Abstract
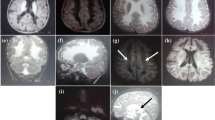
Brain iron accumulation disorders (BIADs) are a group of diseases characterized by iron overload in deep gray matter nuclei, which is a common feature of neurodegenerative diseases. Although genetic factors have been reported to be one of the etiologies, much more details about the genetic background and molecular mechanism of BIADs remain unclear. This study aimed to illustrate the genetic characteristics of BIADs and clarify their molecular mechanisms. A total of 84 patients with BIADs were recruited from April 2018 to October 2022 at Xuanwu Hospital. Clinical characteristics including family history, consanguineous marriage history, and age at onset (AAO) were collected and assessed by two senior neurologists. Neuroimaging data were conducted for all the patients, including cranial magnetic resonance imaging (MRI) and susceptibility-weighted imaging (SWI). Whole-exome sequencing (WES) and capillary electrophoresis for detecting sequence mutation and trinucleotide repeat expansion, respectively, were conducted on all patients and part of their parents (whose samples were available). Variant pathogenicity was assessed according to the American College of Medical Genetics and Association for Molecular Pathology (ACMG/AMP). The NBIA and NBIA-like genes with mutations were included for bioinformatic analysis, using Gene Ontology (GO) annotation and Kyoto Encyclopedia of Genes and Genome (KEGG). GO annotation and KEGG pathway analysis were performed on Metascape platform. In the 84 patients, 30 (35.7%) were found to carry mutations, among which 20 carried non-dynamic mutations (missense, stop-gained, frameshift, inframe, and exonic deletion) and 10 carried repeat expansion mutations. Compared with sporadic cases, familial cases had more genetic variants (non-dynamic mutation: P=0.025, dynamic mutation: P=0.003). AAO was 27.85±10.42 years in cases with non-dynamic mutations, which was significantly younger than those without mutations (43.13±17.17, t=3.724, P<0.001) and those with repeated expansions (45.40±8.90, t=4.550, P<0.001). Bioinformatic analysis suggested that genes in lipid metabolism, autophagy, mitochondria regulation, and ferroptosis pathways are more likely to be involved in the pathogenesis of BIADs. This study broadens the genetic spectrum of BIADs and has important implications in genetic counselling and clinical diagnosis. Patients diagnosed as BIADs with early AAO and family history are more likely to carry mutations. Bioinformatic analysis provides new insights into the molecular pathogenesis of BIADs, which may shed lights on the therapeutic strategy for neurodegenerative diseases.





Similar content being viewed by others
Data availability
The data of this study are available on request from the corresponding author.
References
Li W, Langkammer C, Chou YH, Petrovic K, Schmidt R, Song AW, Madden DJ, Ropele S, Liu C (2015) Association between increased magnetic susceptibility of deep gray matter nuclei and decreased motor function in healthy adults. Neuroimage 105:45–52
Dusek P, Hofer T, Alexander J, Roos PM, Aaseth JO (2022) Cerebral Iron Deposition in Neurodegeneration. Biomolecules 12:714
Ward RJ, Zucca FA, Duyn JH, Crichton RR, Zecca L (2014) The role of iron in brain ageing and neurodegenerative disorders. Lancet Neurol 13:1045–1060
Hayflick SJ, Kurian MA, Hogarth P (2018) Neurodegeneration with brain iron accumulation. Handb Clin Neurol 147:293–305
Kruer MC (2013) The neuropathology of neurodegeneration with brain iron accumulation. Int Rev Neurobiol 110:165–194
Ndayisaba A, Kaindlstorfer C, Wenning GK (2019) Iron in Neurodegeneration – Cause or Consequence? Front Neurosci 13:180
Dusek P, Schneider SA, Aaseth J (2016) Iron chelation in the treatment of neurodegenerative diseases. J Trace Elem Med Biol 38:81–92
Amaral LL, Gaddikeri S, Chapman PR, Roy R, Gaddikeri RS, Marussi VH, Bag AK (2015) Neurodegeneration with Brain Iron Accumulation: Clinicoradiological Approach to Diagnosis. J Neuroimaging 25:539–551
Hajirnis O, Udwadia-Hegde A (2015) Chronic GM1 Gangliosidosis with Characteristic "Wish Bone Sign" on Brain MRI. Another Type of Neurodegeneration with Brain Iron Accumulation? Mov Disord Clin Pract 2:323–325
Roubertie A, Hieu N, Roux CJ, Leboucq N, Manes G, Charif M, Echenne B, Goizet C, Guissart C, Meyer P, Marelli C, Rivier F, Burglen L, Horvath R, Hamel CP, Lenaers G (2018) AP4 deficiency: A novel form of neurodegeneration with brain iron accumulation? Neurol Genet 4:e217
Horvath R, Lewis-Smith D, Douroudis K, Duff J, Keogh M, Pyle A, Fletcher N, Chinnery PF (2015) SCP2 mutations and neurodegeneration with brain iron accumulation. Neurology 85:1909–1911
Dard R, Meyniel C, Touitou V, Stevanin G, Lamari F, Durr A, Ewenczyk C, Mochel F (2017) Mutations in DDHD1, encoding a phospholipase A1, is a novel cause of retinopathy and neurodegeneration with brain iron accumulation. Eur J Med Genet 60:639–642
Drecourt A, Babdor J, Dussiot M, Petit F, Goudin N, Garfa-Traoré M, Habarou F, Bole-Feysot C, Nitschké P, Ottolenghi C, Metodiev MD, Serre V, Desguerre I, Boddaert N, Hermine O, Munnich A, Rötig A (2018) Impaired Transferrin Receptor Palmitoylation and Recycling in Neurodegeneration with Brain Iron Accumulation. Am J Hum Genet 102:266–277
Jaberi E, Rohani M, Shahidi GA, Nafissi S, Arefian E, Soleimani M, Rasooli P, Ahmadieh H, Daftarian N, Carrami EM, Klotzle B, Fan JB, Turk C, Steemers F, Elahi E (2016) Identification of mutation in GTPBP2 in patients of a family with neurodegeneration accompanied by iron deposition in the brain. Neurobiol Aging 38:216.e11–216.e18
Arber CE, Li A, Houlden H, Wray S (2016) Review: Insights into molecular mechanisms of disease in neurodegeneration with brain iron accumulation: unifying theories. Neuropathol Appl Neurobiol 42:220–241
Cheng W, Zhang C, Ren X, Jiang Y, Han S, Liu Y, Cai J, Li M, Wang K, Liu Y, Hu H, Li Q, Yang P, Bao Z, Wu A (2017) Bioinformatic analyses reveal a distinct Notch activation induced by STAT3 phosphorylation in the mesenchymal subtype of glioblastoma. J Neurosurg 126:249–259
Zhang Q, Huang H, Zhang M, Fang C, Wang N, Jing X, Guo J, Sun W, Yang X, Xu Z (2022) Exome Sequencing Reveals Genetic Variability and Identifies Chronic Prognostic Loci in Chinese Sarcoidosis Patients. Front Oncol 12:910227
Haller S, Haacke EM, Thurnher MM, Barkhof F (2021) Susceptibility-weighted Imaging: Technical Essentials and Clinical Neurologic Applications. Radiology 299:23–26
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, Kondrashov AS, Sunyaev SR (2010) A method and server for predicting damaging missense mutations. Nat Methods 7:248–249
Sim NL, Kumar P, Hu J, Henikoff S, Schneider G, Ng PC (2012) SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic Acids Res 40:W452–W457
Ioannidis NM, Rothstein JH, Pejaver V et al (2016) REVEL: An Ensemble Method for Predicting the Pathogenicity of Rare Missense Variants. Am J Hum Genet 99:877–885
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL (2015) ACMG Laboratory Quality Assurance Committee. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17:405–424
McCormick EM, Lott MT, Dulik MC, Shen L, Attimonelli M, Vitale O, Karaa A, Bai R, Pineda-Alvarez DE, Singh LN, Stanley CM, Wong S, Bhardwaj A, Merkurjev D, Mao R, Sondheimer N, Zhang S, Procaccio V, Wallace DC et al (2020) Specifications of the ACMG/AMP standards and guidelines for mitochondrial DNA variant interpretation. Hum Mutat 41:2028–2057
Sahajpal NS, Barseghyan H, Kolhe R, Hastie A, Chaubey A (2021) Optical Genome Mapping as a Next-Generation Cytogenomic Tool for Detection of Structural and Copy Number Variations for Prenatal Genomic Analyses. Genes (Basel) 12:398
Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, Davis AP, Dolinski K, Dwight SS, Eppig JT, Harris MA, Hill DP, Issel-Tarver L, Kasarskis A, Lewis S, Matese JC, Richardson JE, Ringwald M, Rubin GM, Sherlock G (2000) Gene ontology: tool for the unification of biology, The Gene Ontology Consortium. Nat Genet 25:25–29
Kanehisa M, Sato Y (2020) KEGG Mapper for inferring cellular functions from protein sequences. Protein Sci 29:28–35
Zhou Y, Zhou B, Pache L, Chang M, Khodabakhshi AH, Tanaseichuk O, Benner C, Chanda SK (2019) Metascape provides a biologist-oriented resource for the analysis of systems-level datasets. Nat Commun 10:1523
Bonilha da Silva C, Bergo FPG, D'Abreu A, Cendes F, Lopes-Cendes I, França MC Jr (2014) Dentate nuclei T2 relaxometry is a reliable neuroimaging marker in Friedreich’s ataxia. Eur J Neurol 21:1131–1136
Borlot F, Regan BM, Bassett AS, Stavropoulos DJ, Andrade DM (2017) Prevalence of Pathogenic Copy Number Variation in Adults With Pediatric-Onset Epilepsy and Intellectual Disability. JAMA Neurol 74:1301–1311
Aoun M, Corsetto PA, Nugue G, Montorfano G, Ciusani E, Crouzier D, Hogarth P, Gregory A, Hayflick S, Zorzi G, Rizzo AM, Tiranti V (2017) Changes in Red Blood Cell membrane lipid composition: A new perspective into the pathogenesis of PKAN. Mol Genet Metab 121:180–189
Leoni V, Strittmatter L, Zorzi G, Zibordi F, Dusi S, Garavaglia B, Venco P, Caccia C, Souza AL, Deik A, Clish CB, Rimoldi M, Ciusani E, Bertini E, Nardocci N, Mootha VK, Tiranti V (2012) Metabolic consequences of mitochondrial coenzyme A deficiency in patients with PANK2 mutations. Mol Genet Metab 105:463–471
Cheon Y, Kim HW, Igarashi M, Modi HR, Chang L, Ma K, Greenstein D, Wohltmann M, Turk J, Rapoport SI, Taha AY (2012) Disturbed brain phospholipid and docosahexaenoic acid metabolism in calcium-independent phospholipase A(2)-VIA (iPLA(2)β)-knockout mice. Biochim Biophys Acta 1821:1278–1286
Shinto L, Quinn J, Montine T, Dodge HH, Woodward W, Baldauf-Wagner S, Waichunas D, Bumgarner L, Bourdette D, Silbert L, Kaye J (2014) A randomized placebo-controlled pilot trial of omega-3 fatty acids and alpha lipoic acid in Alzheimer’s disease. J Alzheimers Dis 38:111–120
Di Pardo A, Amico E, Basit A, Armirotti A, Joshi P, Neely MD, Vuono R, Castaldo S, Digilio AF, Scalabrì F, Pepe G, Elifani F, Madonna M, Jeong SK, Park BM, D'Esposito M, Bowman AB, Barker RA, Maglione V (2017) Defective Sphingosine-1-phosphate metabolism is a druggable target in Huntington’s disease. Sci Rep 7:5280
Galvagnion C (2017) The Role of Lipids Interacting with α-Synuclein in the Pathogenesis of Parkinson’s Disease. J Parkinsons Dis 7:433–450
Aring L, Choi EK, Kopera H, Lanigan T, Iwase S, Klionsky DJ, Seo YA (2022) A neurodegeneration gene, WDR45, links impaired ferritinophagy to iron accumulation. J Neurochem 160:356–375
Muñoz-Braceras S, Tornero-Écija AR, Vincent O, Escalante R (2019) VPS13A is closely associated with mitochondria and is required for efficient lysosomal degradation. Dis Model Mech 12. https://doi.org/10.1242/dmm.036681
Frake RA, Ricketts T, Menzies FM, Rubinsztein DC (2015) Autophagy and neurodegeneration. J Clin Invest 125:65–74
Álvarez-Córdoba M, Fernández Khoury A, Villanueva-Paz M, Gómez-Navarro C, Villalón-García I, Suárez-Rivero JM, Povea-Cabello S, de la Mata M, Cotán D, Talaverón-Rey M, Pérez-Pulido AJ, Salas JJ, Pérez-Villegas EM, Díaz-Quintana A, Armengol JA, Sánchez-Alcázar JA (2019) Pantothenate Rescues Iron Accumulation in Pantothenate Kinase-Associated Neurodegeneration Depending on the Type of Mutation. Mol Neurobiol 56:3638–3656
Sumi-Akamaru H, Beck G, Shinzawa K, Kato S, Riku Y, Yoshida M, Fujimura H, Tsujimoto Y, Sakoda S, Mochizuki H (2016) High expression of α-synuclein in damaged mitochondria with PLA2G6 dysfunction. Acta Neuropathol Commun 4:27
Zhou ZD, Lee JCT, Tan EK (2018) Pathophysiological mechanisms linking F-box only protein 7 (FBXO7) and Parkinson’s disease (PD). Mutat Res Rev Mutat Res 778:72–78
Kim S, Wong YC, Gao F, Krainc D (2021) Dysregulation of mitochondria-lysosome contacts by GBA1 dysfunction in dopaminergic neuronal models of Parkinson’s disease. Nat Commun 12:1807
Hu CL, Nydes M, Shanley KL, Morales Pantoja IE, Howard TA, Bizzozero OA (2019) Reduced expression of the ferroptosis inhibitor glutathione peroxidase-4 in multiple sclerosis and experimental autoimmune encephalomyelitis. J Neurochem. 148:426–439
Ashraf A, So PW (2020) Spotlight on Ferroptosis: Iron-Dependent Cell Death in Alzheimer’s Disease. Front Aging Neurosci 12:196
Maccarinelli F, Pagani A, Cozzi A, Codazzi F, Di Giacomo G, Capoccia S, Rapino S, Finazzi D, Politi LS, Cirulli F, Giorgio M, Cremona O, Grohovaz F, Levi S (2015) A novel neuroferritinopathy mouse model (FTL 498InsTC) shows progressive brain iron dysregulation, morphological signs of early neurodegeneration and motor coordination deficits. Neurobiol Dis 81:119–133
Bonaccorsi di Patti MC, Cutone A, Polticelli F, Rosa L, Lepanto MS, Valenti P, Musci G (2018) The ferroportin-ceruloplasmin system and the mammalian iron homeostasis machine: regulatory pathways and the role of lactoferrin. Biometals 31:399–414
Reichert CO, de Freitas FA, Sampaio-Silva J, Rokita-Rosa L, Barros PL, Levy D, Bydlowski SP (2020) Ferroptosis Mechanisms Involved in Neurodegenerative Diseases. Int J Mol Sci 21:8765
Acknowledgements
The authors would like to thank all the participants and their family members in this study.
Funding
This study is supported by the National Natural Science Foundation (NNSF) of China to Dr. C.W (No. 82171412; No. 81771212).
Author information
Authors and Affiliations
Contributions
Lianghao Si: data curation, methodology, investigation, writing—original draft. Zhanjun Wang: case enrollment, clinical assessment. Xu-Ying Li: data curation genetic data analysis, methodology. Yang Song: case enrollment, clinical assessment. Tingyan Yao: genetic data analysis, methodology. Erhe Xu: case enrollment, clinical assessment. Xianling Wang: case enrollment, clinical assessment. Chaodong Wang: conceptualization, writing—review, editing and supervision.
Corresponding author
Ethics declarations
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Xuanwu Hospital of the Capital Medical University (Clinical Research Audit: [2021]034)). The informed consent was obtained from all the participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Si, L., Wang, Z., Li, XY. et al. Novel mutations and molecular pathways identified in patients with brain iron accumulation disorders. Neurogenetics 24, 231–241 (2023). https://doi.org/10.1007/s10048-023-00725-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10048-023-00725-9