Abstract
Purpose
Physical examination (PE) combined with ultrasound (US) is recommended to confirm a recurrent hernia. However, the evidence is rather weak. The aim of this study was to evaluate PE and appraise the added value of US in alleged recurrent inguinal hernias after totally extraperitoneal (TEP) inguinal hernia repair.
Methods
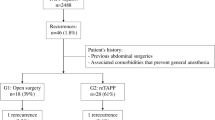
All adult patients who were re-operated for suspicion of a recurrent hernia after a primary unilateral or bilateral TEP between 2006 and 2017 were identified and investigated retrospectively. Patient characteristics, PE, additional imaging and intra-operative findings were registered. PE outcomes were compared with intra-operative findings to calculate the positive predictive value (PPV) of PE. In case of clinical doubt, the added value of US was evaluated by comparing US findings with the intra-operative findings.
Results
A total of 130 patients were re-operated for suspicion of 137 recurrent hernias. In 75 patients, US was performed. PE was positive for an inguinal hernia in 101 groins (73.7%), negative in 30 (21.9%) and inconclusive in 6 (4.4%). PE matched the operative findings in 75.2%. The PPV of diagnosing a recurrent hernia (or lipoma) on PE was 97%. In case of clinical doubt (n = 36), positive US matched the operative findings in 20 cases (87.0%).
Conclusion
US does not necessarily need to be incorporated in the standard diagnostic workup of a recurrent inguinal hernia. After PE alone, a recurrent hernia (or lipoma) can be diagnosed with a PPV of 97%. Only in case of clinical doubt, US has additional value.
Similar content being viewed by others
References
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165. https://doi.org/10.1007/s10029-017-1668-x
Kingsnorth A, Hernias LeBlanc K (2003) Hernias: Inguinal and incisional. Lancet 362:1561–1571. https://doi.org/10.1016/S0140-6736(03)14746-0
Shpitz B, Kuriansky J, Werener M, Osadchi A, Tiomkin V, Bugayev N, Klein E (2004) Early postoperative evaluation of groins after laparoscopic total extraperitoneal repair of inguinal hernias. J Laparoendosc Adv Surg Tech A 14(6):353–357. https://doi.org/10.1089/lap.2004.14.353
Young J, Gilbert AI, Graham MF (2007) The use of ultrasound in the diagnosis of abdominal wall hernias. Hernia 11(4):347–351. https://doi.org/10.1007/s10029-007-0227-2
Roos MM, van Hessen CV, Verleisdonk EJMM, Clevers GJ, Davids PHP, Voorbrood CEH, Simmermacher RKJ, Burgmans JPJ (2018) An 11-year analysis of reoperated groins after endoscopic totally extraperitoneal (TEP) inguinal hernia repair in a high volume hernia center. Hernia. https://doi.org/10.1007/s10029-018-1827-8
Burgmans JP, Voorbrood CE, Simmermacher RK, Schouten N, Smakman N, Clevers G, Davids PH, Verleisdonk EM, Hamaker ME, Lange JF, van Dalen T (2016) Long-term results of a randomized double-blinded prospective trial of a lightweight (Ultrapro) versus a heavyweight mesh (Prolene) in laparoscopic total extraperitoneal inguinal hernia repair (TULP-trial). Ann Surg 263(5):862–866. https://doi.org/10.1097/SLA.0000000000001579
Roos MM, Bakker WJ, Schouten N, Voorbrood CEH, Clevers GJ, Verleisdonk EJMM, Davids PHP, Burgmans JPJ (2018) Higher recurrence rate after endoscopic totally extraperitoneal (TEP) inguinal hernia repair with ultrapro lightweight mesh: 5-year results of a randomized controlled trial (TULP-trial). Ann Surg 268(2):241–246. https://doi.org/10.1097/SLA.0000000000002649
Tonolini M, Ippolito S (2016) Multidetector CT of expected findings and early postoperative complications after current techniques for ventral hernia repair. Insights Imaging 7:541–551. https://doi.org/10.1007/s13244-016-0501-x
Vandersteegen T, Marneffe W, Cleemput I, Vandijck D, Vereeck L (2016) The determinants of defensive medicine practices in Belgium. Health Econ Policy Law 12:363–386. https://doi.org/10.1017/S174413311600030X
Assing Hvidt E, Lykkegaard J, Pedersen LB, Pedersen KM, Munck A, Andersen MK (2017) How is defensive medicine understood and experienced in a primary care setting? A qualitative focus group study among Danish general practitioners. BMJ Open 7(12):e019851. https://doi.org/10.1136/bmjopen-2017-019851
Ertem M, Ozben V, Gok H, Ozveri E (2013) Relaparoscopic treatment of recurrences after previous laparoscopic inguinal hernia repair. Minim Invasive Surg. https://doi.org/10.1155/2013/260131(Article ID 260131)
Sharma A, Sarwal A (2017) Surgical repair in recurrent inguinal hernia. Ann Laparosc Endosc Surg 2:97. https://doi.org/10.21037/ales.2017.05.03
Lacour M, Ridereau Zins C, Casa C, Venara A, Cartier V, Yahya S, Barbieux J, Aubé C (2017) CT findings of complications after abdominal wall repair with prosthetic mesh. Diagn Interv Imaging 98:517–528. https://doi.org/10.1016/j.diii.2017.01.002
Author information
Authors and Affiliations
Contributions
CH: study conception and design, data collection, analysis and interpretation of data, drafting of manuscript. MR: study conception and design, interpretation of data, critical revision. FS: study conception and design, interpretation of data, critical revision EV: study conception and design, critical revision. GC: study conception and design, critical revision. PD: study conception and design, critical revision JB: study conception and design, interpretation of data, critical revision.
Corresponding author
Ethics declarations
Conflict of interest
Coen van Hessen declares no conflict of interest. Marleen Roos declares no conflict of interest. Floris Sanders declares no conflict of interest. Egbert Jan Verleisdonk declares no conflict of interest. Geert Jan Clevers declares no conflict of interest. Paul Davids declares no conflict of interest. Josephina Burgmans declares no conflict of interest.
Ethical approval
This study did not need approval from an ethic committee.
Human and animal rights
This study does not contain any studies with participants or animals performed by any of the authors.
Informed consent
Informed consent was not required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van Hessen, C.V., Roos, M.M., Sanders, F.B.M. et al. Recurrence after totally extraperitoneal (TEP) inguinal hernia repair: the role of physical examination and ultrasound. Hernia 24, 153–157 (2020). https://doi.org/10.1007/s10029-019-02029-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-02029-0