Abstract
Objective
To evaluate the clinical outcomes following extraction of impacted maxillary tooth adjacent to maxillary via submaxillary sinus membrane space approach.
Materials and methods
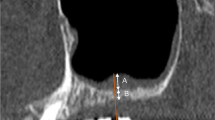
Seventy-two patients were enrolled in our study. The positions of the maxillary impacted tooth were confirmed by cone-beam computed tomography (CBCT). Cases were randomly divided into two groups: the “submaxillary sinus membrane space approach” was applied in the new method (NM) group, and the conventional “avoid maxillary sinus membrane exposure” strategy was executed in the traditional method (TM) group. The clinical and follow-up data were recorded.
Results
The duration of the procedure in the TM group was significantly longer than those in the NM group (P < 0.05). Four teeth were accidentally displaced into the maxillary sinus with MSM perforation. The MSM perforation rate was slightly higher in the TM group than in the NM group, however, without significant difference between the two groups (8/36 vs. 3/36, P = 0.19). The maxillary sinus membrane perforation was associated with the displacement of tooth into the maxillary sinus (OR = 16.2, P = 0.026). The root tip exposure of the adjacent tooth was significantly higher in the TM group than in the NM group (10/36 vs. 1/36, P = 0.006). The incidence of reduced pulp vitality of the adjacent tooth was significantly higher in the TM group (10/36 vs. 1/36, P = 0.006), and it was associated with the exposure of the root tip intraoperatively (OR = 456.5, P < 0.001). The incidence of external root resorption was significantly lower in the NM group, and there was no significant association with the root exposure intraoperatively (OR = 3.7, P = 0.47).
Conclusions
Submaxillary sinus membrane space approach is a safe and efficient approach in extraction of impacted maxillary tooth. It is an alternative way for cases which are in close proximity to the maxillary sinus.
Clinical relevance
A novel method to extract impacted maxillary tooth adjacent to maxillary sinus.

Similar content being viewed by others
References
Komerik N, Muglali M, Tas B, Selcuk U (2014) Difficulty of impacted mandibular third molar tooth removal: predictive ability of senior surgeons and residents. J Oral Maxillofac Surg 72(1062):e1-6. https://doi.org/10.1016/j.joms.2014.01.023
Ma Y, Mu D, Li X (2022) Risk factors for root resorption of second molars with impacted third molars: a meta-analysis of CBCT studies. Acta Odontol Scandinavica:1–11. https://doi.org/10.1080/00016357.2022.2077982
Li D, Tao Y, Cui M, Zhang W, Zhang X, Hu X (2019) External root resorption in maxillary and mandibular second molars associated with impacted third molars: a cone-beam computed tomographic study. Clin Oral Invest 23:4195–4203. https://doi.org/10.1007/s00784-019-02859-3
Rajendra Santosh AB (2020) Odontogenic Cysts. Dent Clin North Am 64:105–119. https://doi.org/10.1016/j.cden.2019.08.002
Jordi C, Mukaddam K, Lambrecht JT, Kühl S (2018) Membrane perforation rate in lateral maxillary sinus floor augmentation using conventional rotating instruments and piezoelectric device-a meta-analysis. Int J Implant Dent 4:3. https://doi.org/10.1186/s40729-017-0114-2
Juzikis E, Gaubys A, Rusilas H (2018) Uses of maxillary sinus lateral wall bony window in an open window sinus lift procedure: literature review. Stomatologija 20:14–21
Starch-Jensen T, Deluiz D, Duch K, Tinoco EMB (2019) Maxillary sinus floor augmentation with or without barrier membrane coverage of the lateral window: a systematic review and meta-analysis. J Oral Maxillofac Res 10:e1. https://doi.org/10.5037/jomr.2019.10401
Testori T, Weinstein T (2000) Taschieri S and Wallace SS (2019) Risk factors in lateral window sinus elevation surgery. Periodontol 81:91–123. https://doi.org/10.1111/prd.12286
Mavriqi L, Lorusso F, Tartaglia G, Inchingolo F, Scarano A (2022) transinusal pathway removal of an impacted third molar with an unusual approach: a case report and a systematic review of the literature. Antibiotics (Basel, Switzerland) 11. https://doi.org/10.3390/antibiotics11050658
Clausen S, Nicholas RG, Likness M (2021) Keratocystic odontogenic tumor associated with impacted molar in the maxillary sinus causing osteomyelitis. South Dakota Med: J South Dakota State Med Assoc 74:102–104
Buyukkurt MC, Omezli MM, Miloglu O (2010) Dentigerous cyst associated with an ectopic tooth in the maxillary sinus: a report of 3 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:67–71. https://doi.org/10.1016/j.tripleo.2009.07.043
Asnani S, Mahindra U, Rudagi BM, Kini Y, Kharkar VR (2012) Dentigerous cyst with an impacted third molar obliterating complete maxillary sinus. Indian J Dental Res: Off Publ Indian Soc Dental Res 23:833–835. https://doi.org/10.4103/0970-9290.111275
Vencio EF, Mota A, de Melo PC, Dias Filho AA (2006) Odontogenic keratocyst in maxillary sinus with invasive behaviour. J Oral pathol Med: Off Publ Int Assoc Oral Pathol Am Acad Oral Pathol 35:249–251. https://doi.org/10.1111/j.1600-0714.2006.00403.x
Yamazaki M, Cheng J, Nomura T, Saito C, Hayashi T, Saku T (2003) Maxillary odontogenic keratocyst with respiratory epithelium: a case report. J Oral Pathol Med : Off Publ Int Assoc Oral Pathol Am Acad Oral Pathol 32:496–498. https://doi.org/10.1034/j.1600-0714.2003.00149.x
Cavalcante RC, Petinati MFP, de Oliveira ER, Bergamaschi IP, Rebelatto NLB, Klüppel L, Scariot R, da Costa DJ (2018) Benign cementoblastoma associated with an impacted third molar inside maxillary sinus. Case Rep Surg 2018:7148479. https://doi.org/10.1155/2018/7148479
Ohki M (2012) Transnasal marsupialization using endoscopic sinus surgery for treatment of keratocystic odontogenic tumor in maxillary sinus. Case Rep Otolaryngol 2012:281402. https://doi.org/10.1155/2012/281402
Singer SR, Mupparapu M, Milles M, Rinaggio J, Pisano D, Quaranta P (2007) Unusually large complex odontoma in maxillary sinus associated with unerupted tooth. Report of case and review of literature. N Y State Dent J 73:51–53
Ojha J, Kossak E, Mangat S, Kossak Z (2015) Recurrent pain and swelling associated with impacted maxillary third molar. THE DIAGNOSIS: squamous cell carcinoma of the maxillary sinus. J Am Dental Assoc (1939) 146:840–4. https://doi.org/10.1016/j.adaj.2015.06.022
Zou R, Qiao Y, Lin Y, Piao Z, Zhao T, Wu Q, Xing L, Zhang J, Ouyang K (2022) Is it necessary to remove bone-impacted teeth? A retrospective study. J Stomatol Oral Maxillofac Surg. https://doi.org/10.1016/j.jormas.2022.10.003
Yesiltepe S, Kılcı G (2022) Evaluation the relationship between the position and impaction level of the impacted maxillary third molar teeth and marginal bone loss, caries and resorption findings of the second molar teeth with CBCT scans. Oral Radiol 38:269–277. https://doi.org/10.1007/s11282-021-00554-2
Baykul T, Doğru H, Yasan H, CinaAksoy M (2006) Clinical impact of ectopic teeth in the maxillary sinus. Auris Nasus Larynx 33:277–281. https://doi.org/10.1016/j.anl.2006.01.004
Sarica I, Derindag G, Kurtuldu E, Naralan ME, Caglayan F (2019) A retrospective study: Do all impacted teeth cause pathology? Niger J Clin Pract 22:527–533. https://doi.org/10.4103/njcp.njcp_563_18
Pang NS, Choi YK, Kim KD, Park W (2011) Autotransplantation of an ectopic impacted premolar with sinus lift and allogenic bone graft. Int Endod J 44:967–975. https://doi.org/10.1111/j.1365-2591.2011.01902.x
Rothamel D, Wahl G, d’Hoedt B, Nentwig GH, Schwarz F, Becker J (2007) Incidence and predictive factors for perforation of the maxillary antrum in operations to remove upper wisdom teeth: prospective multicentre study. Br J Oral Maxillofac Surg 45:387–391. https://doi.org/10.1016/j.bjoms.2006.10.013
Han G, Song C, Lin S, Piao Z (2020) A rare case of nasolacrimal duct partial obstruction after extraction of an impacted maxillary canine. J Oral Maxillofac Surg : Off J Am Assoc Oral Maxillofac Surg 78:350–356. https://doi.org/10.1016/j.joms.2019.10.020
Hernández-Alfaro F, Torradeflot MM, Marti C (2008) Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin Oral Implant Res 19:91–98. https://doi.org/10.1111/j.1600-0501.2007.01372.x
Lim HC, Kim S, Kim DH, Herr Y, Chung JH, Shin SI (2021) Factors affecting maxillary sinus pneumatization following posterior maxillary tooth extraction. J Periodontal Implant Sci 51:285–295. https://doi.org/10.5051/jpis.2007220361
Gu Y, Sun C, Wu D, Zhu Q, Leng D, Zhou Y (2018) Evaluation of the relationship between maxillary posterior teeth and the maxillary sinus floor using cone-beam computed tomography. BMC Oral Health 18:164. https://doi.org/10.1186/s12903-018-0626-z
Becker A, Brix M, Simon E, Devoti JF (2022) Iatrogenic displacement of an impacted third maxillary molar in the parapharyngeal space: a case report. J Stomatol Oral Maxillofac Surg. https://doi.org/10.1016/j.jormas.2022.04.006
Wasfi KH, Wayzani HN, Aoun G, Berberi NA (2021) Maxillary third molar tooth accidentally displaced in buccal space: report of two cases. J Dent (Shiraz, Iran) 22:308–311. https://doi.org/10.30476/dentjods.2020.87280.1250
Mace T, Kahn A, Dechaufour P, Kün-Darbois JD (2020) An extremely rare case of a displaced third molar into the infratemporal fossa associated with a textiloma. J Stomatol Oral Maxillofac Surg 121:746–748. https://doi.org/10.1016/j.jormas.2020.04.004
Primo BT, Stringhini DJ, da Costa DJ, Rebellato NLB, Scariot R (2016) Delayed removal of maxillary third molar displaced into the maxillary sinus. Stomatologija 18:128–132
Kumar A, Srivastava RK, Saxena A, Khanna R, Ali I (2016) Removal of infected maxillary third molar from the infra-temporal fossa by Caldwell Luc procedure - rare case report with literature review. J Clin Diagn Res : JCDR 10:Zd01-zd03. https://doi.org/10.7860/jcdr/2016/17362.8961
Iwai T, Matsui Y, Hirota M, Tohnai I (2012) Endoscopic removal of a maxillary third molar displaced into the maxillary sinus via the socket. J Craniofac Surg 23:e295–e296. https://doi.org/10.1097/SCS.0b013e318252f1cf
Author information
Authors and Affiliations
Contributions
Rui Sun was responsible for drafting the article, collecting the images, the patient’s follow-up, and data analysis. Lin-wei Zheng, Yu-qi Sun, and Ting-ting Li were responsible for the patient’s follow-up and collecting the images. Jian-gang Ren and Ji-hong Zhao were responsible for the study design and patient collection.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study followed the Declaration of Helsinki on medical protocol and ethics and the Regional Ethical Review Board of the Ethics Committee of the Hospital of Stomatology, Wuhan University, approved the study. Informed consent was obtained from all subjects.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, R., Zheng, Lw., Sun, Yq. et al. Is it safe and effective to extract impacted maxillary tooth adjacent to maxillary sinus via submaxillary sinus membrane space approach?—a randomized controlled trial. Clin Oral Invest 27, 6081–6087 (2023). https://doi.org/10.1007/s00784-023-05223-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05223-8