Abstract
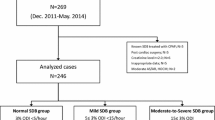
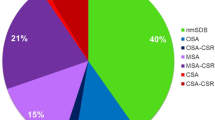
Sleep-disordered breathing (SDB) is associated with an increased risk of adverse events in patients with heart failure (HF); however, its impact in patients implanted with a left ventricular assist device (LVAD) remains unclear. We aimed to investigate the prevalence of SDB in patients with LVAD and its impact on their clinical outcomes. Fifty consecutive patients with LVAD who underwent portable sleep monitoring between September 2017 and April 2018 were prospectively enrolled, and they were followed up for 170 ± 36 days. According to their respiratory disturbance indexes (RDIs), they were categorized into the SDB group (RDI ≥ 15, n = 12) and the non-SDB group (RDI < 15, n = 38). The incidence of adverse events during the follow-up period was investigated after enrollment. Multivariate logistic regression analysis revealed significant differences in SDB in LVAD-implanted patients in terms of the logarithmic transformation brain natriuretic peptide (BNP) values (p = 0.005). The optimal BNP cut-off value for SDB prediction in LVAD-implanted patients was 300 pg/mL (sensitivity: 58.3%, specificity: 94.7%). During follow-up, ventricular tachyarrhythmias (VTas) occurred significantly more frequently in the SDB group (4 [33%] vs. 2 [5%] patients, p = 0.02); Atrial tachyarrhythmia (ATa) also tended to occur more frequently in the SDB group (2 [25%] vs. 2 [2%] patients, p = 0.07). SBD was prevalent in 24% of the LVAD-implanted patients with advanced HF. Furthermore, SDB was significantly associated with high BNP levels and was also potentially associated with subsequent incidence of VTa in patients with LVAD.


Similar content being viewed by others
References
Sharma B, Owens R, Malhotra A. Sleep in congestive heart failure. Med Clin North Am. 2010;94:447–64.
Phillips BG, Narkiewicz K, Pesek CA, Haynes WG, Dyken ME, Somers VK. Effects of obstructive sleep apnea on endothelin-1 and blood pressure. J Hypertens. 1999;17:61–6.
Takahashi S, Nakamura Y, Nishijima T, Sakurai S, Inoue H. Essential roles of angiotensin II in vascular endothelial growth factor expression in sleep apnea syndrome. Respir Med. 2005;99:1125–31.
Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. 2008;118:1080–111.
Bucca CB, Brussino L, Battisti A, et al. Diuretics in obstructive sleep apnea with diastolic heart failure. Chest. 2007;132:440–6.
Tamura A, Kawano Y, Naono S, Kotoku M, Kadota J. Relationship between beta-blocker treatment and the severity of central sleep apnea in chronic heart failure. Chest. 2007;131:130–5.
Gabor JY, Newman DA, Barnard-Roberts V, et al. Improvement in Cheyne–Stokes respiration following cardiac resynchronisation therapy. Eur Respir J. 2005;26:95–100.
Yagi H, Nakata S, Tsuge H, et al. Significance of a screening device (Apnomonitor 5) for sleep apnea syndrome. Auris Nasus Larynx. 2009;36:176–80.
Di Lenarda A, Remme WJ, Charlesworth A, et al. Exchange of beta-blockers in heart failure patients. Experiences from the poststudy phase of COMET (the carvedilol or metoprolol European Trial). Eur J Heart Fail. 2005;7:640–9.
Stainback RF, Estep JD, Agler DA, et al. Echocardiography in the management of patients with left ventricular assist devices: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2015;28:853–909.
Hoeper MM, Maier R, Tongers J, et al. Determination of cardiac output by the Fick method, thermodilution, and acetylene rebreathing in pulmonary hypertension. Am J Respir Crit Care Med. 1999;160:535–41.
INTERMACS Executive Committee. INTERMACS adverse event definitions: adult and pediatric patients. http://www.uab.edu/medicine/intermacs/appendices-4-0/appendix-a-4-0. Accessed 17 Nov 2016.
Vazir A, Hastings PC, Morrell MJ, et al. Resolution of central sleep apnoea following implantation of a left ventricular assist device. Int J Cardiol. 2010;138:317–9.
Voortman M, Ramjankan FZ, Lahpor JR, De Jonge N, Kwakkel-Van Erp JM. Obstructive sleep apnea in heart failure with nearly complete resolution after implantation of a left ventricular assist device. J Heart Cardiol. 2014;1:1–3.
Padeletti M, Henriquez A, Mancini DM, Basner RC. Persistence of Cheyne–Stokes breathing after left ventricular assist device implantation in patients with acutely decompensated end-stage heart failure. J Heart Lung Transplant. 2007;26:742–4.
Schaffer SA, Bercovitch RS, Ross HJ, Rao V. Central sleep apnea interfering with adequate left ventricular filling in a patient with left ventricular assist device. J Clin Sleep Med. 2013;9:161–2.
Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med. 1999;160:1101–6.
Christ M, Sharkova Y, Fenske H, et al. Brain natriuretic peptide for prediction of Cheyne–Stokes respiration in heart failure patients. Int J Cardiol. 2007;116:62–9.
Sato T, Seguchi O, Iwashima Y, et al. Serum brain natriuretic peptide concentration 60 days after surgery as a predictor of long-term prognosis in patients implanted with a left ventricular assist device. ASAIO J. 2015;61:373–8.
Fichter J, Bauer D, Arampatzis S, Fries R, Heisel A, Sybrecht GW. Sleep-related breathing disorders are associated with ventricular arrhythmias in patients with an implantable cardioverter-defibrillator. Chest. 2002;122:558–61.
Serizawa N, Yumino D, Kajimoto K, et al. Impact of sleep-disordered breathing on life-threatening ventricular arrhythmia in heart failure patients with implantable cardioverter-defibrillator. Am J Cardiol. 2008;102:1064–8.
Ryan CM, Usui K, Floras JS, Bradley TD. Effect of continuous positive airway pressure on ventricular ectopy in heart failure patients with obstructive sleep apnoea. Thorax. 2005;60:781–5.
Bitter T, Westerheide N, Prinz C, et al. Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur Heart J. 2011;32:61–74.
Franz MR. Mechano-electrical feedback in ventricular myocardium. Cardiovasc Res. 1996;32:15–24.
Schlatzer C, Schwarz EI, Sievi NA, et al. Intrathoracic pressure swings induced by simulated obstructive sleep apnoea promote arrhythmias in paroxysmal atrial fibrillation. Europace. 2016;18:64–70.
Yoruk A, Sherazi S, Massey HT, et al. Predictors and clinical relevance of ventricular tachyarrhythmias in ambulatory patients with a continuous flow left ventricular assist device. Heart Rhythm. 2016;13:1052–6.
Bedi M, Kormos R, Winowich S, McNamara DM, Mathier MA, Murali S. Ventricular arrhythmias during left ventricular assist device support. Am J Cardiol. 2007;99:1151–3.
Refaat M, Chemaly E, Lebeche D, Gwathmey JK, Hajjar RJ. Ventricular arrhythmias after left ventricular assist device implantation. Pacing Clin Electrophysiol. 2008;31:1246–52.
Vollkron M, Voitl P, Ta J, Wieselthaler G, Schima H. Suction events during left ventricular support and ventricular arrhythmias. J Heart Lung Transplant. 2007;26:819–25.
Nakashima H, Katayama T, Takagi C, et al. Obstructive sleep apnoea inhibits the recovery of left ventricular function in patients with acute myocardial infarction. Eur Heart J. 2006;27:2317–22.
Funding
The authors have no source of funding statement.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kumai, Y., Seguchi, O., Mochizuki, H. et al. Impact of sleep-disordered breathing on ventricular tachyarrhythmias after left ventricular assist device implantation. J Artif Organs 25, 223–230 (2022). https://doi.org/10.1007/s10047-021-01307-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-021-01307-y