Abstract
Background
Subcutaneous heparin at a prophylactic dose (SHPD) is a rather common treatment in ischemic stroke, but whether it confers an increased risk of hemorrhagic transformation of cerebral infarct (HT) and whether its reduction or discontinuation favors HT regression are presently poorly understood.
Methods
Two samples of ischemic stroke patients with a cerebral lesion diameter ≥ 3 cm on brain CT scan, admitted over 7 years to our stroke unit, were retrospectively examined: (1) patients treated or not treated with SHPD (enoxaparin 4000 U/day), with subsequent assessment of possible HT appearance (N = 267, mean age 75.9 ± 12.8 years) and (2) patients treated with SHPD, with HT and subsequent reduction/discontinuation or maintenance of the initial dose, and subsequent assessment of HT evolution (N = 116, mean age 75.7 ± 11.1 years). HT severity was quantified according to the ECASS study (HT score).
Results
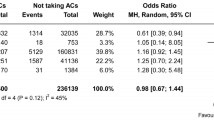
In the first sample, after adjustment for age, sex, stroke severity, cerebral lesion diameter, and other possible confounders, SHPD was inversely associated with HT appearance (hazard ratio 0.62, 95% CI 0.39–0.98, P = 0.04). In the second sample, after adjustment for age, sex, stroke severity, cerebral lesion diameter, and initial HT severity, SHPD reduction/discontinuation had an inverse effect on both HT score improvement (odds ratio 0.42, 95% CI 0.18–0.99, P = 0.049) and HT improvement according to neuroradiological reports (odds ratio 0.34, 95% CI 0.14–0.82, P = 0.015).
Conclusions
This retrospective study suggests that SHPD may play a protective role in HT appearance and evolution, which requires verification by a randomized clinical trial.
Similar content being viewed by others
References
Lindley RI, Wardlaw JM, Sandercock PA, Rimdusid P, Lewis SC, Signorini DF, Ricci S (2004) Frequency and risk factors for spontaneous hemorrhagic transformation of cerebral infarction. J Stroke Cerebrovasc Dis 13:235–246
Chen G, Wang A, Zhao X, Wang C, Liu L, Zheng H, Wang Y, Cao Y, Wang Y (2016) Frequency and risk factors of spontaneous hemorrhagic transformation following ischemic stroke on the initial brain CT or MRI: data from the China National Stroke Registry (CNSR). Neurol Res 38:538–544
Paciaroni M, Agnelli G, Corea F, Ageno W, Alberti A, Lanari A, Caso V, Micheli S, Bertolani L, Venti M, Palmerini F, Biagini S, Comi G, Previdi P, Silvestrelli G (2008) Early hemorrhagic transformation of brain infarction: rate, predictive factors, and influence on clinical outcome: results of a prospective multicenter study. Stroke 39:2249–2256
Toni D, Fiorelli M, Bastianello S, Sacchetti ML, Sette G, Argentino C, Montinaro E, Bozzao L (1996) Hemorrhagic transformation of brain infarct: predictability in the first 5 hours from stroke onset and influence on clinical outcome. Neurology 46:341–345
D'Amelio M, Terruso V, Famoso G, Di Benedetto N, Realmuto S, Valentino F, Ragonese P, Savettieri G, Aridon P (2014) Early and late mortality of spontaneous hemorrhagic transformation of ischemic stroke. J Stroke Cerebrovasc Dis 23:649–654
Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, Ringleb AP, Lorenzano S, Manelfe C, Bozzao L (1999) Hemorrhagic transformation within 36 hours of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke 30:2280–2284
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, ESC Scientific Document Group (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37:2893–2962
Muscari A, Faccioli L, Lega MV, Lorusso A, Masetti M, Pastore Trossello M, Puddu GM, Spinardi L, Zoli M (2020) Predicting hemorrhagic transformation and its timing from maximum cerebral lesion diameter in non-lacunar ischemic strokes. Brain Behav 10:e01497. https://doi.org/10.1002/brb3.1497
Paciaroni M, Agnelli G, Caso V, Corea F, Ageno W, Alberti A, Lanari A, Micheli S, Bertolani L, Venti M, Palmerini F, Billeci AM, Comi G, Previdi P, Silvestrelli G (2009) Acute hyperglycemia and early hemorrhagic transformation in ischemic stroke. Cerebrovasc Dis 28:119–123
Larrue V, von Kummer R, del Zoppo G, Bluhmki E (1997) Hemorrhagic transformation in acute ischemic stroke. Potential contributing factors in the European Cooperative Acute Stroke Study Stroke 28:957–960
Marsh EB, Llinas RH, Schneider AL, Hillis AE, Lawrence E, Dziedzic P, Gottesman-RF (2016) Predicting hemorrhagic transformation of acute ischemic stroke: prospective validation of the HeRS score. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000002430
Paciaroni M, Agnelli G, Falocci N, Caso V, Becattini C, Marcheselli S, Rueckert C, Pezzini A, Poli L, Padovani A, Csiba L, Szabó L, Sohn SI, Tassinari T, Abdul-Rahim AH, Michel P, Cordier M, Vanacker P, Remillard S, Alberti A, Venti M, Scoditti U, Denti L, Orlandi G, Chiti A, Gialdini G, Bovi P, Carletti M, Rigatelli A, Putaala J, Tatlisumak T, Masotti L, Lorenzini G, Tassi R, Guideri F, Martini G, Tsivgoulis G, Vadikolias K, Liantinioti C, Corea F, Del Sette M, Ageno W, De Lodovici ML, Bono G, Baldi A, D'Anna S, Sacco S, Carolei A, Tiseo C, Acciarresi M, D'Amore C, Imberti D, Zabzuni D, Doronin B, Volodina V, Consoli D, Galati F, Pieroni A, Toni D, Monaco S, Baronello MM, Barlinn K, Pallesen LP, Kepplinger J, Bodechtel U, Gerber J, Deleu D, Melikyan G, Ibrahim F, Akhtar N, Mosconi MG, Bubba V, Silvestri I, Lees KR (2015) Early recurrence and cerebral bleeding in patients with acute ischemic stroke and atrial fibrillation: effect of anticoagulation and its timing: the RAF study. Stroke 46:2175–2182
Dennis M, Caso V, Kappelle LJ, Pavlovic A, Sandercock P, European Stroke Organisation (2016) European Stroke Organisation (ESO) guidelines for prophylaxis for venous thromboembolism in immobile patients with acute ischaemic stroke. Eur Stroke J 1:6–19
ISO-SPREAD Stroke Prevention And Educational Awareness Diffusion, VIII Edition (2016) www.iso-spread.it. Accessed 20 March 2020
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50:e344–e418
International Stroke Trial Collaborative Group (1997) The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. Lancet 349:1569–1581
Adams HP, Woolson RF, Helgason C, Karanjia PN, Gordon DL (1998) Low molecular weight heparinoid, ORG 10172 (Danaparoid), and outcome after acute ischemic stroke. A randomized controlled trial JAMA 279:1265–1272
Bath PMW, Lindenstrom E, Boysen G, De Deyn P, Friis P, Leys D, Marttila R, Olsson J-E, O’Neill D, Orgogozo J-M, Ringelstein B, van der Sande JJ, Turpie AGG, Investigators TAIST (2001) Tinzaparin in acute ischamic stroke (TAIST): a randomised aspirin-controlled trial. Lancet 358:702–710
Wong KS, Chen C, Ng PW, Tsoi TH, Li HL, Fong WC, Yeung J, Wong CK, Yip KK, Gao H, Wong HB, for the FISS-tris Study Investigators (2007) Low-molecular-weight heparin compared with aspirin for the treatment of acute ischaemic stroke in Asian patients with large artery occlusive disease: a randomised study. Lancet Neurol 6:407–413
Bath PMW, Iddenden R, Bath FJ (2000) Low-molecular-weight heparins and heparinoids in acute ischemic stroke. A meta-analysis of randomized controlled trials. Stroke 31:1770–1778
Paciaroni M, Agnelli G, Micheli S, Caso V (2007) Efficacy and safety of anticoagulant treatment in acute cardioembolic stroke. A meta-analysis of randomized controlled trials. Stroke 38:423–430
Whiteley WN, Adams HP Jr, Bath PMW, Berge E, Sandset PM, Dennis M, Murray GD, Wong KSL, Sandercock PAG (2013) Targeted use of heparin, heparinoids, or low-molecular-weight heparin to improve outcome after acute ischaemic stroke: an individual patient data meta-analysis of randomised controlled trials. Lancet Neurol 12:539–545
Mocco J, Shelton CE, Sergot P, Ducruet AF, Komotar RJ, Otten ML, Sosunov SA, Macarthur RB, Kennedy TP, Connolly ES Jr (2007) O-desulfated heparin improves outcome after rat cerebral ischemia/reperfusion injury. Neurosurgery 61:1297–1303
Zhang ZG, Sun X, Zhang QZ, Yang H (2013) Neuroprotective effects of ultra-low-molecular-weight heparin on cerebral ischemia/reperfusion injury in rats: involvement of apoptosis, inflammatory reaction and energy metabolism. Int J Mol Sci 14:1932–1939
Nordling S, Hong J, Fromell K, Edin F, Brännström J, Larsson R, Nilsson B, Magnusson PU (2015) Vascular repair utilising immobilised heparin conjugate for protection against early activation of inflammation and coagulation. Thromb Haemost 113:1312–1322
Lyden P, Lu M, Jackson C, Marler J, Kothari R, Brott T, Zivin J (1999) Underlying structure of the National Institutes of Health Stroke Scale: results of a factor analysis. NINDS tPA Stroke Trial Investigators. Stroke 30:2347–2354
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C (1991) Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 337:1521–1526
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Rankin J (1957) Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J 2:200–215
Muscari A, Faccioli L, Lega MV, Lorusso A, Trossello MP, Puddu GM, Spinardi L, Zoli M (2019) Predicting cerebral edema in ischemic stroke patients. Neurol Sci 40:745–752
Kay R, Wong KS, Yu YL, Chan YW, Tsoi TH, Ahuja AT, Chan FL, Fong KY, Law CB, Wong A (1995) Low-molecular-weight heparin for the treatment of acute ischemic stroke. N Engl J Med 333:1588–1593
England TJ, Bath PM, Sare GM, Geeganage C, Moulin T, O'Neill D, Woimant F, Christensen H, De Deyn P, Leys D, Ringelstein EB, Investigators TAIST (2010) Asymptomatic hemorrhagic transformation of infarction and its relationship with functional outcome and stroke subtype: assessment from the Tinzaparin in Acute Ischaemic Stroke Trial. Stroke 41:2834–2839
Lin K, Kazmi KS, Law M, Babb J, Peccerelli N, Pramanik BK (2007) Measuring elevated microvascular permeability and predicting hemorrhagic transformation in acute ischemic stroke using first-pass dynamic perfusion CT imaging. Am J Neuroradiol 28:1292–1298
Kim T, Koo J, Kim SH, Song IU, Chung SW, Lee KS (2018) Blood-brain barrier permeability assessed by perfusion computed tomography predicts hemorrhagic transformation in acute reperfusion therapy. Neurol Sci 39:1579–1584
Rossi DJ, Brady JD, Mohr C (2007) Astrocyte metabolism and signaling during brain ischemia. Nat Neurosci 10:1377–1386
László JM, Hortobágyi T (2017) Hemorrhagic transformation of ischemic stroke - pathogenesis and pathophysiology. Vasc Dis Ther 2:1–25
Kulik T, Kusano Y, Aronhime S, Sandler AL, Winn HR (2008) Regulation of cerebral vasculature in normal and ischemic brain. Neuropharmacology 55:281–288
Spencer JL, Stone PJ, Nugent MA (2006) New insights into the inhibition of human neutrophil elastase by heparin. Biochemistry 45:9104–9120
Li L, Ling Y, Huang M, Yin T, Gou S-M, Zhan N-Y, Xiong J-X, Wu H-S, Yang Z-Y, Wang C-Y (2015) Heparin inhibits the inflammatory response induced by LPS and HMGB1 by blocking the binding off HGMB1 to the surface of macrophages. Cytokine 72:36–42
Medeiros GF, Mendes A, Castro RAB, Baú EC, Nader HB, Dietrich CP (2000) Distribution of sulfated glycosaminoglycans in the animal kingdom: widespread occurrence of heparin-like compounds in invertebrates. Biochim Biophys Acta 1475:287–294
Hayman EG, Patel AP, James RF, Simard JM (2017) Heparin and heparin-derivatives in post-subarachnoid hemorrhage brain injury: a multimodal therapy for a multimodal disease. Molecules 22. https://doi.org/10.3390/molecules22050724
Nelson RM, Cecconi O, Roberts WG, Aruffo A, Linhardt RJ, Bevilacqua MP (1993) Heparin oligosaccharides bind L- and P-selectin and inhibit acute inflammation. Blood 82:3253–3258
Sandström J, Carlsson L, Marklund SL, Edlund T (1992) The heparin-binding domain of extracellular superoxide dismutase C and formation of variants with reduced heparin affinity. J Biol Chem 267:18205–18209
Li PA, He QP, Siddiqui MM, Shuaib A (1998) Posttreatment with low molecular weight heparin reduces brain edema and infarct volume in rats subjected to thrombotic middle cerebral artery occlusion. Brain Res 801:220–223
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Because of the retrospective nature of this study, which included several patients who died after stroke, written informed consent could not be obtained. However, the utilization of the data derived from medical records for the present study was approved by our joint university-hospital Ethics Committee (Comitato Etico di Area Vasta Emilia Centro), and the study was conducted in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muscari, A., Bartoli, E., Faccioli, L. et al. Venous thromboembolism prevention with low molecular weight heparin may reduce hemorrhagic transformation in acute ischemic stroke. Neurol Sci 41, 2485–2494 (2020). https://doi.org/10.1007/s10072-020-04354-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04354-0