Abstract
Purpose
To provide a comparative analysis of short-term outcomes after open, laparoscopic, and robotic-assisted (RAS) ventral incisional hernia (VIH) repairs that include subject-reported pain medication usage and hernia-related quality of life (QOL).
Methods
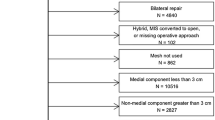
Subjects were ≥ 18 years old and underwent elective open, laparoscopic or RAS VIH repair without myofascial release. Perioperative clinical outcomes through 30 days were analyzed as were prescription pain medication use and subject-reported responses to the HerQLes Abdominal QOL questionnaire. Observed differences in baseline characteristics were controlled using a weighted propensity score analysis to obviate potential selection bias (inverse probability of treatment weighting, IPTW). A p value < 0.05 was considered statistically significant.
Results
Three hundred and seventy-one subjects (RAS, n = 159; open, n = 130; laparoscopic, n = 82) were enrolled in the study across 17 medical institutions within the United States. Operative times were significantly different between the RAS and laparoscopic groups (126.2 vs 57.2, respectively; p < 0.001). Mean length of stay was comparable for RAS vs laparoscopic (1.4 ± 1.0 vs 1.4 ± 1.1, respectively; p = 0.623) and differed for the RAS vs open groups (1.4 ± 1.0 vs 2.0 ± 1.9, respectively; p < 0.001). Conversion rates differed between RAS and laparoscopic groups (0.6% vs 4.9%; p = 0.004). The number of subjects reporting the need to take prescription pain medication through the 2–4 weeks visit differed between RAS vs open (65.2% vs 79.8%; p < 0.001) and RAS vs laparoscopic (65.2% vs 78.75%; p < 0.001). For those taking prescription pain medication, the mean number of pills taken was comparable for RAS vs open (23.3 vs 20.4; p = 0.079) and RAS vs laparoscopic (23.3 vs 23.3; p = 0.786). Times to return to normal activities and to work, complication rates and HerQLes QOL scores were comparable for the RAS vs open and RAS vs laparoscopic groups. The reoperation rate within 30 days post-procedure was comparable for RAS vs laparoscopic (0.6% vs 0%; p = 0.296) and differed for RAS vs open (0.6% vs 3.1%; p = 0.038).
Conclusions
Short-term outcomes indicate that open, laparoscopic, and robotic-assisted approaches are effective surgical approaches to VIH repair; however, each repair technique may demonstrate advantages in terms of clinical outcomes. Observed differences in the RAS vs laparoscopic comparison are longer operative time and lower conversion rate in the RAS group. Observed differences in the RAS vs open comparison are shorter LOS and lower reoperation rate through 30 days in the RAS group. The operative time in the RAS vs open comparison is similar. The number of subjects requiring the use of prescription pain medication favored the RAS group in both comparisons; however, among subjects reporting a need for pain medication, there was no difference in the number of prescription pain medication pills taken. While the study adds to the body of evidence evaluating the open, laparoscopic, and RAS approaches, future controlled studies are needed to better understand pain and QOL outcomes related to incisional hernia repair.
Trial registration
ClinicalTrials.gov identifier: NCT02715622.
Similar content being viewed by others
References
Cassar K, Munro A (2002) Surgical treatment of incisional hernia. Br J Surg 89:534–545
Milbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144:1056–1059
Guzman-Pruneda FA, Huang L-C, Collins C, Renshaw S, Narula V, Poulouse BK (2020) Abdominal core quality of life after ventral hernia repair: a comparison of open versus robotic-assisted retromuscular techniques. Surg Endosc. https://doi.org/10.1007/s00464-020-07386
Borab ZM, Shakir S, Lanni MA, Tecce MG, MacDonald J, Hope WW, Fischer JP (2017) Does prophylactic mesh placement in elective, midline laparotomy reduce the incidence of incisional hernia? A systematic review and meta-analysis. Hernia 161:1149–1163
Holihan JL, Alawadi Z, Martindale RG, Roth JS, Wray CJ, Ko TC, Kao LS, Liang MK (2015) Adverse events after ventral hernia repair: the vicious cycle of complications. J Am Coll Surg 221:478–485
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
DuBay DA, Choi W, Urbanchek MG, Wang X, Adamson B, Dennis RG, Kuzon WM, Franz MG (2007) Incisional herniation induces decreased abdominal wall compliance via oblique muscle atrophy and fibrosis. Ann Surg 245:140–146
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Graaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J (2000) A comparison of suture repair with mesh repair for incision hernia. N Engl J Med 343:392–398
Al Chalabi H, Larkin J, Mehigan B, McCormick P (2015) A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 20:65–74
Prabhu AS, Dickens EO, Copper CM, Mann JW, Yunis JP, Phillips S, Huang LC, Poulose BK, Rosen MJ (2017) Laparoscopic vs robotic intraperitoneal mesh repair for incisional hernia: an Americas Hernia Society Quality Collaborative Analysis. J Am Coll Surg 225(2):285–293. https://doi.org/10.1016/j.amcollsurg.2017.08.007
Krpata DM, Schmotzer BJ, Flocke S, Jin J, Blatnik JA, Ermlich B, Novitsky YW, Rosen MJ (2012) Design and initial implementation of HerQles: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215:635–642
LeBlanc K, Dickens E, Gonzalez A, Gamagami R, Pierce R, Balentine C, Voeller G, for The Prospective Hernia Study Group (2020) Prospective, multicenter, pairwise analysis of robotic-assisted inguinal hernia repair with open and laparoscopic inguinal hernia repair: early results from the Prospective Hernia Study. Hernia. https://doi.org/10.1007/s10029-020-02224-4
LeBlanc KA (2019) Design of a comparative outcome analysis of open, laparoscopic, or robotic-assisted incisional or inguinal hernia repair utilizing surgeon experience and a novel follow-up model. Contemp Clin Trials 86:105853. https://doi.org/10.1016/j.cct.2019.105853
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 34:3661–3679. https://doi.org/10.1002/sim6607
Gavigan T, Stewart T, Matthews B, Reinke C (2018) Patients undergoing parastomal hernia repair using the Americas Hernia Society Quality Collaborative: a prospective cohort study. J Am Coll Surg 227:393–403. https://doi.org/10.1016/j.jamcollsurg.2018.07.658
Warren JA, Love M (2018) Incisional hernia repair: minimally invasive approaches. Surg Clin N Am 98:537–559. https://doi.org/10.1016/j.suc.2018.01.008
Yoo A, Corso K, Chung G, Sheng R, Schmitz N-D (2018) The impact of surgical approach on late recurrence in incisional hernia repair. JSLS 22(e2018):00053. https://doi.org/10.4293/JSLS.2018.00053
LaPinska M, Kleppe K, Webb L, Stewart TG, Olson M, online ahead of print March 31, 2020 (2020) Robotic-assisted and laparoscopic hernia repair: real-world evidence from the Americas Hernia Society Quality Collaborative (AHSQC). Surg Endosc. https://doi.org/10.1007/s00464-020-07511 (online ahead of print March 31, 2020)
Forester B, Attaar M, Donovan K, Kuchta K, Ujiki M, Denham W, Haggarty SP, Carbray J, Linn J, online ahead of print July 27, 2020 (2020) Short-term quality of life comparison of laparoscopic, open, and robotic incisional hernia repairs. Surg Endosc. https://doi.org/10.1007/s00464-020-07711-4 (online ahead of print July 27, 2020)
He C, Lu J, Ong MW, Lee DJK, Tan KY, Chia CLK (2020) Seroma prevention strategies in laparoscopic ventral hernia repair: a systematic review. Hernia 24:717–731. https://doi.org/10.1007/s10029-019-02098-1
Gonzalez A, Escobar E, Romero R, Walker G, Mejias J, Gallas M, Dickens E, Johnson CJ, Rabaza J, Kudsi OY (2017) Robotic-assisted ventral hernia repair: a multicenter evaluation of clinical outcomes. Surg Endosc 31:1342–1349
Olavarria O et al (2020) Robotic versus laparoscopic ventral hernia repair: a multicenter, blinded randomized controlled trial. SSRN Electron J. https://doi.org/10.2139/ssrn.3453330
Chen YJ et al (2016) Outcomes of robot-assisted versus laparoscopic repair of small-sized ventral hernias. Surg Endosc 31(3):1275–1279. https://doi.org/10.1007/s00464-016-5106-4
Pierce RA et al (2006) Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 21(3):378–386. https://doi.org/10.1007/s00464-006-9115-6
Acknowledgements
We thank the participating investigators in the Prospective Hernia Study Group, and their staff for their involvement in this study. We would also like to acknowledge Intuitive Surgical, Inc. for its sponsorship and funding of the study and, specifically, Jennifer Mueller, MS, Monica Shah, MD and Sundeep Master, BS MBA (Intuitive Surgical, Inc.) for their clinical trial operational support; Dongjing Guo, MPH (Intuitive Surgical, Inc.) for statistical analysis; and Mimi Wainwright (Wainwright Medical Communications, Los Gatos, CA) for medical writing support. The members of the Prospective Hernia Study Group are: Courtney Balentine, MD, MPH; Thai Pham, MD FACS; Valerie-Sue Emuakhagbon, MD; Sergio Huerta, MD FACS (Dallas Veterans Affairs, Dallas, TX); Amy Banks-Venegoni, MD; Lora Silverman, MD; David Scheeres, MD; Thomas Martin, MD (Spectrum Health Medical Group, Grand Rapids, MI); Elliott Brill, MD; Jemmy Hwang, MD; Justin Choi, MD; John Stevenson, MD; Jong-Ping Lu, MD; Amid Keshavarzi, MD, FACS; Judith Keddington, MD, FACS; Maureen Tedesco, MD, FACS; Rouzbeh Mostaedi, MD; David Nguyen, MD; Lisa Yang, MD; Albert Im, MD; Jonathan Svahn, MD; Melissa Chu, MD, FACS; Aaron Baggs, MD, FACS (Kaiser Permanente of Northern California, Santa Clara, CA); Eugene Dickens, MD; Michael McGee, MD, FACS (Hillcrest Medical Center, Tulsa, OK); Reza Gamagami, MD, FACS (Progressive Surgical Associates, New Lenox, IL); Anthony Gonzalez, MD, FACS, FASMBS; Jorge Rabaza, MD, FACS; Juan-Carlos Verdeja, MD, FACS (Baptist Health South Florida, Miami, FL); William Hope, MD, FACS (New Hanover Regional Medical Center, Wilmington, NC); Brian Jacob, MD, FACS; Anthony Vine, MD, FACS; Mark Reiner, MD; Brian Katz, MD (Mount Sinai Medical Center, New York, NY); Karl LeBlanc, MD, MBA, FACS, FASMBS; Keith Rhynes, MD, MBA, FACS (Our Lady of the Lake Hospital, Baton Rouge, LA); Adrian Martin, MD, FACS (Southern Illinois Medical Center, Carbondale, IL); Keith Millikan, MD (Rush University Medical Center, Chicago, IL); John Olsofka, MD (Louisville Surgical Associates, Louisville, KY); Carlos Ortiz-Ortiz, MD, FACS; Eduardo Parra-Davila, MD, FACS, FASCRS (Advent Health, Celebration, FL); Richard Pierce, MD, PhD, FACS (Vanderbilt University Medical Center, Nashville, TN); Thomas Swope, MD, FACS; Kelly Alexander, MD; Phuong Nguyen, MD (Mercy Medical Center, Baltimore, MD); Shirin Towfigh, MD, FACS; (Beverly Hills Hernia Center, Beverly Hills, CA); Guy Voeller, MD; Nathaniel Stoikes, MD; David Webb, MD (University of Tennessee, Memphis, TN).
Funding
This study was sponsored and funded by Intuitive Surgical, Inc. (Sunnyvale, CA USA) in association with the study chair under a cooperative clinical trial agreement.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Drs. Dickens, Gonzalez, LeBlanc, Olsofka, Pierce, Ortiz-Ortiz, and Verdeja received clinical research grants from Intuitive Surgical. Drs. Dickens and LeBlanc receive personal fees for consulting and education from Intuitive. Dr. Gonzales receives personal fees for teaching and proctoring from Intuitive. Dr. LeBlanc receives personal fees from Intuitive, personal fees from W.L. Gore & Associates, Inc., personal fees from Davol Inc., non-financial support from Covidien LP, and personal fees from RTI Surgical, Inc., outside of the submitted work. Dr. Ortiz-Ortiz receives personal fees from Medtronic. Drs. Olsofka and Verdeja do not have other conflicts of interest to disclose.
Ethical approval
Ethical approval was agreed by the ethical committee of the institution.
Human and animal rights
The study including human participants has been performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients prior to surgical procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Prospective Hernia Study Group are listed in “Acknowledgements”.
Rights and permissions
About this article
Cite this article
LeBlanc, K.A., Gonzalez, A., Dickens, E. et al. Robotic-assisted, laparoscopic, and open incisional hernia repair: early outcomes from the Prospective Hernia Study. Hernia 25, 1071–1082 (2021). https://doi.org/10.1007/s10029-021-02381-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02381-0