Abstract
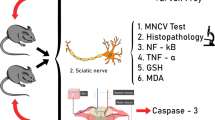
Vincristine (VCR) is a well-known anticancer drug which frequently induced painful neuropathy and impairs the quality of life of patients. The present study was designed to investigate the alleviative potential of a novel cyclohexenone derivative (CHD), i.e., ethyl 6-(4-methoxyphenyl)-2-oxo-4-phenylcyclohexe-3-enecarboxylate, against VCR-induced neuropathic pain in mice model. VCR was administered intraperitoneally for 10 days in two cycles to induce neuropathic pain. Static and dynamic mechanical allodynia was evaluated using von Frey hair filaments and cotton buds, respectively. Paw thermal hyperalgesia was determined through a hot plate analgesiometer. The tail cold immersion hyperalgesia and paw cold allodynia were determined by available standard protocols. The formalin nociception was induced via subplantar injection of formalin. The antioxidant potential was evaluated via 2,2-diphenyl-1-picrylhydrazyl free radical scavenging activity. The outcome of this study revealed that CHD (30–45 mg/kg) and gabapentin (75 mg/kg) significantly enhanced the paw withdrawal threshold (PWT) and paw withdrawal latency (PWL) in static and dynamic allodynia, respectively, and increased the PWL in thermal hyperalgesia and tail withdrawal latency (TWL) as compared to the VCR-treated group. CHD significantly augmented the paw withdrawal duration (PWD) in paw cold allodynia, while the same compound only increased the paw elevation and paw licking in the delayed phase of formalin nociception. Moreover, CHD significantly inhibited the DPPH free radical scavenging action (IC50 = 56), butylated hydroxytoluene (BHT) (IC50 = 39), and ascorbic acid (IC50 = 2.93). In conclusion, CHD exhibited a profile of potential attenuative effect against the VCR-induced neuropathic pain which might be attributed to its possible antinociceptive and antioxidant effect.









Similar content being viewed by others
References
Merskey H (1986) Classification of chronic pain: description of chronic pain syndromes and definitions of pain terms. Pain 3:216–221
Rasmussen PV, Sindrup SH, Jensen TS, Bach FW (2004) Symptoms and signs in patients with suspected neuropathic pain. Pain 110:461–469
Woolf CJ, Mannion RJ (1999) Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet 353:1959–1964. https://doi.org/10.1016/S0140-6736(99)01307-0
Poupon P, Monlun M, Alexandre L, Blanco L, Rigalleau V (2018) Sudomotor function in diabetic peripheral artery disease: a role for diabetic neuropathy? Neurol Sci 39:191–192. https://doi.org/10.1007/s10072-017-3103-6
Cazzato D, Dalla Bella E, Saveri P, Taroni F, Marucci G, Lauria G (2019) Late-onset and fast progressive neuropathy and cardiomyopathy in Val32Ala transthyretin gene mutation. Neurol Sci:1–3. https://doi.org/10.1007/s10072-019-3716-z
Ali G, Subhan F, Abbas M, Zeb J, Shahid M, Sewell RD (2015) A streptozotocin-induced diabetic neuropathic pain model for static or dynamic mechanical allodynia and vulvodynia: validation using topical and systemic gabapentin. Naunyn Schmiedeberg's Arch Pharmacol 388:1129–1140. https://doi.org/10.1007/s00210-015-1145-y
Gutiérrez-Gutiérrez G, Sereno M, Miralles A, Casado-Sáenz E, Gutiérrez-Rivas E (2010) Chemotherapy-induced peripheral neuropathy: clinical features, diagnosis, prevention and treatment strategies. Clin Transl Oncol 12:81–91. https://doi.org/10.1007/S12094-010-0474-z
Ito T, Mochida A, Saito K, Nishi K, Sasaki S, Hisada T, Morinari H, Nakahara K, Tahara M, Masuda S (2002) An autopsy case of pulmonary and central nervous system metastatic osteosarcoma treated with thirty-six courses of chemotherapy over four years. Nihon Kokyuki Gakkai zasshi 40:71–76
Bromberg M (2000) Peripheral neurotoxic disorders. Clin Neurobehav Toxicol 18:681–689
Tanner KD, Levine JD, Topp KS (1998) Microtubule disorientation and axonal swelling in unmyelinated sensory axons during vincristine-induced painful neuropathy in rat. J Comp Neurol 395:481–492. https://doi.org/10.1002/(SICI)1096-9861(19980615)395:4<481::AID-CNE5>3.0.CO;2-Y
Tanner KD, Reichling DB, Levine JD (1998) Nociceptor hyper-responsiveness during vincristine-induced painful peripheral neuropathy in the rat. J Neurosci 18:6480–6491. https://doi.org/10.1523/JNEUROSCI.18-16-06480.1998
Topp KS, Tanner KD, Levine JD (2000) Damage to the cytoskeleton of large diameter sensory neurons and myelinated axons in vincristine-induced painful peripheral neuropathy in the rat. J Comp Neurol 424:563–576. https://doi.org/10.1002/1096-9861(20000904)424:4<563::AID-CNE1>3.0.CO;2-U
Aley K, Reichling D, Levine J (1996) Vincristine hyperalgesia in the rat: a model of painful vincristine neuropathy in humans. Neuroscience 73:259–265. https://doi.org/10.1016/0306-4522(96)00020-6
Nozaki-Taguchi N, Chaplan SR, Higuera ES, Ajakwe RC, Yaksh TL (2001) Vincristine-induced allodynia in the rat. Pain 93:69–76. https://doi.org/10.1016/S0304-3959(01)00294-9
Authier N, Gillet J-P, Fialip J, Eschalier A, Coudore F (2003) A new animal model of vincristine-induced nociceptive peripheral neuropathy. Neurotoxicology 24:797–805. https://doi.org/10.1016/S0161-813X(03)00043-3
Jaggi AS, Singh N (2010) Differential effect of spironolactone in chronic constriction injury and vincristine-induced neuropathic pain in rats. Eur J Pharmacol 648:102–109. https://doi.org/10.1016/j.ejphar.2010.08.050
Muthuraman A, Jaggi AS, Singh N, Singh D (2008) Ameliorative effects of amiloride and pralidoxime in chronic constriction injury and vincristine induced painful neuropathy in rats. Eur J Pharmacol 587:104–111. https://doi.org/10.1016/j.ejphar.2008.03.042
Dworkin RH, O’connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, Kent JL, Krane EJ, LeBel AA, Levy RM (2010) Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. In: Mayo Clin Proc. Elsevier, pp S3-S14. https://doi.org/10.4065/mcp.2009.0649
Lee JNP (2010) Improving the management of neuropathic pain. Practioner 254:27–30
Wiffen PJ, Collins S, McQuay HJ, Carroll D, Jadad A, Moore RA (2010) WITHDRAWN. Anticonvulsant drugs for acute and chronic pain. Cochrane Database Syst Rev 1:CD001133–CD001133. https://doi.org/10.1002/14651858.CD001133.pub3
Wamboldt C, Kapustin J (2006) Evidence-based treatment of diabetic peripheral neuropathy. J Nurse Pract 2:370–378. https://doi.org/10.1016/j.nurpra.2006.04.015
Senguttuvan S, Nagarajan S (2010) Synthesis of 2-amino-5-aryl-5,6-dihydro-7-(naphthalen-2-yl)quinazolin-4-ols. Int J Chem 2:108
Gopalakrishnan M, Thanusu J, Kanagarajan V (2008) Synthesis and characterization of 4,6-diaryl-4,5-dihydro-2H-indazol-3-ols and 4,6-diaryl-2-phenyl-4,5-dihydro-2H-indazol-3-ols—a new series of fused indazole derivatives. Chem Heterocycl Comp 44:950–955. https://doi.org/10.1007/s10593-008-0137-y
Johnson T, Pultar F, Menke F, Lautens M (2016) Palladium-catalyzed α-arylation of vinylogous esters for the synthesis of γ, γ-disubstituted cyclohexenones. Org Lett 18:6488–6491. https://doi.org/10.1021/acs.orglett.6b03394
Liu D, Yu W, Li J, Pang C, Zhao L (2013) Novel 2-(E)-substituted benzylidene-6-(N-substituted aminomethyl) cyclohexanones and cyclohexanols as analgesic and anti-inflammatory agents. Med Chem Res 22:3779–3786. https://doi.org/10.1007/s00044-012-0362-x
Wang Y, Yu C, Pan Y, Li J, Zhang Y, Ye F, Yang S, Zhang H, Li X, Liang G (2011) A novel compound C12 inhibits inflammatory cytokine production and protects from inflammatory injury in vivo. PLoS One 6:e24377. https://doi.org/10.1371/journal.pone.0024377
Sheorey R, Thangathiruppathy A, Alagarsamy V (2016) Synthesis and pharmacological evaluation of 3-propyl-2-substitutedamino-3H-quinazolin-4-ones as analgesic and anti-inflammatory agents. J Heterocycl Chem 53:1371–1377. https://doi.org/10.1002/jhet.1973
Lednicer D, Von Voigtlander PF, Emmert DE (1981) 4-Aryl-4-aminocyclohexanones and their derivatives, a novel class of analgesics. 3. M-hydroxyphenyl derivatives. J Med Chem 24:341–346. https://doi.org/10.1021/jm00135a019
Lednicer D, VonVoigtlander PF, Emmert DE (1981) 4-Amino-4-arylcyclohexanones and their derivatives: a novel class of analgesics. 2. Modification of the carbonyl function. J Med Chem 24:404–408. https://doi.org/10.1021/jm00136a010
Ming-Tatt L, Khalivulla SI, Akhtar MN, Lajis N, Perimal EK, Akira A, Ali DI, Sulaiman MR (2013) Anti-hyperalgesic effect of a benzilidine-cyclohexanone analogue on a mouse model of chronic constriction injury-induced neuropathic pain: participation of the κ-opioid receptor and KATP. Pharmacol Biochem Behav 114:58–63. https://doi.org/10.1016/j.pbb.2013.10.019
Ahmadi A, Khalili M, Hajikhani R, Hosseini H, Afshin N, Nahri-Niknafs B (2012) Synthesis and study the analgesic effects of new analogues of ketamine on female Wistar rats. Med Chem 8:246–251. https://doi.org/10.2174/157340612800493683
Ming-Tatt L, Khalivulla SI, Akhtar MN, Mohamad AS, Perimal EK, Khalid MH, Akira A, Lajis N, Israf DA, Sulaiman MR (2012) Antinociceptive activity of a synthetic curcuminoid analogue, 2,6-bis-(4-hydroxy-3-methoxybenzylidene) cyclohexanone, on nociception-induced models in mice. Basic Clin Pharmacol Toxicol 110:275–282. https://doi.org/10.1111/j.1742-7843.2011.00804.x
Weng H-R, Cordella J, Dougherty P (2003) Changes in sensory processing in the spinal dorsal horn accompany vincristine-induced hyperalgesia and allodynia. Pain 103:131–138
Siau C, Bennett GJ (2006) Dysregulation of cellular calcium homeostasis in chemotherapy-evoked painful peripheral neuropathy. Anesth Analg 102:1485–1490. https://doi.org/10.1213/01.ane.0000204318.35194.ed
Chaplan S, Bach F, Pogrel J, Chung J, Yaksh T (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53:55–63
Field MJ, McCleary S, Hughes J, Singh L (1999) Gabapentin and pregabalin, but not morphine and amitriptyline, block both static and dynamic components of mechanical allodynia induced by streptozocin in the rat. Pain 80:391–398
Nakazato-Imasato E, Tanimoto-Mori S, Kurebayashi Y (2009) Effect of mexiletine on dynamic allodynia induced by chronic constriction injury of the sciatic nerve in rats. J Vet Med Sci 71:991–994
Ahmad N, Subhan F, Islam NU, Shahid M, Rahman FU, Sewell RD (2017) Gabapentin and its salicylaldehyde derivative alleviate allodynia and hypoalgesia in a cisplatin-induced neuropathic pain model. Eur J Pharmacol 814:302–312. https://doi.org/10.1016/j.ejphar.2017.08.040
Necker R, Hellon R (1977) Noxious thermal input from the rat tail: modulation by descending inhibitory influences. Pain 4:231–242
Decosterd I, Woolf CJ (2000) Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain 87:149–158
Geisler S, Doan RA, Strickland A, Huang X, Milbrandt J, DiAntonio A (2016) Prevention of vincristine-induced peripheral neuropathy by genetic deletion of SARM1 in mice. Brain 139:3092–3108. https://doi.org/10.1093/brain/aww251
Abad ANA, Nouri MHK, Tavakkoli F (2011) Effect of Salvia officinalis hydroalcoholic extract on vincristine-induced neuropathy in mice. Chin J Nat Med 9:354–358. https://doi.org/10.3724/SP.J.1009.2011.00354
Samshuddin S, Narayana B, Sarojini BK, Madhu LN (2013) A study on the reactions of alkyl 4,6-bis (4-fluorophenyl)-2-oxocyclohex-3-ene-1-carboxylate and in vitro antioxidant activity of derivatives. Med Chem Res 22:3002–3011. https://doi.org/10.1007/s00044-012-0304-7
Cata J, Weng H, Lee B, Reuben J, Dougherty P (2006) Clinical and experimental findings in humans and animals with chemotherapy-induced peripheral neuropathy. Minerva Anestesiol 72:151
Linglu D, Yuxiang L, Yaqiong X, Ru Z, Lin M, Shaoju J, Juan D, Tao S, Jianqiang Y (2014) Antinociceptive effect of matrine on vincristine-induced neuropathic pain model in mice. Neurol Sci 35:815–821. https://doi.org/10.1007/s10072-013-1603-6
Hur W, Chung JY, Choi PK, Kang HG (2019) Uremia presented as acute cranial neuropathy. Neurol Sci:1–3. https://doi.org/10.1007/s10072-019-03741-6
Vitet L, Patte-Mensah C, Boujedaini N, Mensah-Nyagan A-G, Meyer L (2018) Beneficial effects of Gelsemium-based treatment against paclitaxel-induced painful symptoms. Neurol Sci 39:2183–2196. https://doi.org/10.1007/s10072-018-3575-z
Jaggi AS, Jain V, Singh N (2011) Animal models of neuropathic pain. Fundam Clin Pharmacol 25:1–28. https://doi.org/10.1111/j.1472-8206.2009.00801.x
Villani F, Busia A, Villani M, Vismara C, Viviani S, Bonfante V (2008) Serum cytokine in response to chemo-radiotherapy for Hodgkin’s disease. Tumori 94:803–808
Starobova H, Vetter I (2017) Pathophysiology of chemotherapy-induced peripheral neuropathy. Front Mol Neurosci 10:174. https://doi.org/10.3389/fnmol.2017.00174
Grisold W, Cavaletti G, Windebank AJ (2012) Peripheral neuropathies from chemotherapeutics and targeted agents: diagnosis, treatment, and prevention. Neuro Oncol 14:iv45–iv54. https://doi.org/10.1093/neuonc/nos203
Jaggi AS, Singh N (2012) Mechanisms in cancer-chemotherapeutic drugs-induced peripheral neuropathy. Toxicology 291:1–9. https://doi.org/10.1016/j.tox.2011.10.019
Meyer L, Patte-Mensah C, Taleb O, Mensah-Nyagan AG (2010) Cellular and functional evidence for a protective action of neurosteroids against vincristine chemotherapy-induced painful neuropathy. Cell Mol Life Sci 67:3017–3034. https://doi.org/10.1007/s00018-010-0372-0
Dworkin RH, O’connor AB, Backonja M, Farrar JT, Finnerup NB, Jensen TS, Kalso EA, Loeser JD, Miaskowski C, Nurmikko TJ (2007) Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain 132(3):237–251
Mora E, Smith EML, Donohoe C, Hertz DL (2016) Vincristine-induced peripheral neuropathy in pediatric cancer patients. Am J Cancer Res 6:2416
Lynch JJ III, Wade CL, Zhong CM, Mikusa JP, Honore P (2004) Attenuation of mechanical allodynia by clinically utilized drugs in a rat chemotherapy-induced neuropathic pain model. Pain 110(1–2):56–63
Flatters SJ, Bennett GJ (2004) Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain 109:150–161. https://doi.org/10.1016/j.pain.2004.01.029
Bhalla S, Singh N, Jaggi AS (2015) Dose-related neuropathic and anti-neuropathic effects of simvastatin in vincristine-induced neuropathic pain in rats. Food Chem Toxicol 80:32–40. https://doi.org/10.1016/j.fct.2015.02.016
Bang S, Kim YS, Jeong SR (2016) Anti-allodynic effect of theoesberiven F in a vincristine-induced neuropathy model. Exp Ther Med 12:799–803. https://doi.org/10.3892/etm.2016.3396
Geis C, Beyreuther BK, Stöhr T, Sommer C (2011) Lacosamide has protective disease modifying properties in experimental vincristine neuropathy. Neuropharmacology 61:600–607. https://doi.org/10.1016/j.neuropharm.2011.05.001
Xiao WH, Bennett GJ (2008) Chemotherapy-evoked neuropathic pain: abnormal spontaneous discharge in A-fiber and C-fiber primary afferent neurons and its suppression by acetyl-L-carnitine. Pain 135:262–270. https://doi.org/10.1016/j.pain.2007.06.001
Mika J, Zychowska M, Popiolek-Barczyk K, Rojewska E, Przewlocka B (2013) Importance of glial activation in neuropathic pain. Eur J Pharmacol 716:106–119. https://doi.org/10.1016/j.ejphar.2013.01.072
Carozzi V, Canta A, Chiorazzi A (2015) Chemotherapy-induced peripheral neuropathy: what do we know about mechanisms? Neurosci Lett 596:90–107. https://doi.org/10.1016/j.neulet.2014.10.014
Sisignano M, Baron R, Scholich K, Geisslinger G (2014) Mechanism-based treatment for chemotherapy-induced peripheral neuropathic pain. Nat Rev Neurol 10:694–707. https://doi.org/10.1038/nrneurol.2014.211
Miyagawa M, Watanabe T, Saito M, Luu B, Yamada M, Suzuki H (2010) Use of cyclohexenone derivatives in the manufacture of a medicament for treating diabetic complications. Google Patents
Yoshizawa T, Hayashi Y, Yoshida A, Ito Y, Yamada S, Takahashi S (2012) 107 therapeutic effects of the cyclohexenone derivative tac-302 on the bladder dysfunction in streptozotocin (STZ)-induced diabetic rats. J Urol 187:e43. https://doi.org/10.1016/j.juro.2012.02.155
Ashalatha B, Narayana B, Vijaya Raj K (2009) Synthesis and characterization of some novel 3-bromo-2-acetylthiophene chalcones and biological evaluation of their ethyl-4-(3-bromothien-2-yl)-2-oxo-6-(aryl) cyclohex-3-ene-1-carboxylate derivatives. Phosphorus Sulfur Silicon Relat Elem 184:1904–1919. https://doi.org/10.1080/10426500802414189
Kato T, Ishii H, Kawai K, Sawa Y (1984) Synthesis and analgesic activity of cyclohexenylmethylamines and related compounds. Chem Pharm Bull 32:2279–2289
Yaouba S, Koch A, Guantai EM, Derese S, Irungu B, Heydenreich M, Yenesew A (2018) Alkenyl cyclohexanone derivatives from Lannea rivae and Lannea schweinfurthii. Phytochem Lett 23:141–148. https://doi.org/10.1016/j.phytol.2017.12.001
Fujioka H, Kotoku N, Sawama Y, Nagatomi Y, Kita Y (2002) Concise asymmetric synthesis of a model compound, (4S,5S,6S)-6-(2,2-dimethoxy)ethyl-4,5-epoxy-6-hydroxy-2-cyclohexenone, for the cyclohexenone core of scyphostatin. Tetrahedron Lett 43:4825–4828. https://doi.org/10.1016/S0040-4039(02)00916-4
Hoye TR, Tennakoon MA (2000) Synthesis (and alternative proof of configuration) of the scyphostatin C (1’)-C(20’) trienoyl fragment. Organic Lett 2:1481–1483. https://doi.org/10.1021/ol0058386
Lopes L, Pereira S, Silva L, Figueiredo K, Moura B, Almeida F, Sousa F (2009) Antinociceptive effect of topiramate in models of acute pain and diabetic neuropathy in rodents. Life Sci 84:105–110. https://doi.org/10.1016/j.lfs.2008.11.005
Ranjithkumar R, Prathab Balaji S, Balaji B, Ramesh R, Ramanathan M (2013) Standardized aqueous Tribulus terristris (Nerunjil) extract attenuates hyperalgesia in experimentally induced diabetic neuropathic pain model: role of oxidative stress and inflammatory mediators. Phytother Res 27:1646–1657. https://doi.org/10.1002/ptr.4915
Muthuraman A, Singh N (2011) Attenuating effect of hydroalcoholic extract of Acorus calamus in vincristine-induced painful neuropathy in rats. J Nat Med 65:480–487. https://doi.org/10.1007/s11418-011-0525-y
Muthuraman A, Singh N, Jaggi AS (2011) Protective effect of Acorus calamus L. in rat model of vincristine induced painful neuropathy: an evidence of anti-inflammatory and anti-oxidative activity. Food Chem Toxicol 49:2557–2563. https://doi.org/10.1016/j.fct.2011.06.069
Kim HK, Zhang YP, Gwak YS, Abdi S (2010) Phenyl N-tert-butylnitrone, a free radical scavenger, reduces mechanical allodynia in chemotherapy-induced neuropathic pain in rats. Anesthesiology 112:432–439. https://doi.org/10.1097/ALN.0b013e3181ca31bd
Okoth DA, Akala HM, Johnson JD, Koorbanally NA (2016) Alkyl phenols, alkenyl cyclohexenones and other phytochemical constituents from Lannea rivae (chiov) Sacleux (Anacardiaceae) and their bioactivity. Med Chem Res 25:690–703. https://doi.org/10.1007/s00044-016-1521-2
Mazimba O, Wale K, Loeto D, Kwape T (2014) Antioxidant and antimicrobial studies on fused-ring pyrazolones and isoxazolones. Bioorg Med Chem 22:6564–6569. https://doi.org/10.1016/j.bmc.2014.10.015
Rose M, Kam P (2002) Gabapentin: pharmacology and its use in pain management. Anaesthesia 57:451–462
Bennett MI, Simpson KH (2004) Gabapentin in the treatment of neuropathic pain. Palliat Med 18:5–11. https://doi.org/10.1191/0269216304pm845ra
Gilron I, Flatters SJ (2006) Gabapentin and pregabalin for the treatment of neuropathic pain: a review of laboratory and clinical evidence. Pain Res Manag 11:16A–29A. https://doi.org/10.1155/2006/651712
Acknowledgments
The selected cyclohexenone compound has been synthesized as part of a series of compounds and their structures were confirmed by Dr. Rasool Khan, Associate Professor, Institute of Chemical Science, University of Peshawar. We are grateful to him for providing a series of compounds and after preliminary study; we have selected the cited CHD compound for neuropharmacological study.
Author information
Authors and Affiliations
Contributions
GA initiated the research project and directed the research scholars as supervisor in conducting pharmacological experiments. GA critically evaluated the contents of the final version of the manuscript. JK accomplished the pharmacological experiments and performed calculations and statistical analysis. He developed the preliminary draft of the manuscript. RU helped JK in the conduction of the experiments. SU conducted experiment-related synthesis and structure confirmation under the supervision of RK. RK helped in planning and supervising the experiments related to chemistry of our selected compounds (chemistry structural data not included in this manuscript). All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khan, J., Ali, G., Khan, R. et al. Attenuation of vincristine-induced neuropathy by synthetic cyclohexenone-functionalized derivative in mice model. Neurol Sci 40, 1799–1811 (2019). https://doi.org/10.1007/s10072-019-03884-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-03884-6