Abstract
Purpose
Robotic inguinal hernia repair (RHR) is an evolving technique but is comparatively expensive and has yet to show superior outcomes versus open (OHR) or laparoscopic (LHR) approaches. The utilization and clinical outcomes of RHR have not been reported within the veterans affairs (VA) system. This study analyzes trends in utilization and 30-day post-operative outcomes between OHR, LHR, and RHR in veterans.
Methods
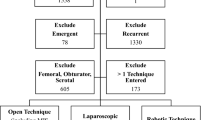
This is a retrospective review of patients that underwent inguinal herniorrhaphy using the Veterans Affairs Quality Improvement Program database. Multivariable analysis of outcomes was performed adjusting for pre-operative confounding covariates between OHR, LHR, and RHR. Trends in utilization, complication rates, and operative times were also reported.
Results
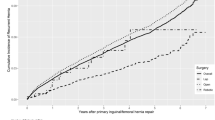
From 2008–2019, 124,978 cases of inguinal herniorrhaphy were identified: 100,880 (80.7%) OHR, 18,035 (14.4%) LHR, and 6063 (4.9%) RHR. Compared to LHR, RHR was associated with 4.94 times higher odds of complications, 100 min longer mean operative time, and 1.5 days longer median length of stay (LOS). Compared to OHR, RHR was associated with 5.92 times higher odds of complications, 57 min longer mean operative time, and 1.1 days longer median LOS. Utilization of RHR and LHR significantly increased over time. RHR complication rates decreased over time (2008: 20.8% to 2019: 3.2%) along with mean operative times (2008: 4.9 h to 2019: 2.8 h; p < 0.05).
Conclusion
While this study demonstrated inferior outcomes after RHR, the temporal trends are encouraging. This may be due to increased surgeon experience with robotics. Further prospective data will elucidate the role of RHR as this technique increases.





Similar content being viewed by others
Data availability
Data were obtained from Veterans Affairs Surgical Quality Improvement Database and used only for the purposes of this research.
Code availability
Statistical analysis was conducted with SAS version 9.4.
References
Ruhl CE, Everhart JE (2007) Risk factors for inguinal hernia among adults in the US population. Am J Epidemiol 165(10):1154–1161
Berndsen MR, Gudbjartsson T, Berndsen FH (2019) Inguinal hernia—review. Laeknabladid 105(9):385–391. https://doi.org/10.17992/lbl.2019.09.247
Miller HJ (2018) Inguinal hernia: mastering the anatomy. Surg Clin North Am 98(3):607–621
Köckerling F, Simons MP (2018) Current concepts of inguinal hernia repair. Visc Med 34(2):145–150. https://doi.org/10.1159/000487278
Stroupe KT, Manheim LM, Luo P et al (2006) Tension-free repair versus watchful waiting for men with asymptomatic or minimally symptomatic inguinal hernias: a cost-effectiveness analysis. J Am Coll Surg 203(4):458–468
Ramanan B, Maloley BJ, Fitzgibbons RJ Jr (2014) Inguinal hernia: follow or repair? Adv Surg 48:1–11
Lichtenstein ME (1954) The custom-tailored inguinal hernia repair. J Okla State Med Assoc 47(8):222–224
Liem MS, van Vroonhoven TJ (1996) Laparoscopic inguinal hernia repair. Br J Surg 83(9):1197–1204
Wei FX, Zhang YC, Han W, Zhang YL, Shao Y, Ni R (2015) Transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) for laparoscopic hernia repair: a meta-analysis. Surg Laparosc Endosc Percutan Tech 25(5):375–383. https://doi.org/10.1097/SLE.0000000000000123
Birth M, Friedman RL, Melullis M, Weiser HF (1996) Laparoscopic transabdominal preperitoneal hernioplasty: results of 1000 consecutive cases. J Laparoendosc Surg 6(5):293–300. https://doi.org/10.1089/lps.1996.6.293
Wake BL, McCormack K, Fraser C, Vale L, Perez J, Grant AM (2005) Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev 1:CD004703
Tanphiphat C, Tanprayoon T, Sangsubhan C, Chatamra K (1998) Laparoscopic vs open inguinal hernia repair. A randomized, controlled trial. Surg Endosc. 12(6):846–851. https://doi.org/10.1007/s004649900727
McCormack K, Scott NW, Go PM, Ross S, Grant AM, EU Hernia Trialists Collaboration (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev 1:CD001785
Trevisonno M, Kaneva P, Watanabe Y et al (2015) Current practices of laparoscopic inguinal hernia repair: a population-based analysis. Hernia 19(5):725–733. https://doi.org/10.1007/s10029-015-1358-5
Tadaki C, Lomelin D, Simorov A et al (2016) Perioperative outcomes and costs of laparoscopic versus open inguinal hernia repair. Hernia 20(3):399–404. https://doi.org/10.1007/s10029-016-1465-y
Perez AJ, Strassle PD, Sadava EE, Gaber C, Schlottmann F (2020) Nationwide analysis of inpatient laparoscopic versus open inguinal hernia repair. J Laparoendosc Adv Surg Tech A 30(3):292–298. https://doi.org/10.1089/lap.2019.0656
Tian W, Fei Y (2018) Application of da vinci robotic surgery to hernia repair. Zhonghua Wei Chang Wai Ke Za Zhi 21(7):740–743
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911. https://doi.org/10.1001/jamanetworkopen.2019.18911
Charles EJ, Mehaffey JH, Tache-Leon CA, Hallowell PT, Sawyer RG, Yang Z (2018) Inguinal hernia repair: is there a benefit to using the robot? Surg Endosc 32(4):2131–2136. https://doi.org/10.1007/s00464-017-5911-4
Janjua H, Cousin-Peterson E, Barry TM, Kuo MC, Baker MS, Kuo PC (2020) The paradox of the robotic approach to inguinal hernia repair in the inpatient setting. Am J Surg 219(3):497–501
Khoraki J, Gomez PP, Mazzini GS et al (2020) Perioperative outcomes and cost of robotic-assisted versus laparoscopic inguinal hernia repair. Surg Endosc 34(8):3496–3507. https://doi.org/10.1007/s00464-019-07128-8
Kakiashvili E, Bez M, Abu Shakra I et al (2021) Robotic inguinal hernia repair: is it a new era in the management of inguinal hernias? Asian J Surg. https://doi.org/10.1016/j.asjsur.2020.03.015
Aiolfi A, Cavalli M, Micheletto G et al (2019) Primary inguinal hernia: systematic review and bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 23(3):473–484. https://doi.org/10.1007/s10029-019-01964-2
Huerta S, Timmerman C, Argo M et al (2019) Open, laparoscopic, and robotic inguinal hernia repair: outcomes and predictors of complications. J Surg Res 241:119–127
Abdelmoaty WF, Dunst CM, Neighorn C, Swanstrom LL, Hammill CW (2019) Robotic-assisted versus laparoscopic unilateral inguinal hernia repair: a comprehensive cost analysis. Surg Endosc 33(10):3436–3443. https://doi.org/10.1007/s00464-018-06606-9
Prabhu AS, Carbonell A, Hope W et al (2020) Robotic inguinal vs transabdominal laparoscopic inguinal hernia repair: the RIVAL randomized clinical trial. JAMA Surg 155(5):380–387. https://doi.org/10.1001/jamasurg.2020.0034
Odani S, Agaku IT, Graffunder CM, Tynan MA, Armour BS (2018) Tobacco product use among military veterans—United States, 2010–2015. MMWR Morb Mortal Wkly Rep 67(1):7–12. https://doi.org/10.15585/mmwr.mm6701a2
Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM (2012) Health and health behavior differences: U.S. military, veteran, and civilian men. Am J Prev Med 43(5):483–489
Klevens RM, Giovino GA, Peddicord JP, Nelson DE, Mowery P, Grummer-Strawn L (1995) The association between veteran status and cigarette-smoking behaviors. Am J Prev Med 11(4):245–250
Eibner (2015) Current and projected characteristics and unique health care needs of the patient population served by the department of veterans affairs. RAND Corporation https://doi.org/10.7249/j.ctt19w735m
Oshinski R (2020) Annual surgery report 2019. National Surgery Office. Veterans Health Administration, Washington DC
Massarweh NN, Kaji AH, Itani KMF (2018) Practical guide to surgical data sets: veterans affairs surgical quality improvement program (VASQIP). JAMA Surg 153(8):768–769
Kudsi OY, McCarty JC, Paluvoi N, Mabardy AS (2017) Transition from laparoscopic totally extraperitoneal inguinal hernia repair to robotic transabdominal preperitoneal inguinal hernia repair: a retrospective review of a single surgeon’s experience. World J Surg 41(9):2251–2257. https://doi.org/10.1007/s00268-017-3998-3
Diez-Barroso R Jr, Palacio CH, Martinez JA et al (2018) Robotic port-site hernias after general surgical procedures. J Surg Res 230:7–12
Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P (2017) Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect (Larchmt) 18(6):722–735. https://doi.org/10.1089/sur.2017.089
Procter LD, Davenport DL, Bernard AC, Zwischenberger JB (2010) General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg 210(1):60–62. https://doi.org/10.1016/j.jamcollsurg.2009.09.034
Tatarian T, Nie L, McPartland C et al (2021) Comparative perioperative and 5-year outcomes of robotic and laparoscopic or open inguinal hernia repair: a study of 153,727 patients in the state of new york. Surg Endosc. https://doi.org/10.1007/s00464-020-08211-1
Napolitano MA, Skancke M, Walters J et al (2020) Outcomes and trends in colorectal surgery in U.S. veterans: a 10-year experience at a tertiary veterans affairs medical center. J Laparoendosc Adv Surg Tech A 30(4):378–382. https://doi.org/10.1089/lap.2019.0739
Muysoms F, Van Cleven S, Kyle-Leinhase I, Ballecer C, Ramaswamy A (2018) Robotic-assisted laparoscopic groin hernia repair: observational case-control study on the operative time during the learning curve. Surg Endosc 32(12):4850–4859. https://doi.org/10.1007/s00464-018-6236-7
Awad MA, Buzalewski J, Anderson C et al (2020) Robotic inguinal hernia repair outcomes: Operative time and cost analysis. J Soc Laparoendosc Surg. https://doi.org/10.4293/JSLS.2020.00058
Qabbani A, Aboumarzouk OM, ElBakry T, Al-Ansari A, Elakkad MS (2021) Robotic inguinal hernia repair: systematic review and meta-analysis. ANZ J Surg. https://doi.org/10.1111/ans.16505
Gamagami R, Dickens E, Gonzalez A et al (2018) Open versus robotic-assisted transabdominal preperitoneal (R-TAPP) inguinal hernia repair: a multicenter matched analysis of clinical outcomes. Hernia 22(5):827–836. https://doi.org/10.1007/s10029-018-1769-1
Balentine CJ, Meier J, Berger M et al (2020) Using local rather than general anesthesia for inguinal hernia repair is associated with shorter operative time and enhanced postoperative recovery. Am J Surg. https://doi.org/10.1016/j.amjsurg.2020.08.024
Patterson TJ, Beck J, Currie PJ, Spence RAJ, Spence G (2019) Meta-analysis of patient-reported outcomes after laparoscopic versus open inguinal hernia repair. Br J Surg 106(7):824–836. https://doi.org/10.1002/bjs.11139
Neumayer L, Giobbie-Hurder A, Jonasson O et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350(18):1819–1827
Millat B, Fédération de Recherche EN CHirurgie (FRENCH) (2007) Inguinal hernia repair. A randomized multicentricstudy comparing laparoscopic and open surgical repair. J Chir (Paris) 144(2):119–124
Funding
No outside funding was received for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to study conception and design. Authors TH, MN, and AS contributed to the acquisition and analysis of data. All authors contributed to the interpretation of data. Authors TH, MN, AS, and FB contributed to drafting of the work while authors MG and JD made critical revisions. All authors read and approved the final manuscript and agree to be accountable for all aspects of work.
Corresponding author
Ethics declarations
Conflict of interest
Timothy Holleran, Michael Napolitano, Andrew Sparks, James Duncan, Meredith Garrett, and Fredrick Brody declare that they have no conflict of interest.
Ethical approval
Due to the retrospective nature of the study and utilization of de-identified data, Institutional Review Board (IRB) waiver of consent was applied and approved for this study (IRB-Exempt Protocol #01966).
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this review, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Holleran, T.J., Napolitano, M.A., Sparks, A.D. et al. Trends and outcomes of open, laparoscopic, and robotic inguinal hernia repair in the veterans affairs system. Hernia 26, 889–899 (2022). https://doi.org/10.1007/s10029-021-02419-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02419-3