, Joulie D, Legout L, Valette M, Dezeque H, Beltrand E et al (2011) Outcome and predictors of treatment failure in Total hip/knee prosthetic joint infections due to Staphylococcus aureus. Clin Infect Dis 53(4):334–340
Lora-Tamayo J, Murillo O, Iribarren JA, Soriano A, Sánchez-Somolinos M, Baraia-Etxaburu JM et al (2013) A large multicenter study of methicillin-susceptible and methicillin-resistant Staphylococcus aureus prosthetic joint infections managed with implant retention. Clin Infect Dis 56(2):182–194
Fernandes A, Dias M (2013) The microbiological profiles of infected prosthetic implants with an emphasis on the organisms which form biofilms. J Clin Diagn Res 7(2):219–223
López-Sánchez C, Rodríguez-Pardo D, Pigrau C, Corona PS, Amat C, Lung M et al (2016) Teicoplanin—an old new treatment for enterococcal prosthetic joint infections. J Inf Secur 72(6):764–766
Hahn F, Zbinden R, Min K (2005) Late implant infections caused by Propionibacterium acnes in scoliosis surgery. Eur Spine J 14(8):783–788
Bémer P, Corvec S, Tariel S, Asseray N, Boutoille D, Langlois C et al (2008) Significance of Propionibacterium acnes-positive samples in spinal instrumentation. Spine (Phila Pa 1976) 33(26):E971–E976
Vilchez H, Campins A, Cobo J, Al E (2018) Prosthetic shoulder joint infection by Propionibacterium acnes. Presented in the ESCMID meeting in Madrid, Spain
Acknowledgments
We thank Celine Cavallo for the English language support.
Funding
This work was supported by Plan Nacional de I + D + i 2013–2016 and Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación cooperativa, Ministerio de Economía, Industria y Competitividad, Spanish Network for Research in Infectious Diseases (REIPI RD16/0016/0003)—cofinanced by European Development Regional Fund “A way to achieve Europe,” Operative program Intelligent Growth 2014–2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bosch-Nicolau, P., Rodríguez-Pardo, D., Pigrau, C. et al. Acute spinal implant infection treated with debridement: does extended antibiotic treatment improve the prognosis?. Eur J Clin Microbiol Infect Dis 38, 951–958 (2019). https://doi.org/10.1007/s10096-019-03537-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03537-8