Abstract
Regenerative medicine products using allogeneic cells, such as allogeneic cultured epidermis (allo-CE), have become a more critical therapeutic method for the treatment of burns. However, there are no clinically available allo-CE products in Japan. Therefore, establishing a quality-controlled cell bank is mandatory to create regenerative medical products using allogeneic cells. In this study, we selected ten patients from the Department of Plastic Surgery of Kyoto University Hospital to become cell donors. We performed medical interviews and blood sampling for the donor to ensure virus safety. We examined the tissues and isolated cells by performing a nucleic acid test (NAT). To establish a master cell bank, quality evaluation was performed according to the International Conference of Harmonization (ICH) Q5A. Serological tests of the blood samples from the ten donors showed that two of them were ineligible. The cells registered in the cell bank were found to be compatible after virus testing was performed, and a master cell bank was constructed. Hence, we established a keratinocyte and fibroblast bank of clinically usable human cultured cells in Japan for the first time.
Similar content being viewed by others
References
Berthiaume F, Maguire TJ, Yarmush ML. Tissue engineering and regenerative medicine: History, progress, and challenges. Annu Rev Chem Biomol Eng. 2011;2:403–30. https://doi.org/10.1146/annurev-chembioeng-061010-114257.
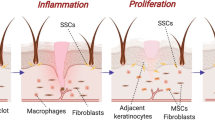
Sakamoto M, Morimoto N, Inoie M, Takahagi M, Ogino S, Jinno C, et al. Cultured human epidermis combined with meshed skin autografts accelerates epithelialization and granulation tissue formation in a rat model. Ann Plast Surg. 2017;78:651–8. https://doi.org/10.1097/SAP.0000000000001058.
Sakamoto M, Ogino S, Shimizu Y, Inoie M, Lee S, Yamanaka H, et al. Human cultured epidermis accelerates wound healing regardless of its viability in a diabetic mouse model. PLoS ONE. 2020;15: e0237985. https://doi.org/10.1371/journal.pone.0237985.
Madden MR, Finkelstein JL, Staiano-Coico L, Goodwin CW, Shires GT, Nolan EE, et al. Grafting of cultured allogeneic epidermis on second- and third-degree burn wounds on 26 patients. J Trauma. 1986;26:955–62. https://doi.org/10.1097/00005373-198611000-00001.
Hefton JM, Madden MR, Finkelstein JL, Shires GT. Grafting of burn patients with allografts of cultured epidermal cells. Lancet. 1983;2:428–30. https://doi.org/10.1016/s0140-6736(83)90392-6.
De Luca M, Albanese E, Bondanza S, Megna M, Ugozzoli L, Molina F, et al. Multicentre experience in the treatment of burns with autologous and allogenic cultured epithelium, fresh or preserved in a frozen state. Burns. 1989;15:303–9. https://doi.org/10.1016/0305-4179(89)90007-7.
van der Merwe AE, Mattheyse FJ, Bedford M, van Helden PD, Rossouw DJ. Allografted keratinocytes used to accelerate the treatment of burn wounds are replaced by recipient cells. Burns. 1990;16:193–7. https://doi.org/10.1016/0305-4179(90)90038-x.
De Luca M, Bondanza S, Cancedda R, Tamisani AM, Di Noto C, Muller L, et al. Permanent coverage of full skin thickness burns with autologous cultured epidermis and reepithelialization of partial skin thickness lesions induced by allogeneic cultured epidermis: A multicentre study in the treatment of children. Burns. 1992;18:S16–9. https://doi.org/10.1016/0305-4179(92)90105-4.
Teepe RG, Roseeuw DI, Hermans J, Koebrugge EJ, Altena T, de Coninck A, et al. Randomized trial comparing cryopreserved cultured epidermal allografts with hydrocolloid dressings in healing chronic venous ulcers. J Am Acad Dermatol. 1993;29:982–8. https://doi.org/10.1016/0190-9622(93)70278-2.
Phillips TJ, Provan A, Colbert D, Easley KW. A randomized single-blind controlled study of cultured epidermal allografts in the treatment of split-thickness skin graft donor sites. Arch Dermatol. 1993;129:879–82.
Rivas-Torres MT, Amato D, Arámbula-Alvarez H, Kuri-Harcuch W. Controlled clinical study of skin donor sites and deep partial-thickness burns treated with cultured epidermal allografts. Plast Reconstr Surg. 1996;98:279–87. https://doi.org/10.1097/00006534-199608000-00011.
Duinslaeger LA, Verbeken G, Vanhalle S, Vanderkelen A. Cultured allogeneic keratinocyte sheets accelerate healing compared to Op-site treatment of donor sites in burns. J Burn Care Rehabil. 1997;18:545–51. https://doi.org/10.1097/00004630-199711000-00013.
Beele H, Naeyaert JM, Goeteyn M, De Mil M, Kint A. Repeated cultured epidermal allografts in the treatment of chronic leg ulcers of various origins. Dermatologica. 1991;183:31–5. https://doi.org/10.1159/000247628.
Lindgren C, Marcusson JA, Toftgård R. Treatment of venous leg ulcers with cryopreserved cultured allogeneic keratinocytes: a prospective open controlled study. Br J Dermatol. 1998;139:271–5. https://doi.org/10.1046/j.1365-2133.1998.02364.x.
Leigh IM, Purkis PE, Navsaria HA, Phillips TJ. Treatment of chronic venous ulcers with sheets of cultured allogenic keratinocytes. Br J Dermatol. 1987;117:591–7. https://doi.org/10.1111/j.1365-2133.1987.tb07491.x.
Andrews PW, Cavagnaro J, Deans R, Feigal E, Horowitz E, Keating A, et al. Harmonizing standards for producing clinical-grade therapies from pluripotent stem cells. Nat Biotechnol. 2014;32:724–6. https://doi.org/10.1038/nbt.2973.
Heng WL, Wang QW, Sornarajah R, Tremblay J, Putri NM, Hamid SSA, et al. A review of skin banking guidelines and standards worldwide: Towards the harmonization of guidelines for skin banking in therapeutic applications for the regions under the Asia Pacific Burn Association (APBA). Burns Trauma. 2020;8:tkaa019. https://doi.org/10.1093/burnst/tkaa019.
Cobo F, Stacey GN, Hunt C, Cabrera C, Nieto A, Montes R, et al. Microbiological control in stem cell banks: approaches to standardisation. Appl Microbiol Biotechnol. 2005;68:456–66. https://doi.org/10.1007/s00253-005-0062-2.
Ramarli D, Giri A, Reina S, Poffe O, Cancedda R, Varnier O, et al. HIV-1 spreads from lymphocytes to normal human keratinocytes suitable for autologous and allogenic transplantation. J Invest Dermatol. 1995;105:644–7. https://doi.org/10.1111/1523-1747.ep12324100.
Dodd RY, Crowder LA, Haynes JM, Notari EP, Stramer SL, Steele WR. Screening blood donors for HIV, HCV, and HBV at the American Red Cross: 10-year trends in prevalence, incidence, and residual risk, 2007 to 2016. Transfus Med Rev. 2020;34:81–93. https://doi.org/10.1016/j.tmrv.2020.02.001.
Stramer SL, Dodd RY. AABB Transfusion-Transmitted Diseases Emerging Infectious Diseases Subgroup. Transfusion-transmitted emerging infectious diseases: 30 years of challenges and progress. Transfusion. 2013;53:2375–83. https://doi.org/10.1111/trf.12371.
Ward JW, Holmberg SD, Allen JR, Cohn DL, Critchley SE, Kleinman SH, et al. Transmission of human immunodeficiency virus (HIV) by blood transfusions screened as negative for HIV antibody. N Engl J Med. 1988;318:473–8. https://doi.org/10.1056/NEJM198802253180803.
Durand F, Beauplet A, Marcellin P. Evidence of hepatitis C virus viremia without detectable antibody to hepatitis C virus in a blood donor. Ann Intern Med. 2000;133:74–5. https://doi.org/10.7326/0003-4819-133-1-200007040-00018.
Glynn SA, Kleinman SH, Schreiber GB, Busch MP, Wright DJ, Smith JW, et al. Trends in incidence and prevalence of major transfusion-transmissible viral infections in US blood donors, 1991 to 1996 Retrovirus Epidemiology Donor Study (REDS). JAMA. 2000;284:229–35. https://doi.org/10.1001/jama.284.2.229.
Stramer SL, Glynn SA, Kleinman SH, Strong DM, Caglioti S, Wright DJ, et al. Detection of HIV-1 and HCV infections among antibody-negative blood donors by nucleic acid-amplification testing. N Engl J Med. 2004;351:760–8. https://doi.org/10.1056/NEJMoa040085.
Takeuchi H, Kobayashi R, Hasegawa M, Hirai K. Detection of latent infection by Epstein-Barr virus in peripheral blood cells of healthy individuals and in non-neoplastic tonsillar tissue from patients by reverse transcription-polymerase chain reaction. J Virol Methods. 1996;58:81–9. https://doi.org/10.1016/0166-0934(95)01993-6.
Cassinotti P, Burtonboy G, Fopp M, Siegl G. Evidence for persistence of human parvovirus B19 DNA in bone marrow. J Med Virol. 1997;53:229–32. https://doi.org/10.1002/(SICI)1096-9071(199711)53:3%3c229::AID-JMV8%3e3.0.CO;2-A.
Garbuglia AR, Iezzi T, Capobianchi MR, Pignoloni P, Pulsoni A, Sourdis J, et al. Detection of TT virus in lymph node biopsies of B-cell lymphoma and Hodgkin’s disease, and its association with EBV infection. Int J Immunopathol Pharmacol. 2003;16:109–18. https://doi.org/10.1177/039463200301600204.
Fanci R, De Santis R, Zakrzewska K, Paci C, Azzi A. Presence of TT virus DNA in bone marrow cells from hematologic patients. New Microbiol. 2004;27:113–7.
Arnold DM, Neame PB, Meyer RM, Soamboonsrup P, Luinstra KE, O’Hoski P, et al. Autologous peripheral blood progenitor cells are a potential source of parvovirus B19 infection. Transfusion. 2005;45:394–8. https://doi.org/10.1111/j.1537-2995.2005.04267.x.
Suthar MS, Diamond MS, Gale MJ. West Nile virus infection and immunity. Nat Rev Microbiol. 2013;11:115–28. https://doi.org/10.1038/nrmicro2950.
Zou S, Dodd RY, Stramer SL, Strong DM. Tissue Safety Study Group. Probability of viremia with HBV, HCV, HIV, and HTLV among tissue donors in the United States. N Engl J Med. 2004;351:751–9. https://doi.org/10.1056/NEJMoa032510.
Drexler HG, Uphoff CC. Mycoplasma contamination of cell cultures: Incidence, sources, effects, detection, elimination, prevention. Cytotechnology. 2002;39:75–90. https://doi.org/10.1023/A:1022913015916.
Roush DJ. Integrated viral clearance strategies-reflecting on the present, projecting to the future. Curr Opin Biotechnol. 2018;53:137–43. https://doi.org/10.1016/j.copbio.2018.01.003.
Moravvej H, Abdollahimajd F, Naseh MH, Piravar Z, Abolhasani E, Mozafari N, et al. Cultured allogeneic fibroblast injection vs. fibroblasts cultured on amniotic membrane scaffold for dystrophic epidermolysis bullosa treatment. Br J Dermatol. 2018;179:72–9. https://doi.org/10.1111/bjd.16338.
Sakamoto M, Nakano T, Tsuge I, Yamanaka H, Katayama Y, Shimizu Y, et al. Dried human cultured epidermis accelerates wound healing in diabetic mouse skin defect wounds. Sci Rep. 2022;12(1):3184. https://doi.org/10.1038/s41598-022-07156-w.
Brohlin M, Kingham PJ, Novikova LN, Novikov LN, Wiberg M. Aging effect on neurotrophic activity of human mesenchymal stem cells. PLoS ONE. 2012;7: e45052. https://doi.org/10.1371/journal.pone.0045052.
Ferri C, Zakrzewska K, Longombardo G, Giuggioli D, Storino FA, Pasero G, et al. Parvovirus B19 infection of bone marrow in systemic sclerosis patients. Clin Exp Rheumatol. 1999;17:718–20.
Lundqvist A, Isa A, Tolfvenstam T, Kvist G, Broliden K. High frequency of parvovirus B19 DNA in bone marrow samples from rheumatic patients. J Clin Virol. 2005;33:71–4. https://doi.org/10.1016/j.jcv.2004.11.011.
Acknowledgements
The authors would like to thank Rie Tatsumi, Minako Chaya, and Yasuko Minaki for their generous assistance.
Funding
This research was supported by the Japan Agency for Medical Research and Development (AMED) under Grant Number JP17be0104005.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
Our study was approved by the Ethics Committee at our institute (No. R0690).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakano, T., Katayama, Y., Sakamoto, M. et al. Establishment of a keratinocyte and fibroblast bank for clinical applications in Japan. J Artif Organs 26, 45–52 (2023). https://doi.org/10.1007/s10047-022-01331-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-022-01331-6