Abstract
Objectives
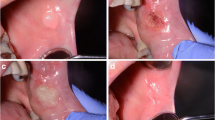
To compare the efficacy and safety of diode laser and electrocautery techniques for inflammatory fibrous hyperplasia (IFH) removal.
Materials and methods
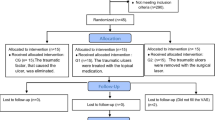
In this randomized double-blind clinical trial, 40 individuals were randomly allocated to two groups: group 1 (G1) consisted of 20 individuals assigned to treatment with diode laser and group 2 (G2) consisted of 20 individuals assigned to treatment with electrocautery. The following transoperative parameters were evaluated: bleeding, temperature, and surgical technique parameters (energy deposited on tissue, flow rate, and time of incision). The postoperative parameters evaluated were as follows: pain, functional alterations (chewing, speaking), analgesic medication intake, swelling, healing of the wound area, and patient satisfaction.
Results
Among the 40 individuals included in the study, four (two in G1 and two in G2) did not complete the entire follow-up. Therefore, 36 individuals (18 in G1 and 18 in G2) participated. Participants in G1 and in G2 had similar demographic characteristics. No difference regarding the trans- or postoperative parameters evaluated was observed between G1 and G2 (p > 0.05). Also, no difference regarding the time for healing was observed between groups.
Conclusions
Diode laser seems to be as effective and safe as electrocautery when applied under similar conditions for IFH removal.
Clinical relevance
IFH corresponds to 65% of the lesions observed in denture wearers. This study shows that under similar conditions diode laser is as effective and safe as electrocautery for removal of IFH.






Similar content being viewed by others
References
Işeri U, Ozçakir-Tomruk C, Gürsoy-Mert H (2009) Treatment of epulis fissuratum with CO2 laser and prosthetic rehabilitation in patients with vesiculobullous disease. Photomed Laser Surg 27:675–681
Amaral MB, de Ávila JM, Abreu MH, Mesquita RA (2015) Diode laser surgery versus scalpel surgery in the treatment of fibrous hyperplasia: a randomized clinical trial. Int J Oral Maxillofac Surg 44:1383–1389
Corbet EF, Holmgren CJ, Phillipsen HP (1994) Oral mucosal lesions in 65-74-year-old Hong Kong Chinese. Community Dent Oral Epidemiol 22:392–395
Canger EM, Celenk P, Kayipmaz S (2009) Denture-related hyperplasia: a clinical study of a Turkish population group. Braz Dent J 20:243–248
Dhanuthai K, Rojanawatsirivej S, Somkotra T, Shin HI, Hong SP, Darling M, Ledderhof N, Khalili M, Thosaporn W, Rattana-Arpha P, Saku T (2016) Geriatric oral lesions: a multicentric study. Geriatr Gerontol Int 16:237–243
Silva LP, Leite RB, Sobral APV, Arruda JA, Oliveira LV, Noronha MS, Kato CO, Mesquita RA, Schuch LF, Gomes APN, Vasconcelos ACU, Souza LB (2017) Oral and maxillofacial lesions diagnosed in older people of a Brazilian population: a multicentric study. J Am Geriatr Soc 65:1586–1590
Corrêa L, Frigerio ML, Sousa SC, Novelli MD (2006) Oral lesions in elderly population: a biopsy survey using 2250 histopathological records. Gerodontology 23:48–54
de Oliveira HC, Tschoeke A, da Cruz GC, Noronha L, de Moraes RS, Mesquita RA, de Aguiar MC, Caldeira PC, de Oliveira RM, Grégio AM, Alanis LR, Ignácio SA, Dos Santos JN, de Lima AA, Johann AC (2016) MMP-1 and MMP-8 expression in giant-cell fibroma and inflammatory fibrous hyperplasia. Pathol Res Pract 212:1108–1112
Gambino A, Carbone M, Broccoletti R, Carcieri P, Conrotto D, Carrozzo M, Arduino PG (2017) A report on the clinical-pathological correlations of 788 gingival lesions. Med Oral Patol Oral Cir Bucal 22:686–693
Macedo Firoozmand L, Dias Almeida J, Guimarães Cabral LA (2005) Study of denture-induced fibrous hyperplasia cases diagnosed from 1979 to 2001. Quintessence Int 36:825–829
Freitas JB, Gomez RS, De Abreu MH, Ferreira E, Ferreira E (2008) Relationship between the use of full dentures and mucosal alterations among elderly Brazilians. J Oral Rehabil 35:370–374
Mozzati M, Mortellaro C, Gallesio G, Ruggiero T, Pol R (2015) Surgical treatment of denture-induced fibrous hyperplasia with plasma rich in growth factors. J Craniofac Surg 26:772–775
Keng SB, Loh HS (1992) The treatment of epulis fissuratum of the oral cavity by CO 2 laser surgery. J Clin Laser Med Surg 10:303–306
Goharkhay K, Moritz A, Wilder-Smith P, Schoop U, Kluger W, Jakolitsch S, Sperr W (1999) Effects on oral soft tissue produced by a diode laser in vitro. Lasers Surg Med 25:401–406
Niccoli-Filho W, Neves ACC, Penna LAP, Seraidarian PI, Riva R (1999) Removal of epulis fissuratum associated to vestibuloplasty with carbon dioxide laser. Lasers Med Sci 14:203–206
Romanos G, Nentwig GH (1999) Diode laser (980 nm) in oral and maxillofacial surgical procedures: clinical observations based on clinical applications. J Clin Laser Med Surg 17:193–197
Fornaini C, Rocca JP, Bertrand MF, Merigo E, Nammour S, Vescovi P (2007) Nd:YAG and diode laser in the surgical management of soft tissues related to orthodontic treatment. Photomed Laser Surg 25:381–392
Angiero F, Parma L, Crippa R, Benedicenti S (2012) Diode laser (808 nm) applied to oral soft tissue lesions: a retrospective study to assess histopathological diagnosis and evaluate physical damage. Lasers Med Sci 27:383–388
Hunter JG (1991) Laser or electrocautery for laparoscopic cholecystectomy? Am J Surg 161:345–349
Hunter JG (1993) Exposure, dissection, and laser versus electrosurgery in laparoscopic cholecystectomy. Am J Surg 165:492–496
Wenig BL, Stenson KM, Wenig BM, Tracey D (1993) Effects of plume produced by the Nd:YAG laser and electrocautery on the respiratory system. Lasers Surg Med 13:242–245
Baeder FM, Santos MT, Pelino JE, Duarte DA, Genovese WJ (2012) High-power diode laser versus electrocautery surgery on human papillomavirus lesion treatment. J Craniofac Surg 23:702–705
Liboon J, Funkhouser W, Terris DJ (1997) A comparison of mucosal incisions made by scalpel, CO2 laser, electrocautery, and constant-voltage electrocautery. Otolaryngol Head Neck Surg 116:379–385
Taheri A, Mansoori P, Sandoval LF, Feldman SR, Pearce D, Williford PM (2014) Electrosurgery: part II. Technology, applications, and safety of electrosurgical devices. J Am Acad Dermatol 70:607.1–607.12 quiz 619–620
Taheri A, Mansoori P, Sandoval LF, Feldman SR, Pearce D, Williford PM (2014) Electrosurgery: part I. Basics and principles. J Am Acad Dermatol 70:591.e1–591.14 quiz 605–606
Rappaport WD, Hunter GC, Allen R, Lick S, Halldorsson A, Chvapil T, Holcomb M, Chvapil M (1990) Effect of electrocautery on wound healing in midline laparotomy incisions. Am J Surg 160:618–620
Schulz KF, Altman DG, Moher D, CONSORT Group (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med 7:1000251
Dunié-Mérigot A, Bouvy B, Poncet C (2010) Comparative use of CO2 laser, diode laser and monopolar electrocautery for resection of the soft palate in dogs with brachycephalic airway obstructive syndrome. Vet Rec 167:700–704
Flick SN (1988) Managing attrition in clinical research. Clin Psychol Rev 8:499–515
Cassidy EL, Baird E, Sheikh JI (2001) Recruitment and retention of elderly patients in clinical trials: issues and strategies. Am J Geriatr Psychiatry 9:136–140
Zweben A, Fucito LM, O'Malley SS (2009) Effective strategies for maintaining research participation in clinical trials. Drug Inf J 43:459–467
El-Kholey KE (2014) Efficacy and safety of a diode laser in second-stage implant surgery: a comparative study. Int J Oral Maxillofac Surg 43:633–638
Mannion AF, Balagué F, Pellisé F, Cedraschi C (2007) Pain measurement in patients with low back pain. Nat Clin Pract Rheumatol 3:610–618
Breytenbach HS (1978) Objective measurement of post-operative swelling. Int J Oral Surg 7:386–392
Peñarrocha M, Carrillo C, Boronat A, Martí E (2007) Level of satisfaction in patients with maxillary full-arch fixed prostheses: zygomatic versus conventional implants. Int J Oral Maxillofac Implants 22:769–773
Petersen PE, Bourgeois D, Bratthall D, Ogawa H (2005) Oral health information systems--towards measuring progress in oral health promotion and disease prevention. Bull World Health Organ 83:686–693
Felton D, Cooper L, Duqum I, Minsley G, Guckes A, Haug S, Meredith P, Solie C, Avery D, Deal Chandler N, American College of Prosthodontists (2011) Evidence-based guidelines for the care and maintenance of complete dentures: a publication of the American College of Prosthodontists. J Prosthodont 20(Suppl 1):S1–S12
MacEntee MI (1985) The prevalence of edentulism and diseases related to dentures--a literature review. J Oral Rehabil 12:195–207
Suter VG, Altermatt HJ, Bornstein MM (2017) A randomized controlled clinical and histopathological trial comparing excisional biopsies of oral fibrous hyperplasias using CO2 and Er:YAG laser. Lasers Med Sci 32:573–581
Murphy MA, Maze NM, Boyd JL, Quick DC, Buss DD (1999) Cost-benefit comparison: holmium laser versus electrocautery in arthroscopic acromioplasty. J Shoulder Elb Surg 8:275–278
Asnaashari M, Zadsirjan S (2014) Application of laser in oral surgery. J Lasers Med Sci 5:97–107
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Augustovski F, Briggs AH, Mauskopf J, Loder E, CHEERS Task Force (2013) Consolidated health economic evaluation reporting standards (CHEERS) statement. Int J Technol Assess Health Care 29:117–122
Acknowledgments
This article was supported by the Brazilian National Council for Scientific and Technological Development (CNPq). RAM and LGA are research fellows at CNPq (#305493/2018-3, #455644/2018-1). The participation of Prof. Dr. Márcio B. F. do Amaral with patient care is greatly appreciated. The authors thank the Coordination for the Improvement of Higher Education Personnel (Finance Code 001). JAAA is the recipient of a scholarship. Mrs. E. Greene provided the English editing of the manuscript.
Funding
This study was supported by the Brazilian National Council for Scientific and Technological Development (#305493/2018–3, #455644/2018–1), Brazil, and by the Coordination for the Improvement of Higher Education Personnel (Finance Code 001), Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Jesus, A.O., Matias, M.D.P., de Arruda, J.A.A. et al. Diode laser surgery versus electrocautery in the treatment of inflammatory fibrous hyperplasia: a randomized double-blind clinical trial. Clin Oral Invest 24, 4325–4334 (2020). https://doi.org/10.1007/s00784-020-03296-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03296-3