Abstract
Background & aims
Primary aim of this study is to determine whether the use of local anaesthesia performed with IINB and IHNB against spinal anaesthesia in inguinal hernia repair is accepted as an alternative medicine.
Methods
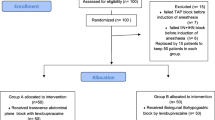
75 cases in the class of American Society of Anesthesia physical status (ASA) I–III between the ages of 18 and 75 diagnosed with single-sided inguinal hernia and hospitalized for surgery in general surgery clinic were prospectively and randomly included in this study.
Results
There was statistically significant difference between the groups (30.14 ± 8.2 and 35.51 ± 9.39) in terms of the duration of the surgery.
The duration was shorter in Group 1 (p < 0.001). There was statistically significant difference between the groups in terms of the duration of the first mobilization. It was significantly shorter in Group 2 than in Group 1 (5.71 ± 1.7 and 2.70 ± 1.53 min) (p < 0.001).
Mean duration of length of hospital stay criteria was significantly shorter in Group 2 than in Group 1 (26.00 ± 6.43 and 14.23 ± 5.40 h) (p < 0.001).
Throughout the follow-up period in postoperative 24 h, the number of patients who needed analgesia was significantly higher in Group 1 than in Group 2 (91.4% and 45.7%)
There was statistically significant difference between the groups in terms of patient satisfaction and urinary retention development (p < 0.005).
Hematoma development or postoperative bleeding was not observed in either group. The time of sensory block onset was significantly higher in Group 2 than in Group 1 (9.66 ± 1.41 and 9.03 ± 0.98 min) (p < 0.005)
Conclusion
The results of our study show that IINB and IHNB applied with local anaesthesia are superior to spinal anaesthesia in unilateral inguinal hernia repairs.



Similar content being viewed by others
References
White PF (2001) Optimizing anesthesia for inguinal herniorrhaphy: general, regional, or local anesthesia? Anesth Analg 93:1367–1369
Subramaniam P, Leslie J, Gourlay C, Clezy J (1998) Inguinal hernia repair: a comparison between local and general anaesthesia. Aust NZ J Surg 68:799–800
Callesen T, Bech K, Kehlet H (1998) The feasibility, safety and cost of infiltration anaesthesia for hernia repair. Anaesthesia 53:31–35
Langesæter E, Dyer RA (2011) Maternal haemodynamic changes during spinal anaesthesia for caesarean section. Curr Opin Anesthesiol 24:242–248
Kaban OG, Yazicioglu D, Akkaya T, Sayin MM, Seker D, Gumus H (2014) Spinal anaesthesia with hyperbaric prilocaine in day-case perianal surgery: randomised controlled trial. Sci World J 2014
O’dwyer PJ, Serpell MG, Millar K, Paterson C, Young D, Hair A, Courtney C-A, Horgan P, Kumar S, Walker A (2003) Local or general anesthesia for open hernia repair: a randomized trial. Ann Surg 237:574
Özgün H, Kurt MN, Kurt I, Çevikel MH (2002) Comparison of local, spinal, and general anaesthesia for inguinal herniorrhaphy. Eur J Surg 168:455–459
Zamani-Ranani MS, Moghaddam N, Firouzian A, Fazli M, Hashemi SA (2015) A comparison between local and spinal anaesthesia in inguinal hernia repair. Int J Clin Anesthesiol 3:1041
Shafique N, Rashid HU, Raja MI, Saeed M (2015) Comparison of efficacy of spinal anaesthesia and sub-fascial local anaesthetic inguinal field block for open inguinal hernia repair-a single institutional experience. J Ayub Med College Abbottabad 27:197–200
Gürkan I, Ütebey G, Özlü O (2013) Comparison of ilioinguinal–iliohypogastric nerve block versus spinal anesthesia techniques for single sided inguinal herniorrhaphy. AĞRI-J Turkish Soc Algol 25:108–114
Santos GdC, Braga GM, Queiroz FL, Navarro TP, Gomez RS (2011) Assessment of postoperative pain and hospital discharge after inguinal and iliohypogastric nerve block for inguinal hernia repair under spinal anesthesia: a prospective study. Revista da Associação Médica Brasileira 57:545–549
Amid PK, Shulman AG, Lichtenstein IL (1994) Local anesthesia for inguinal hernia repair step-by-step procedure. Ann Surg 220:735
Kark AE, Kurzer MN, Belsham PA (1998) Three thousand one hundred seventy-five primary inguinal hernia repairs: advantages of ambulatory open mesh repair using local anesthesia. J Am Coll Surg 186:447–455
Prakash D, Heskin L, Doherty S, Galvin R (2017) Local anaesthesia versus spinal anaesthesia in inguinal hernia repair: A systematic review and meta-analysis. Surgeon 15:47–57
Klein SM, Pietrobon R, Nielsen KC, Steele SM, Warner DS, Moylan JA, Eubanks WS, Greengrass RA (2002) Paravertebral somatic nerve block compared with peripheral nerve blocks for outpatient inguinal herniorrhaphy. Reg Anesth Pain Med 27:476–480
Kulacoglu H, Alptekin A (2011) Current options in local anesthesia for groin hernia repairs. Acta Chir Iugosl 58:25–35
Ramsay M, Savege T, Simpson B, Goodwin R (1974) Controlled sedation with alphaxalone-alphadolone. Br med J 2:656–659
Scott J, Huskisson E (1979) Vertical or horizontal visual analogue scales. Ann Rheum Dis 38:560
Pyati S, Gan TJ (2007) Perioperative pain management. CNS Drugs 21:185–211
Ozkan D, Akkaya T, Comert A, Balkc N, Ozdemir E, Gumus H, Ergul Z, Kaya O (2009) Paravertebral block in inguinal hernia surgeries: two segments or 4 segments? Reg Anesth Pain Med 34:312–315
Metzinger SE, Bailey DJ, Boyce RG, Lyons GD (1992) Local anesthesia in rhinoplasty: a new twist? Ear Nose Throat J 71:405–406
Ball E, Sanjay P, Woodward A (2006) Comparison of buffered and unbuffered local anaesthesia for inguinal hernia repair: a prospective study. Hernia 10:175–178
Daubländer M, Kämmerer PW, Willershausen B, Leckel M, Lauer H-C, Buff S, Rösl B (2012) Clinical use of an epinephrine-reduced (1/400,000) articaine solution in short-time dental routine treatments—a multicenter study. Clin Oral Invest 16:1289–1295
McLure H, Rubin A (2005) Review of local anaesthetic agents. Minerva Anestesiol 71:59–74
El-Emam EM, El Motlb EAA (2019) Ultrasound-guided erector spinae versus ilioinguinal/iliohypogastric block for postoperative analgesia in children undergoing inguinal surgeries. Anesth Essays Res 13:274–279
Kamal K, Jain P, Bansal T, Ahlawat G (2018) A comparative study to evaluate ultrasound-guided transversus abdominis plane block versus ilioinguinal iliohypogastric nerve block for post-operative analgesia in adult patients undergoing inguinal hernia repair. Indian J Anaesth 62:292–297
Gentili M, Huu PC, Enel D, Hollande J, Bonnet F (1998) Sedation depends on the level of sensory block induced by spinal anaesthesia. Br J Anaesth 81:970–971
Yaddanapudi S, Batra Y, Balagopal A, Nagdeve N (2007) Sedation in patients above 60 years of age undergoing urological surgery under spinal anesthesia: Comparison of propofol and midazolam infusions. J Postgrad Med 53:171
Khedkar SM, Bhalerao PM, Yemul-Golhar SR, Kelkar KV (2015) Ultrasound-guided ilioinguinal and iliohypogastric nerve block, a comparison with the conventional technique: an observational study. Saudi J Anaesth 9:293–297
Baloyiannis I, Perivoliotis K, Sarakatsianou C, Tzovaras G (2018) Laparoscopic total extraperitoneal hernia repair under regional anesthesia: a systematic review of the literature. Surg Endosc 32:2184–2192
Pere P, Harju J, Kairaluoma P, Remes V, Turunen P, Rosenberg PH (2016) Randomized comparison of the feasibility of three anesthetic techniques for day-case open inguinal hernia repair. J Clin Anesth 34:166–175
Ozgun H, Kurt MN, Kurt I, Cevikel MH (2002) Comparison of local, spinal, and general anaesthesia for inguinal herniorrhaphy. Eur J Surg 168:455–459
Gurkan I, Utebey G, Ozlu O (2013) Comparison of ilioinguinal–iliohypogastric nerve block versus spinal anesthesia techniques for single sided inguinal herniorrhaphy. Agri 25:108–114
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165
Acknowledgements
No sources of funding were used to conduct this study or prepare this article. The authors have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
They authors declare that they have no conflict of interest.
Ethical approval
This study was performed after institutional review boardapproval (IRB No. 2019–45) in the Human Research Ethics Committee of Erciyes University in Turkey. The research meets the ethical guidelines. The study was also conducted according to the Helsinki Declaration Guidelines.
Human and animal rights
All human rights were observed in keeping with Decleration of Helsinki 2008 (ICH GCP). There are no animal rights issues as this is a clinical study.
Informed consent
Informed consent was obtained from all individuals included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaçmaz, M., Bolat, H. Comparison of spinal anaesthesia versus ilioinguinal–iliohypogastric nerve block applied with tumescent anaesthesia for single-sided inguinal hernia. Hernia 24, 1049–1056 (2020). https://doi.org/10.1007/s10029-020-02163-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02163-0