Abstract
Objectives
Evaluate whether there is an association between convergence insufficiency and temporomandibular disorder (TMD) and whether there is an association between pain and range of motion in different degrees of TMD.
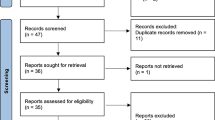
Methods
We evaluated 138 individuals with TMD and 46 without TMD using the Research Diagnostic Criteria for temporomandibular disorders, the Fonseca Anamnestic Index (FAI), Numeric Pain Rating Scale, and the measurement of mandibular range of motion (ROM). Convergence insufficiency was diagnosed using the convergence test and Convergence Insufficiency Symptom Survey. Analysis of variance was used to compare age and mandibular ROM. The Kruskal–Wallis was used to compare mandibular ROM and pain between groups. The chi-square test was used to evaluate associations between TMD subgroups and the FAI, sex, and ocular convergence.
Results
The majority of individuals without TMD did not exhibit convergence insufficiency. The frequency convergence insufficiency was significantly higher among individuals with severe TMD (p < 0.003). Mean pain severity differed between individuals with and without TMD. Mandibular ROM diminished with the increase in TMD severity.
Conclusions
Convergence insufficiency, age, the increase in pain, and the reduction in mandibular range of motion were associated with the degrees of TMD severity. Despite the significant associations between convergence insufficiency and both pain and TMD severity, these variables cannot be indicated as predictive factors due to the low variability in the linear regression analysis.
Clinical relevance
The present findings can assist in decision making regarding the treatment of severe TMD and the evaluation of ocular convergence.
Similar content being viewed by others
References
Gray’s Anatomy: The Anatomical Basis of Clinical Practice. Kindle (2015) de Elsevier
Scheiman M, Rouse MW (2005) Optometric management of learning-related vision problems, 2nd edn. Mosby, New York
Von Noorden GK, Campos EC (2002) Binocular vision and ocular motility: theory and management of strabismus, 6th edn. Mosby, New York
Cunha T, Pinto S, Sargo J, Mendanha L, Lança C, Oliveira M (2013) Insuficiência de convergência e atenção visual: estudo exploratório em estudantes do ensino superior. Saúde Tecnol (9):5–10
Gupta A, Kailwoo SK, Vijayawali (2008) Convergence insufficiency in patients visiting eye OPD with headache. Rev Sci 10(3):135–136
Rowe FJ (2004) Clinical orthoptics. 3rd Edition, Kindle Edition
Tavares C, Nunes AMMF, Nunes AJS, Vaz Pato M, Monteiro PML (2014) Translation and validation of convergence insufficiency symptom survey (CISS) to Portuguese - psychometric results. Arq Bras Oftalmol 77(1):21-4
Goss DA (1995) Ocular accommodation, convergence and fixation disparity: a manual of clinical analysis, 2nd edn. Butterworth-Heinemann, Boston, p 11±2
Zeng C, Shroff H, Shore SE (2011) Cuneate and spinal trigeminal nucleus projections to the cochlear nucleus are differentially associated with vesicular glutamate transporter-2. Neuroscience 176:142–151. https://doi.org/10.1016/j.neuroscience.2010.12.010
Zhou J, Nannapaneni N, Shore S (2007) Vessicular glutamate transporters 1 and 2 are differentially associated with auditory nerve and spinal trigeminal inputs to the cochlear nucleus. J Comp Neurol 500(4):777–787. https://doi.org/10.1002/cne.21208
Shore SE, Vass Z, Wys NL, Altschuler RA (2000) Trigeminal ganglion innervates the auditory brainstem. J Comp Neurol 419(3):271–285. https://doi.org/10.1002/(SICI)1096-9861(20000410)419:3<271::AID-CNE1>3.0.CO;2-M
Riemann R, Reuss S (1999) Nitric oxide synthase in trigeminal ganglion cells projecting to the cochlea of rat and guinea pig. Neuroreport 10(12):2641–2645. https://doi.org/10.1097/00001756-199908200-00037
Bhargava D, Thomas S, Chakravorty N, Dutt A (2014) Trigeminocardiac reflex: a reappraisal with relevance to maxillofacial surgery. J Maxillofac Oral Surg 13(4):373–377. https://doi.org/10.1007/s12663-013-0541-4
Allen LE, Sudesh S, Sandramouli S, Cooper G, McFarlane D, Willshaw HE (1998) The association between the oculocardiac reflex and post-operative vomiting in children undergoing strabismus surgery. Eye (Lond) 12(Pt 2):193–196. https://doi.org/10.1038/eye.1998.46
Imbe H, Dubner R, Ren K (1999) Masseteric inflammation-induced Fos protein expression in the trigeminal interpolaris/caudalis transition zone: contribution of somatosensory-vagal-adrenal integration. Brain Res 845(2):165–175. https://doi.org/10.1016/S0006-8993(99)01913-7
Bereiter DA, Bereiter DF, Ramos M (2002) Vagotomy prevents morphine-induced reduction in Fos-like immunoreactivity in trigeminal spinal nucleus produced after TMJ injury in a sex-dependent manner. Pain 96(1-2):205–213. https://doi.org/10.1016/S0304-3959(01)00450-X
Venugopal S, Hsiao CF, Sonoda T, Wiedau-Pazos M, Chandler SH (2015) Homeostatic dysregulation in membrane properties of masticatory motoneurons compared with oculomotor neurons in a mouse model for amyotrophic lateral sclerosis. J Neurosci 35(2):707–720. https://doi.org/10.1523/JNEUROSCI.1682-14.2015
Ndiaye A, Pinganaud G, VanderWerf F, Buisseret-Delmas C, Buisseret P (2000) Connections between the trigeminal mesencephalic nucleus and the superior colliculus in the rat. Neurosci Lett 294:17–20
Guerra-Seijas MJ, Labandeira Garcia J, Tobio J, Gonzalez F (1993) Neurons located in the trigeminal sensory complex and the lateral pontine tegmentum project to the oculomotor nucleus in the rabbit. Brain Res 601(1-2):1–13. https://doi.org/10.1016/0006-8993(93)91689-P
Manni E, Draicchio F, Pettorossi VE et al (1989) On the nature of the afferent fibers of oculomotor nerve. Arch Ital Biol 127(2):99–108
Milani RS, De Periere DD et al (1998) Relationship between dental occlusion and visual focusing. J Craniomandib Pract 16:109–118
Monaco et al (2003) Convergence defects in patients with temporomandibular disorders. J Craniomandibular Pract 21:190–195. https://doi.org/10.1080/08869634.2003.11746250
Mcneill C (1993) Epidemiology Temporomandibular disorders: guidelines for classification, assessment and management. Quintessence Publishing Company, Carol Stream, pp 19–22
Leresche L (1997) Epidemiology of tempororomandibular disorders: implications for the investigations of etiologic factors. Crit Rev Oral Biol Med Off Publ Am Assoc Oral Biol 8:291–305
Armijo-Olivo S, Pitance L, Singh V, Neto F, Thie N, Michelotti A (2016) Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: sistematic review and meta-analysis. Phys Ther 96(1):9–25
Manfredini D, Guarda-Nardini L, Wincour E et al (2011) Research diagnostic criteria for temporomandibular disorderes: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112(4):453–462
Fonseca DM (1992) Disfunção Craniomandibular (DCM): diagnóstico pela anamnese [Dissertação de Mestrado]. Faculdade de Odontologia de Bauru da USP, Bauru
Dworkin SF, Leresche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Temporomandib Disord 6(4):300–355
Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach RK, Truelove EL, John MT, Schiffman EL (2009) Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 107(6):844-60
Look JO, Schiffman EL, Truelove EL (2010) Reliability and validity of axis I of the research diagnostic criteria for temporomandibular disorders (RDC/TMD) with proposed revisions. J Oral Rehabil 37(10):744e759
Fonseca DM, Bonfate G, Valle AL et al (1994) Diagnóstico pela anamnese da disfunção craniomandibular. Rev Gaúcha Odontol 42(1):23e28
Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, Terwee CB (2019) Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low Back pain: a systematic review. J Pain 20(3):245–263
Gomes CAFP, Politti F, Gonzalez TO, Hage YE, Arruda EEC, Amaral AP, Biasotto-Gonzalez DA (2012) Analysis of associations between the vertical extension of mandibular movement and different types of temporomandibular disorder. Clin Exp Med Lett 53:37–41
Cuccia AM, Caradonna C (2008) Binocular motility system and temporomandibular joint internal derangement: a study in adults. Am J Orthod Dentofac Orthop 133:640.e15–640.e20
Borsting E, Rouse MW, Mitchel GL, Scheiman M, Cotter SA, Cooper J, Kulp MT, London R (2004) Coonverge insufficiency treatment trial group. Validity and reliability of the revised convergence insufficiency symptom survey in children aged 9 to 18 years. Optom Vis Sci.80(12):832-8. Optom Vis Sci 81(7):489 author reply 489-90
Menigite NC, Tagliette M (2017) Visual symptoms and convergence insufficiency in university teachers. Rev Bras Oftalmol 76(5):242–246. https://doi.org/10.5935/0034-7280.20170050
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Routledge, Hillsdale
Kim HY (2017) Statistical notes for clinical researchers: chi-squared test and Fisher’s exact test. Restor Dent Endod 42(2):152–155
Berni KCS, Dibai-Filho AV, Rodrigues-Bigaton D (2014) Accuracy of Fonseca anamnestic index in the identification of myogenous temporomandibular disorder in female community cases. J Bodyw Mov Ther 19(3):404–409
Bevilaqua-Grossi D, Chaves TC, De Oliveira AS, Monteiro-Pedro V (2006) Anamnestic index severity and signs and symptoms of TMD. Cranio. 24(2):112–118
Dym H, Israel H (2012) Diagnosis and treatment of temporomandibular disorders. Dent Clin Noth Am 56(1):149–161
Pedroni CR, Oliveira AS, Guaratini MI (2003) Prevalence study of signs and symptoms of temporomandibular disorders in university students. J Oral Rehabil 30(3):283–289
Lipton JA, Ship JA, Larach-Robinson S (1993) Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc 124(10):115–121
Rauch A, Schierz O, Körner A, Kiess W, Hirsch C (2020) Prevalence of anamnestic symptoms and clinical signs of temporomandibular disorders in adolescents — results of the epidemiologic LIFE child study. J Oral Rehabil 47:425–431. https://doi.org/10.1111/joor.12926
Berger M, Szalewski L, Bakalczuk M (2015) Association between estrogen levels and temporomandibular disorders: a systematic literature review. Prz Menopauzanlny 14(4):260–270
Wadhwa S, Kapila S (2008) TMJ disorders: future innovations in diagnostics and therapeutics. J Dent Educ 72(8):930–947
Ferreira CLP, Silva MAMR, Felicio CM (2016) Signs and symptoms of temporomandibular disorders in women and men. CoDAS. 28(1):17–21
Herpich CM, Gomes CAFP, Dibai-Filho AV, Politti F, Souza CS, Biasotto-Gonzalez DA (2018) Correlation between severity of temporomandibular disorder, pain intensity, and pressure pain threshold. J Manip Physiol Ther 41:47–51
Christidis N, Kang I, Cairns BE, Kumar U, Dong X, Rosen A et al (2014) Expression of 5-HT3 receptors and TTX resistant sodium channels (Na(V)1.8) on muscle nerve fibers in pain-free humans and patients with chronic myofascial temporomandibular disorders. J Headache Pain 15:63-2377-15-63
Ojima K, Watanabe N, Narita N, Narita M (2007) Temporomandibular disorder is associated with a serotonin transporter gene polymorphism in the Japanese population. Biopsychosoc Med 1:3
Miller VJ, Karic VV, Ofec R, Nehete SR, Smidt A (2014) The temporomandibular opening index, report of headache and TMD, and implications for screening in general practice: an initial study. Quintessence Int 45(7):605–612
Bianchini EMG (1998) Mastigação e ATM. In: Marchesan IQ (ed) Fundamentos em fonoaudiologia: Aspectos clínicos da motricidade oral. Guanabara Koogan, Rio de Janeiro, pp 37–49
Karkazis HC, Kossioni AE (1998) Surface EMG activity of the masseter muscle in denture wearers during chewing of hard and soft food. J Oral Rehabil. Jan 25(1):8–14
Vanegas GAM, Rubio AMG, Osorio LJP (1996) Effects of unilateral mastication on the stomatognathic system and possible predisposing factors in schoolchildren from Medellin. Rev Fac Odontol Univ Antioq 8(1):41–52
Acknowledgments
The authors are grateful to Nove de Julho University, represented by Dean Prof. Eduardo Esterópoli, Director João Carlos Ferrari of the Rehabilitation Sciences and all study participants.
Funding
The work was supported by the Department of Postgraduate Program in Rehabilitation Sciences, Universidade Nove de Julho—UNINOVE.
Author information
Authors and Affiliations
Contributions
Douglas Meira dos Santos: data collection and analysis, critical revision, and final approval of the manuscript. Ludmila Menezes Alves de Azevedo: screening of participants. Rita de Cássia das Neves Martins: screening of participants. Felipe Cunha Ricci: screening of participants. Kelly Sayuri Yun Masuda: data collection. Erika Maria Muramoto do Nascimento: data collection. Cid Andre Fidelis de Paula Gomes: conception and design and final approval of the manuscript. Fabiano Politti: data analysis. Itana Lisane Spinato: data analysis. Daniela Aparecida Biasotto-Gonzalez: conception and design, statistical analysis, manuscript writing, and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Douglas Meira dos Santos declares that he has no conflict of interest. Fabiano Politti declares that he has no conflict of interest. Ludmila Menezes Alves de Azevedo declares that she has no conflict of interest. Rita de Cássia das Neves Martins declares that she has no conflict of interest. Felipe Cunha Ricci declares that he has no conflict of interest. Kelly Sayuri Yun Masuda declares that he has no conflict of interest. Erika Maria Muramoto do Nascimento declares that he has no conflict of interest. Itana Lisane Spinato declares that she has no conflict of interest. Cid Andre Fidelis de Paula Gomes declares that he has no conflict of interest. Daniela Aparecida Biasotto-Gonzalez declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance Resolution number 466/12 of the Brazilian National Board of Health and received approval from the ethics committee of Nove de Julho University (certificate number 12416319.9.0000.5511).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
dos Santos, D.M., Politti, F., de Azevedo, L.M.A. et al. Association between convergence insufficiency and temporomandibular disorder cross-sectional study. Clin Oral Invest 25, 851–858 (2021). https://doi.org/10.1007/s00784-020-03372-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03372-8