Abstract
Environmental factors are at least as important as genetic factors for the development of obsessive–compulsive symptoms (OCS), but the identification of such factors remain a research priority. Our study aimed to investigate the association between a broad scope of potential risk factors and OCS in a large community cohort of children and adolescents. We evaluated 1877 participants and their caregivers at baseline and after 3 years to assess various demographic, prenatal, perinatal, childhood adversity, and psychopathological factors. Mean age at baseline was 10.2 years (SD 1.9) and mean age at follow-up was 13.4 years (SD 1.9). Reports of OCS at baseline and follow-up were analyzed using latent variable models. At preliminary regression analysis, 15 parameters were significantly associated with higher OCS scores at follow-up. At subsequent regression analysis, we found that eight of these parameters remained significantly associated with higher follow-up OCS scores while being controlled by each other and by baseline OCS scores. The significant predictors of follow-up OCS were: lower socioeconomic status (p = 0.033); lower intelligence quotient (p = 0.013); lower age (p < 0.001); higher maternal stress level during pregnancy (p = 0.028); absence of breastfeeding (p = 0.017); parental baseline OCS (p = 0.038); youth baseline anxiety disorder (p = 0.023); and youth baseline OCS scores (p < 0.001). These findings may better inform clinicians and policymakers engaged in the mental health assessment and prevention in children and adolescents.


Similar content being viewed by others
References
Nestadt G, Samuels J, Riddle MA, Liang KY, Bienvenu OJ, Hoehn-Saric R, Grados M, Cullen B (2001) The relationship between obsessive-compulsive disorder and anxiety and affective disorders: results from the Johns Hopkins OCD Family Study. Psychol Med 31(3):481–487
Tibbo P, Kroetsch M, Chue P, Warneke L (2000) Obsessive-compulsive disorder in schizophrenia. J Psychiatr Res 34(2):139–146
Torres AR, Ramos-Cerqueira AT, Ferrao YA, Fontenelle LF, do Rosario MC, Miguel EC (2011) Suicidality in obsessive-compulsive disorder: prevalence and relation to symptom dimensions and comorbid conditions. J Clin Psychiatry 72(1):17–26. https://doi.org/10.4088/JCP.09m05651blu(quiz 119–120)
Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K, Sceery W, Shaffer D (1988) Obsessive compulsive disorder in adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry 27(6):764–771. https://doi.org/10.1097/00004583-198811000-00018
Subramaniam M, Soh P, Vaingankar JA, Picco L, Chong SA (2013) Quality of life in obsessive-compulsive disorder: impact of the disorder and of treatment. CNS Drugs 27(5):367–383. https://doi.org/10.1007/s40263-013-0056-z
World Health Organization (2008) The global burden of disease: 2004 update. World Health Organization, Geneva
Alvarenga PG, do Rosario MC, Cesar RC, Manfro GG, Moriyama TS, Bloch MH, Shavitt RG, Hoexter MQ, Coughlin CG, Leckman JF, Miguel EC (2016) Obsessive-compulsive symptoms are associated with psychiatric comorbidities, behavioral and clinical problems: a population-based study of Brazilian school children. Eur Child Adolesc Psychiatry 25(2):175–182. https://doi.org/10.1007/s00787-015-0723-3
Saad LO, do Rosario MC, Cesar RC, Batistuzzo MC, Hoexter MQ, Manfro GG, Shavitt RG, Leckman JF, Miguel EC, Alvarenga PG (2017) The child behavior checklist-obsessive-compulsive subscale detects severe psychopathology and behavioral problems among school-aged children. J Child Adolesc Psychopharmacol 27(4):342–348. https://doi.org/10.1089/cap.2016.0125
Barzilay R, Patrick A, Calkins ME, Moore TM, Wolf DH, Benton TD, Leckman JF, Gur RC, Gur RE (2018) Obsessive-compulsive symptomatology in community youth: typical development or a red flag for psychopathology? J Am Acad Child Adolesc Psychiatry. https://doi.org/10.1016/j.jaac.2018.06.038
Mataix-Cols D, Boman M, Monzani B, Ruck C, Serlachius E, Langstrom N, Lichtenstein P (2013) Population-based, multigenerational family clustering study of obsessive-compulsive disorder. JAMA Psychiatry 70(7):709–717. https://doi.org/10.1001/jamapsychiatry.2013.3
Taylor S (2013) Molecular genetics of obsessive-compulsive disorder: a comprehensive meta-analysis of genetic association studies. Molecular Psychiatry 18(7):799–805. https://doi.org/10.1038/mp.2012.76
Fernandez TV, Leckman JF (2016) Prenatal and perinatal risk factors and the promise of birth cohort studies: origins of obsessive-compulsive disorder. JAMA Psychiatry 73(11):1117–1118. https://doi.org/10.1001/jamapsychiatry.2016.2092
Monzani B, Rijsdijk F, Harris J, Mataix-Cols D (2014) The structure of genetic and environmental risk factors for dimensional representations of DSM-5 obsessive-compulsive spectrum disorders. JAMA Psychiatry 71(2):182–189. https://doi.org/10.1001/jamapsychiatry.2013.3524
Brander G, Perez-Vigil A, Larsson H, Mataix-Cols D (2016) Systematic review of environmental risk factors for obsessive-compulsive disorder: a proposed roadmap from association to causation. Neurosci Biobehav Rev 65:36–62. https://doi.org/10.1016/j.neubiorev.2016.03.011
Sampaio AS, Miguel EC, Borcato S, Batistuzzo M, Fossaluza V, Geller DA, Hounie AG (2009) Perinatal risk factors and obsessive-compulsive spectrum disorders in patients with rheumatic fever. Gen Hosp Psychiatry 31(3):288–291. https://doi.org/10.1016/j.genhosppsych.2008.08.003
Geller DA, Wieland N, Carey K, Vivas F, Petty CR, Johnson J, Reichert E, Pauls D, Biederman J (2008) Perinatal factors affecting expression of obsessive compulsive disorder in children and adolescents. J Child Adolesc Psychopharmacol 18(4):373–379. https://doi.org/10.1089/cap.2007.0112
Cath DC, van Grootheest DS, Willemsen G, van Oppen P, Boomsma DI (2008) Environmental factors in obsessive-compulsive behavior: evidence from discordant and concordant monozygotic twins. Behav Genet 38(2):108–120. https://doi.org/10.1007/s10519-007-9185-9
Vasconcelos MS, Sampaio AS, Hounie AG, Akkerman F, Curi M, Lopes AC, Miguel EC (2007) Prenatal, perinatal, and postnatal risk factors in obsessive-compulsive disorder. Biol Psychiat 61(3):301–307. https://doi.org/10.1016/j.biopsych.2006.07.014
Lensi P, Cassano GB, Correddu G, Ravagli S, Kunovac JL, Akiskal HS (1996) Obsessive-compulsive disorder. Familial-developmental history, symptomatology, comorbidity and course with special reference to gender-related differences. Br J Psychiatry 169(1):101–107
Douglass HM, Moffitt TE, Dar R, McGee R, Silva P (1995) Obsessive-compulsive disorder in a birth cohort of 18-year-olds: prevalence and predictors. J Am Acad Child Adolesc Psychiatry 34(11):1424–1431. https://doi.org/10.1097/00004583-199511000-00008
Capstick N, Seldrup J (1977) Obsessional stat es. A study in the relationship between abnormalities occurring at the time of birth and the subsequent development of obsessional symptoms. Acta Psychiatr Scand 56(5):427–431
Brander G, Rydell M, Kuja-Halkola R, Fernandez de la Cruz L, Lichtenstein P, Serlachius E, Ruck C, Almqvist C, D'Onofrio BM, Larsson H, Mataix-Cols D (2016) Association of perinatal risk factors with obsessive-compulsive disorder: a population-based birth cohort, sibling control study. JAMA Psychiatry 73(11):1135–1144. https://doi.org/10.1001/jamapsychiatry.2016.2095
Grisham JR, Fullana MA, Mataix-Cols D, Moffitt TE, Caspi A, Poulton R (2011) Risk factors prospectively associated with adult obsessive-compulsive symptom dimensions and obsessive-compulsive disorder. Psychol Med 41(12):2495–2506. https://doi.org/10.1017/s0033291711000894
Valleni-Basile LA, Garrison CZ, Waller JL, Addy CL, McKeown RE, Jackson KL, Cuffe SP (1996) Incidence of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry 35(7):898–906. https://doi.org/10.1097/00004583-199607000-00015
Geller DA, March J (2012) Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 51(1):98–113. https://doi.org/10.1016/j.jaac.2011.09.019
Alvarenga PG, Cesar RC, Leckman JF, Moriyama TS, Torres AR, Bloch MH, Coughlin CG, Hoexter MQ, Manfro GG, Polanczyk GV, Miguel EC, do Rosario MC (2015) Obsessive-compulsive symptom dimensions in a population-based, cross-sectional sample of school-aged children. J Psychiatr Res 62:108–114. https://doi.org/10.1016/j.jpsychires.2015.01.018
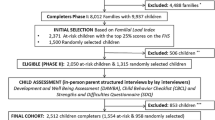
Salum GA, Gadelha A, Pan PM, Moriyama TS, Graeff-Martins AS, Tamanaha AC, Alvarenga P, Valle Krieger F, Fleitlich-Bilyk B, Jackowski A, Sato JR, Brietzke E, Polanczyk GV, Brentani H, de Jesus MJ, Do Rosario MC, Manfro GG, Bressan RA, Mercadante MT, Miguel EC, Rohde LA (2015) High risk cohort study for psychiatric disorders in childhood: rationale, design, methods and preliminary results. Int J Methods Psychiatric Res 24(1):58–73. https://doi.org/10.1002/mpr.1459
Schwab-Stone M, Fallon T, Briggs M, Crowther B (1994) Reliability of diagnostic reporting for children aged 6–11 years: a test-retest study of the diagnostic interview schedule for children-revised. Am J Psychiatry 151(7):1048–1054. https://doi.org/10.1176/ajp.151.7.1048
Goodman R, Ford T, Richards H, Gatward R, Meltzer H (2000) The development and well-being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 41(5):645–655
Achenbach T (1991) Manual for the child behavior checklist/4-18 and 1991 profile. Department of Psychiatry, University of Vermont, Burlington
Bordin IA, Rocha MM, Paula CS, Teixeira MC, Achenbach TM, Rescorla LA, Silvares EF (2013) Child behavior checklist (CBCL), youth self-report (YSR) and teacher's report form (TRF): an overview of the development of the original and Brazilian versions. Cadernos de Saude Publica 29(1):13–28
Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D, Katsovich L, Scahill L, King RA, Woody SR, Tolin D, Hollander E, Kano Y, Leckman JF (2006) The dimensional yale-brown obsessive-compulsive scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry 11(5):495–504. https://doi.org/10.1038/sj.mp.4001798
Victora CG, Horta BL, Loret de Mola C, Quevedo L, Pinheiro RT, Gigante DP, Goncalves H, Barros FC (2015) Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil. Lancet Glob Health 3(4):e199–205. https://doi.org/10.1016/s2214-109x(15)70002-1
Jackson DL, Gillaspy JA, Purc-Stephenson R (2009) Reporting practices in confirmatory factor analysis: an overview and some recommendations. Psychol Methods 14(1):6–23. https://doi.org/10.1037/a0014694
Nelson EC, Hanna GL, Hudziak JJ, Botteron KN, Heath AC, Todd RD (2001) Obsessive-compulsive scale of the child behavior checklist: specificity, sensitivity, and predictive power. Pediatrics 108(1):E14
Loehlin JC (1998) Latent variable models: an introduction to factor, path, and structural analysis, 3rd edn. Lawrence Erlbaum Associates Publishers, Mahwah
DiStefano C, Zhu M, Mindrila D (2009) Understanding and using factor scores: considerations for the applied researcher. Practical Assess Res Evalu 14(20):1–11
Everitt B, Skrondal A (2002) The Cambridge dictionary of statistics, vol 44. University Press Cambridge, Cambridge
Claeskens G, Hjort NL (2008) Model selection and model averaging. Cambridge University Press, Cambridge
Martel MM, Pan PM (2017) A general psychopathology factor (P factor) in children: structural model analysis and external validation through familial risk and child global executive function. J Abnorm Psychol 126(1):137–148. https://doi.org/10.1037/abn0000205
Voltas Moreso N, Hernández-Martínez C, Arija Val V, Canals Sans J (2013) Socio-demographic and psychopathological risk factors in obsessive-compulsive disorder: epidemiologic study of school population. Int J Clin Health Psychol 13(2):118–126. https://doi.org/10.1016/S1697-2600(13)70015-2
Zohar AH, Bruno R (1997) Normative and pathological obsessive-compulsive behavior and ideation in childhood: a question of timing. J Child Psychol Psychiatry 38(8):993–999. https://doi.org/10.1111/j.1469-7610.1997.tb01616.x
Fernandez de la Cruz L, Micali N, Roberts S, Turner C, Nakatani E, Heyman I, Mataix-Cols D (2013) Are the symptoms of obsessive-compulsive disorder temporally stable in children/adolescents? A prospective naturalistic study. Psychiatry Res 209(2):196–201. https://doi.org/10.1016/j.psychres.2012.11.033
Springer KW, Sheridan J, Kuo D, Carnes M (2007) Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse Negl 31(5):517–530. https://doi.org/10.1016/j.chiabu.2007.01.003
Sugaya L, Hasin DS, Olfson M, Lin K-H, Grant BF, Blanco C (2012) Child physical abuse and adult mental health: a national study. J Trauma Stress 25(4):384–392. https://doi.org/10.1002/jts.21719
MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, Duku EK, Walsh CA, Wong MY, Beardslee WR (2001) Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiatry 158(11):1878–1883. https://doi.org/10.1176/appi.ajp.158.11.1878
Markham JA, Koenig JI (2011) Prenatal stress: role in psychotic and depressive diseases. Psychopharmacology 214(1):89–106. https://doi.org/10.1007/s00213-010-2035-0
Schmitt A, Malchow B, Hasan A, Falkai P (2014) The impact of environmental factors in severe psychiatric disorders. Front Neurosci 8:19. https://doi.org/10.3389/fnins.2014.00019
Cunha GR, Asevedo E, Mansur RB, Zugman A, Pan PM, Gadelha A, Belangero SI, Rizzo LB, Coelho R, Stertz L, Cogo-Moreira H, Grassi-Oliveira R, Teixeira AL, Kauer-Sant'Anna M, Mari JJ, Miguel EC, Bressan RA, Brietzke E (2016) Inflammation, neurotrophism and oxidative stress and childhood psychopathology in a large community sample. Acta Psychiatr Scand 133(2):122–132. https://doi.org/10.1111/acps.12453
Mahgoub M, Monteggia LM (2013) Epigenetics and psychiatry. Neurotherapeutics 10(4):734–741. https://doi.org/10.1007/s13311-013-0213-6
Ptak C, Petronis A (2010) Epigenetic approaches to psychiatric disorders. Dialogues Clin Neurosci 12(1):25–35
Taylor S (2011) Etiology of obsessions and compulsions: a meta-analysis and narrative review of twin studies. Clin Psychol Rev 31(8):1361–1372. https://doi.org/10.1016/j.cpr.2011.09.008
Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, Poulton R (2009) Obsessions and compulsions in the community: prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatry 166(3):329–336. https://doi.org/10.1176/appi.ajp.2008.08071006
Diagnostic and statistical manual of mental disorders: DSM-5 (2013). American Psychiatric Association, Arlington. https://nla.gov.au/nla.cat-vn6261708
Geller D, Biederman J, Faraone SV, Frazier J, Coffey BJ, Kim G, Bellordre CA (2000) Clinical correlates of obsessive compulsive disorder in children and adolescents referred to specialized and non-specialized clinical settings. Depress Anxiety 11(4):163–168. https://doi.org/10.1002/1520-6394(2000)11:4<139::AID-DA1>3.0.CO;2-3
Rapp AM, Bergman RL, Piacentini J, McGuire JF (2016) Evidence-based assessment of obsessive-compulsive disorder. J Cent Nerv Syst Dis 8:JCNSD.S38359. https://doi.org/10.4137/JCNSD.S38359
Uher R, Heyman I, Turner CM, Shafran R (2008) Self-, parent-report and interview measures of obsessive-compulsive disorder in children and adolescents. J Anxiety Disord 22(6):979–990. https://doi.org/10.1016/j.janxdis.2007.10.001
Storch EA, Murphy TK, Adkins JW, Lewin AB, Geffken GR, Johns NB, Jann KE, Goodman WK (2006) The children's yale-brown obsessive-compulsive scale: psychometric properties of child- and parent-report formats. J Anxiety Disord 20(8):1055–1070. https://doi.org/10.1016/j.janxdis.2006.01.006
Fontenelle LF, Hasler G (2008) The analytical epidemiology of obsessive–compulsive disorder: risk factors and correlates. Prog Neuropsychopharmacol Biol Psychiatry 32(1):1–15. https://doi.org/10.1016/j.pnpbp.2007.06.024
Acknowledgements
This work was supported by the National Institute of Developmental Psychiatry for Children and Adolescents, a science and technology institute funded by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq; National Council for Scientific and Technological Development; Grant number 573974/2008-0) and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP; Research Support Foundation of the State of São Paulo; Grant numbers 2008/57896-8 and 2015/01587-0). The authors thank the children and families for their participation, which made this research possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Pedro Macul Ferreira de Barros, Natalia Szejko, Natália Polga, Guaraci de Lima Requena, Ana Beatriz Ravagnani Salto, Daniel Fatori, Marcelo Camargo Batistuzzo, Marcelo Queiroz Hoexter, Eurípedes Constantino Miguel and Pedro Gomes de Alvarenga declare no conflicts of interest. Maria Conceição do Rosário has served on the speakers’ bureau of Novartis and Shire, and declares no potential conflicts of interest relating to this research. Luis Augusto Rohde has received grant or research support from, served as a consultant to, and served on the speakers’ bureau of Eli Lilly and Co., Janssen, Medice, Novartis, and Shire. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by Dr. Rohde have received unrestricted educational and research support from the following pharmaceutical companies: Eli Lilly and Co., Janssen, Shire, and Novartis. Dr. Rohde has received travel grants from Shire to take part in the 2018 American Psychological Association annual meeting and from Novartis to take part of the 2016 American Academy of Child and Adolescent Psychiatry annual meeting. He also has received authorship royalties from Oxford Press and ArtMed, and declares no potential conflicts of interest relating to this research. Guilherme Vanoni Polanczyk has served as a consultant or speaker to Shire, Teva, and Medice, has received royalties from Editora Manole, and declares no potential conflicts of interest relating to this research. James Frederick Leckman receives royalties from John Wiley and Sons, McGraw Hill, and Oxford University Press; is on the Advisory Boards for Brain and Behavior Research Foundation and How I Decide; has served as a consultant for Tasly Pharmaceuticals, Inc., and declares no potential conflicts of interest relating to this research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Macul Ferreira de Barros, P., do Rosário, M.C., Szejko, N. et al. Risk factors for obsessive–compulsive symptoms. Follow-up of a community-based youth cohort. Eur Child Adolesc Psychiatry 30, 89–104 (2021). https://doi.org/10.1007/s00787-020-01495-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01495-7