Abstract
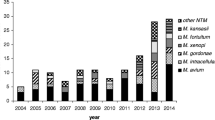
To determine trends in incidence and clinical relevance of rapidly growing mycobacteria (RGM) in a low-prevalence region of non-tuberculous mycobacteria. We retrospectively identified all patients with RGM-positive cultures between January 1994 and December 2015. Trends in incidence, clinical significance, and outcomes were assessed. One hundred and forty patients had RGM-positive cultures (116 respiratory and 24 extra-respiratory sources). The incidence of RGM isolates increased steadily from 2003 (0.34 per 100,000) to 2015 (1.73 per 100,000), with an average annual increase of 8.3%. Thirty-two patients (22.9%) had clinical disease, which trended to cluster in the second half of the study period. A positive acid-fast bacilli smear (odds ratio [OR] 97.7, 95 % CI 13.8–689.4), the presence of extra-respiratory isolates (OR 19.4, 95 % CI 5.2–72.7), and female gender (OR 5.9, 95 % CI 1.9–19.1) were independently associated with clinical disease. Cure rates were 73.3 and 87.5% for pulmonary and extra-pulmonary disease respectively. Although the burden of disease remains low, the presence of RGM isolates is increasing in our geographical setting. Whether this rise will be sustained over time and will coincide with an increase in clinical disease, or whether it is merely a cycle in the poorly understood epidemiological behaviour of environmental mycobacteria, will be seen in the near future.


Similar content being viewed by others
References
De Groote MA, Huitt G (2006) Infections due to rapidly growing mycobacteria. Clin Infect Dis 42:1756–1763
Winthrop KL, Mcnelley E, Kendall B, Marshall-Olson A, Morris C, Cassidy M, Saulson A, Hedberg K (2010) Pulmonary nontuberculous mycobacterial disease prevalence and clinical features: an emerging public health disease. Am J Respir Crit Care Med 182(7):977–982
Prevots DR, Shaw PA, Strickland D, Jackson LA, Raebel MA, Blosky MA et al (2010) Nontuberculous mycobacterial lung disease prevalence at four integrated health care delivery systems. Am J Respir Crit Care Med 182:970–976
Griffith DE (2010) It is better to light a candle…than to repeat the opinions of experts. Am J Respir Crit Care Med 182:865–866
Jarand J, Levin A, Zhang L, Huitt G, Mitchell JD, Daley CL (2011) Clinical and microbiologic outcomes in patients receiving treatment for Mycobacterium abscessus pulmonary disease. Clin Infect Dis 52:565–571
Moore JE, Kruijshaar ME, Ormerod LP, Drobniewski F, Abubakar I (2010) Increasing reports of non-tuberculous mycobacteria in England, Wales and Northern Ireland. BMC Public Health 10:612
Martin-Casabona N, Bahrmand AR, Bennedsen J, Thomsen VØ, Curcio M, Feldman K, Havelkova M et al (2004) Non-tuberculous mycobacteria: patterns of isolation. A multi-country retrospective survey. Int J Tuberc Lung Dis 8:1186–1193
Marras TK, Chedore P, Ying AM, Jamieson F (2007) Isolation prevalence of pulmonary non-tuberculous mycobacteria in Ontario, 1997–2003. Thorax 62:661–666
This official statement of the American Thoracic Society was approved by the Board of Directors, Medical Section of the American Lung Association (1997) Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am J Respir Crit Care Med 156:S1–S2
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F et al (2007) An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 175:367–416
Pfyffer GE (2015) Mycobacterium: general characteristics, laboratory detection, and staining procedures. In: Jorgensen J, Pfaller M, Carroll KC, Funke G, Landry ML, Richter SS, Warnock DW (eds) Manual of clinical microbiology, 11th edn. ASM Press, Washington, DC, pp 536–569
Simner PJ, Stenger S, Richter E, Brown-Elliott BA, Wallace RJ Jr, Wengenack NL (2015) Mycobacterium: laboratory characteristics of slowly growing mycobacteria. In: Jorgensen J, Pfaller M, Carroll KC, Funke G, Landry ML, Richter SS, Warnock DW (eds) Manual of clinical microbiology, 11th edn. ASM Press, Washington, DC, pp 570–594
Brown-Elliott BA, Wallace RJ Jr (2015) Mycobacterium: clinical and laboratory characteristics of rapidly growing mycobacteria. In: Jorgensen J, Pfaller M, Carroll KC, Funke G, Landry ML, Richter SS, Warnock DW (eds) Manual of clinical microbiology, 11th edn. ASM Press, Washington, DC, pp 595–612
Clinical and Laboratory Standards Institute (CLSI) (2011) Susceptibility testing of mycobacteria, nocardiae, and other aerobic actinomycetes; approved standard-second edition. CLSI document M24-A2. CLSI, Wayne, PA, USA
Marras TK, Mendelson D, Marchand-Austin A, May K, Jamieson FB (2013) Pulmonary nontuberculous mycobacterial disease, Ontario, Canada, 1998–2010. Emerg Infect Dis 19:1889–1891
van Ingen J, Bendien SA, de Lange WC, Hoefsloot W, Dekhuijzen PN, Boeree MJ, van Soolingen D (2009) Clinical relevance of non-tuberculous mycobacteria isolated in the Nijmegen–Arnhem region, The Netherlands. Thorax 64:502–506
Lai CC, Tan CK, Chou CH, Hsu HL, Liao CH, Huang YT, Yang PC, Luh KT, Hsueh PR (2010) Increasing incidence of nontuberculous mycobacteria, Taiwan, 2000–2008. Emerg Infect Dis 16:294–296
Wentworth AB, Drage LA, Wengenack NL, Wilson JW, Lohse CM (2013) Increased incidence of cutaneous nontuberculous mycobacterial infection, 1980 to 2009: a population-based study. Mayo Clin Proc 88:38–45
Alcaide F, Benítez MA, Escribà JM, Martín R (2000) Evaluation of the BACTEC MGIT 960 and the MB/BacT systems for recovery of mycobacteria from clinical specimens and for species identification by DNA AccuProbe. J Clin Microbiol 38(1):398–401
Cruciani M, Scarparo C, Malena M, Bosco O, Serpelloni G, Mengoli C (2004) Meta-analysis of BACTEC MGIT 960 and BACTEC 460 TB, with or without solid media, for detection of mycobacteria. J Clin Microbiol 42:2321–2325
Griffith DE, Girard WM, Wallace RJ Jr (1993) Clinical features of pulmonary disease caused by rapidly growing mycobacteria. An analysis of 154 patients. Am Rev Respir Dis 147:1271–1278
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare having no conflict of interest.
Ethical approval and informed consent
The ethical committee of the Bellvitge University Hospital approved the study (Ref.: PR130/14). Informed consent was not required due to the retrospective design of the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 89 kb)
Rights and permissions
About this article
Cite this article
Alcaide, F., Peña, M.J., Pérez-Risco, D. et al. Increasing isolation of rapidly growing mycobacteria in a low-incidence setting of environmental mycobacteria, 1994–2015. Eur J Clin Microbiol Infect Dis 36, 1425–1432 (2017). https://doi.org/10.1007/s10096-017-2949-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-2949-0