Abstract
Purpose
To analyze the characteristics of acute ischemic stroke (AIS) resulting from moyamoya disease (MMD) and intracranial large artery atherosclerotic stenosis (LAS).
Method
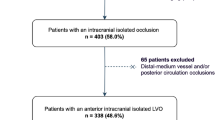
This real-world case control study enrolled imaging-confirmed AIS patients owing to MMD or LAS hospitalized from January 2015 through September 2020 consecutively. The features of risk factors, peripheral blood, and imaging presentations were compared between the two cohorts.
Results
A total of 191 eligible patients entered into final analysis, including 70 cases with MMD stroke and 121 with LAS stroke. LAS stroke vs. MMD stroke, the ratios of hyperlipidemia, hypertension, diabetes, and hyperhomocysteinemia were higher in the former (65.3 vs.12.9%, 65.3% vs. 4.3%, 39.7% vs. 2.9%, and 43.8% vs.12.9%; all p < 0.01) as well as baseline plasma arachidonic acid (AA) and adenosine diphosphate (ADP)-stimulated maximum platelet aggregation rates (75.3% vs. 60.8% and 73.1% vs.64.9%, respectively, all p < 0.01), which were positively correlated with triglycerides and cholesterol levels, blood glucose, age, and platelet counts (all p < 0.01). Classical watershed infarction (WSI) accounted for 87.14% in MMD stroke and 40.49% in LAS stroke, respectively (p < 0.01). Almost all of the patients with LAS showed plaques in arterial walls on CTA maps and non-homogeneous thickening with irregular luminal narrowing on HRMRI, while plaques were seldom found in MMD besides homogeneous thickening with regular luminal narrowing.
Conclusions
Differing from LAS stroke, MMD stroke mainly presents with WSI and does not feature with platelet hyper-aggregation and fragmentation of ulcer plaque. Whereby, focusing on perfusion improvement rather than antiplatelets and statins may be the predominant step in MMD-stroke correction.





Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AA%:
-
Arachidonic acid–induced platelet maximum aggregation rate
- ADP%:
-
Adenosine diphosphate–induced platelet maximum aggregation rate
- MMD:
-
Moyamoya disease
- RIC:
-
Remote ischemic conditioning
- WSI:
-
Watershed infarction
- TOAST:
-
Trial of org in acute stroke treatment
- DWI:
-
Diffusion-weighted imaging
- LAS:
-
Large artery atherosclerotic stenosis
- MRI:
-
Magnetic resonance imaging
- ICA:
-
Internal carotid artery
- MCA:
-
Middle cerebral artery
- ACA:
-
Anterior cerebral artery
- CTA:
-
Computed tomography angiography
- DSA:
-
Digital subtraction angiography
References
Gokcal E, Niftaliyev E, Asil T (2017) Etiological classification of ischemic stroke in young patients: a comparative study of TOAST, CCS, and ASCO. Acta Neurol Belg 117:643–648
McArdle PF, Kittner SJ, Ay H, Brown RJ, Meschia JF, Rundek T et al (2014) Agreement between TOAST and CCS ischemic stroke classification: the NINDS SiGN study. Neurology 83:1653–1660
Shang S, Zhou D, Ya J, Li S, Yang Q, Ding Y et al (2020) Progress in moyamoya disease. Neurosurg Rev 43:371–382
Kim DY, Son JP, Yeon JY, Kim GM, Kim JS, Hong SC et al (2017) Infarct pattern and collateral status in adult moyamoya disease: a multimodal magnetic resonance imaging study. Stroke 48:111–116
Suzuki J, Kodama N (1983) Moyamoya disease–a review. Stroke 14:104–109
Hashimoto N, Tominaga T, Miyamoto S, Nagata I, Houkin K, Suzuki N et al (2012) Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo) 52:245–266
Ding JY, Shang SL, Sun ZS, Asmaro K, Li WL, Yang Q et al (2020) Remote ischemic conditioning for the treatment of ischemic moyamoya disease. CNS Neurosci Ther 26:549–557
Onozuka D, Hagihara A, Nishimura K, Kada A, Nakagawara J, Ogasawara K et al (2016) Prehospital antiplatelet use and functional status on admission of patients with non-haemorrhagic moyamoya disease: a nationwide retrospective cohort study (J-ASPECT study). BMJ Open 6:e9942
Ferguson GG, Eliasziw M, Barr HW, Clagett GP, Barnes RW, Wallace MC et al (1999) The North American Symptomatic Carotid Endarterectomy Trial: surgical results in 1415 patients. Stroke 30:1751–1758
Banerjee C, Turan TN (2017) Large artery atherosclerosis: extracranial and intracranial. Semin Neurol 37:307–315
Mura M, Della SN, Long A, Chirico EN, Pialoux V, Millon A (2020) Carotid intraplaque haemorrhage: pathogenesis, histological classification, imaging methods and clinical value. Ann Transl Med 8:1273
Cumming MJ, Morrow IM (1994) Carotid artery stenosis: a prospective comparison of CT angiography and conventional angiography. AJR Am J Roentgenol 163:517–523
Barnett H, Taylor DW, Haynes RB, Sackett DL, Peerless SJ, Ferguson GG et al (1991) Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 325:445–453
Momjian-Mayor I, Baron JC (2005) The pathophysiology of watershed infarction in internal carotid artery disease: review of cerebral perfusion studies. Stroke 36:567–577
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K et al (2018) 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49:e46–e110
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Ya J, Zhou D, Ding J, Ding Y, Ji X, Yang Q et al (2020) High-resolution combined arterial spin labeling MR for identifying cerebral arterial stenosis induced by moyamoya disease or atherosclerosis. Ann Transl Med 8:87
van Geffen JP, Swieringa F, van Kuijk K, Tullemans B, Solari FA, Peng B et al (2020) Mild hyperlipidemia in mice aggravates platelet responsiveness in thrombus formation and exploration of platelet proteome and lipidome. Sci Rep 10:21407
Schoepe R, McQuillan S, Valsan D, Teehan G (2017) Atherosclerotic renal artery stenosis. Adv Exp Med Biol 956:209–213
Cazenave JP, Gachet C, Lanza F, Wiesel ML (2003) Platelets and arterial thrombosis. Bull Acad Natl Med 187(35–44):45–46
Pan Y, Elm JJ, Li H, Easton JD, Wang Y, Farrant M et al (2019) Outcomes associated with clopidogrel-aspirin use in minor stroke or transient ischemic attack. JAMA Neurology 76:1466–1473
Wang Y, Pan Y, Zhao X, Li H, Wang D, Johnston SC et al (2015) Clopidogrel with aspirin in acute minor stroke or transient ischemic attack (CHANCE) trial: one-year outcomes. Circulation 132:40–46
Wang X, Zhao X, Johnston SC, Xian Y, Hu B, Wang C et al (2015) Effect of clopidogrel with aspirin on functional outcome in TIA or minor stroke: CHANCE substudy. Neurology 85:573–579
Li XG, Ma N, Sun SS, Xu Z, Li W, Wang YJ et al (2017) Association of genetic variant and platelet function in patients undergoing neuroendovascular stenting. Postgrad Med J 93:555–559
Yang Y, Chen W, Pan Y, Yan H, Meng X, Liu L et al (2020) Effect of ticagrelor versus clopidogrel on platelet reactivity measured by thrombelastography in patients with minor stroke or TIA. Aging 12:20085–20094
Wang Y, Lin Y, Meng X, Chen W, Chen G, Wang Z et al (2017) Effect of ticagrelor with clopidogrel on high on-treatment platelet reactivity in acute stroke or transient ischemic attack (PRINCE) trial: Rationale and design. Int J Stroke 12:321–325
Kim JH, Bae HY, Kim SY (2013) Clinical marker of platelet hyperreactivity in diabetes mellitus. Diabetes Metab J 37:423–428
Boulet MM, Cheillan D, Di Filippo M, Buisson C, Michalski MC, Moulin P et al (2020) Large triglyceride-rich lipoproteins from fasting patients with type 2 diabetes activate platelets. Diabetes Metab 46:54–60
Chang BY, Kim DS, Kim SY (2020) Vitis labrusca Extract (HP01) Improves blood circulation and lipid metabolism in hyperlipidemic rats. Evid Based Complement Alternat Med 2020:6180310
Li HF, Zhang X, Zhang Y, Pan XD, Zhao HQ, Li H (2010) Clinical and neuroradiological features of internal watershed infarction and the occlusive diseases of carotid artery system. Neurol Res 32:1090–1096
Sarfo FS, Sarfo-Kantanka O, Adamu S, Obese V, Voeks J, Tagge R et al (2018) Stroke minimization through additive anti-atherosclerotic agents in routine treatment (SMAART): study protocol for a randomized controlled trial. Trials 19:181
Sarfo FS, Ovbiagele B (2017) Stroke minimization through additive anti-atherosclerotic agents in routine treatment (SMAART): a pilot trial concept for improving stroke outcomes in sub-Saharan Africa. J Neurol Sci 377:167–173
Acknowledgements
We would like to thank all patients and doctors who participated in this study for their cooperation.
Funding
This study was sponsored by the National Key R&D Program (2017YFC1308401), the National Natural Science Foundation (81660209, 81801143), and the Beijing Natural Science Foundation (7212047).
Author information
Authors and Affiliations
Contributions
(I) Conception and design: Zhiying Chen, Ran Meng. (II) Administrative support: Zhiying Chen, Da Zhou. (III) Provision of study materials: Zhiying Chen, Xiaoqin Wu. (IV) Collection and assembly of data. Zhiying Chen, Xiaoqin Wu, Shuling Shang. (V) Data analysis and interpretation: Zhiying Chen, Xiaoqin Wu. (VI) Manuscript writing: all authors.
(VII) Final approval of manuscript: all authors.
(VIII) The final version has been revised by Ran Meng, Yuchuan Ding, and Xunming Ji.
Corresponding author
Ethics declarations
Ethics approval
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Ethics Committee of Xuanwu Hospital, Capital Medical University, and all participants signed the consent forms before enrolment.
Consent for publication
Written informed consent was obtained from the patients’ parents and participants for publication of this case report and any accompanying images.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All subjects participating in the image acquisition signed the informed consent form.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Z., Wu, X., Zhou, D. et al. Characteristics of cerebral ischemic stroke based on moyamoya disease and atherosclerosis-associated intracranial arterial stenosis. Neurol Sci 43, 1087–1096 (2022). https://doi.org/10.1007/s10072-021-05359-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05359-z